Your guide to coumadin(r)/warfarin therapy


Your Guide to
Coumadin®/Warfarin
Therapy
This booklet is based on a product developed by Carla
Huber, A.R.N.P., M.S., Cedar Rapids Community
Anticoagulation Clinic, Cedar Rapids, Iowa, under Agency
for Healthcare Research and Quality (AHRQ) Grant No.
1 U18 HSO15830-01 to Kirkwood Community College.
This document is in the public domain and may be used and
reprinted without special permission. Citation of the source is
What Coumadin®/Warfarin is and What it
How to Take Coumadin®/Warfarin.5
Possible Side Effects .7
Stay Safe While Taking Coumadin®/Warfarin.9
Use of Other Medications .11
Diet for Coumadin®/Warfarin Users .14
Share Information With Your Other Doctors.16
Specific Conditions .17
Atrial Fibrillation .17
Deep Vein Thrombosis.17
Heart Valve Replacement .18
Peripheral Vascular Disease.18
Pregnancy and Breastfeeding.19
Pulmonary Embolism.20
Valvular Heart Disease .21
Introduction
Your doctor, nurse, or other health professional
has started you on the medication
Coumadin®/warfarin. Patients who are on
Coumadin®/warfarin must be watched closely. You
will need to have blood drawn often. You will also
need to be careful that you do not do something
to hurt yourself and cause bleeding. Your doctor
will work with you to keep you healthy and safe
while you are taking Coumadin®/warfarin.
Starting on a new medicine, especially one you
may have to take for a long period of time, may
make you worry. To help you learn about your
medication, your doctor has given you this
booklet to take home and read. The information
in the booklet will help you understand why you
are taking Coumadin®/warfarin and how to keep
yourself healthy. Please take time to read all of the
information in the booklet. If you have any
questions call your doctor.
n Your doctor is here to help you.
Call if you have questions.
n Your doctor's phone number is:

You can stay healthy even when you have a health
problem that needs special medication. You and
your doctor will work together as a team to make
sure that taking a medication like
Coumadin®/warfarin does not stop you from
living well and safely.
What Coumadin®/Warfarin is
And What it Does for You
If your blood is too thick
and forms clots, you
could be at risk for heart
attack, stroke, and other
problems. Coumadin®/
warfarin is a medicine
that will keep your blood
from clotting. The drug
is an anticoagulant.
"Anti" means against
and "coagulant" means
to thicken into a gel or solid. Sometimes this drug
is called a blood thinner. Think of syrup being
poured—it is sticky and thick and flows slowly.
Coumadin®/warfarin helps your blood flow easier
Coumadin®/warfarin will:
n Keep your blood from making clots.
n Help your blood flow easily.
How to Take
Coumadin®/Warfarin
Always take your pills as directed. You must take the
pills only on the days your doctor tells you to. The
amount of Coumadin®/warfarin each person needs
is different. The dose is based on a blood test called
the INR (International Normalized Ratio). The
amount of medication you take may change, based
on the blood test. It needs to be taken at the same
time, usually in the evening.
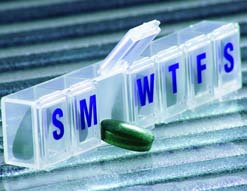
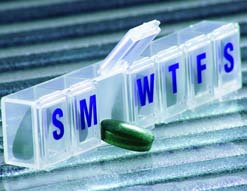
Coumadin®/warfarin can be
medications. Never skip a
dose and never take a double
dose. If you miss a dose,
take it as soon as you
remember. If you don't
remember until the next day, please call your doctor
for instructions. If this happens on a weekend or
holiday, skip the missed dose and start again the
next day. Mark the missing dose in a diary. A daily
pillbox will help you keep track of your dose.
n Go for blood tests as directed.
n Never skip a dose.
n Never take a double dose.
n Take Coumadin®/warfarin in the evening at
the same time as directed by your doctor.
Blood Tests
The doctor decides how much
Coumadin®/warfarin you need by testing your
blood. The test measures how fast your blood is
clotting and lets the doctor know if your dosage
should change. If your blood test is too high, you
might be at risk for bleeding problems. If it is too
low, you might be at risk for forming clots. Your
doctor has decided on a range on the blood test
that is right for you.
Coumadin®/ warfarin
is like balancing a
scale. If you take too
increase bleeding; if you take too little, your
blood will clot. Getting your blood within the
target range is getting it balanced.
When you first start taking Coumadin®/warfarin
you may have your blood checked often. Once
the blood test is in the target range and the
correct dose is reached, this test is done less often.
Because your dose is based on the INR blood test
it is very important that you get your blood tested
on the date and at the time that you are told.
Illness can affect your INR blood test and your
Coumadin®/warfarin dose. If you become sick
with a fever, the flu, or an infection, call your
doctor. Also call if you have diarrhea and vomiting
lasting more than 1 day.

Know your INR blood test range.
n My INR blood test range is:
Possible Side Effects
Side effects with Coumadin®/warfarin may
happen. Most side effects relate to how the
medicine works. To lower the risk of bleeding,
your blood Coumadin®/warfarin level will be kept
within a range that is right for you. Even when
your INR blood test is in range, you might see a
little bleeding like bruises on your body or slight
gum bleeding when you brush your teeth. Some
people may experience hair
loss or skin rashes, but this is
rare. If you notice
something wrong that you
feel may be caused by your
medication, call your doctor.
Slight bleeding—you may notice from time to
Gum bleeding while brushing teeth.
Easy bruising.
Bleeding after a minor cut that stops within
a few minutes.
Menstrual bleeding that is a little heavier
than normal.
Major bleeding—call your doctor, or go to
the hospital emergency room right away if
you have any of the following:
Red, dark, coffee, or cola colored urine.
Bowel movements that are red or look
Bleeding from the gums or nose that does
not stop quickly.
Vomit that is coffee colored or bright red.
Anything red in color that you cough up.
Severe pain, such as a headache or
Sudden appearance of bruises for no
Menstrual bleeding that is much heavier
than normal.
A cut that will not stop bleeding within 10
A serious fall or hit on the head.
Dizziness or weakness.
Stay Safe While Taking
Coumadin®/Warfarin
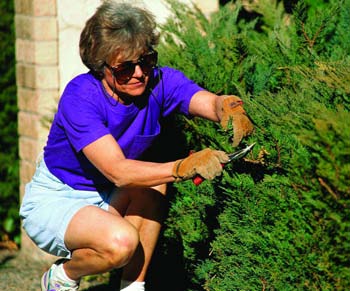
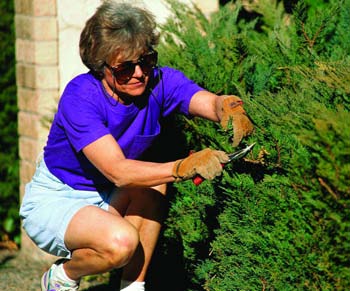
You will need to be careful using objects, such as
knives and scissors, that could make you bleed.
You will need to avoid some activities and sports
that could cause injury. For example, it is not a
good idea to take
them, you need to think about how you can
protect yourself from injury. For example, if you
like to work in the yard, be sure to wear sturdy
shoes and gloves. Activities that would be safe for
you include swimming and walking.
It is very important to know that you can be
bleeding and not see any blood. For example, you
could fall and hit your head, and bleeding could
occur under your skull. Or, you could fall and
hurt your arm and notice a large purple bruise.
This would be bleeding under the skin. Call your
doctor or go to the hospital immediately if
you have taken a bad fall, even if you are not

Talk to your doctor about
wearing a medical alert
bracelet or necklace. If you
are badly injured and
unable to speak, the
bracelet would tell health care workers that you
are on Coumadin®/warfarin.
Stay active.
Exercise is important to your health.
Think about the sports and activities youlike doing. Do they put you at risk forinjury? If so, try another activity and useprotective gear to keep you safe while
you are doing it. For example, if you liketo ride your bike, be sure you wear ahelmet and gloves. If you would like tostart a new activity that will increase theamount of exercise you get every day,talk to your doctor.
To prevent injury; be careful:
Be very careful using knives and scissors.
Use an electric razor.
Use a soft toothbrush.
Use waxed dental floss.
Do not use toothpicks.
Wear shoes or non-skid slippers in the
Take care trimming your toenails.
Do not trim corns or calluses yourself.
Always wear shoes.
Be very careful with sharp tools; wear
gloves when using them.
Avoid activities and sports that can easily
Wear gardening gloves when doing yard
Stay active.
Use of Other Medications
When Coumadin®/warfarin is taken with other
medicines, it can change the way other medicines
work. Other medicines can also change the way
Coumadin®/warfarin works. It is very important
to talk with your doctor about all of the other
medicines that you are taking, including over-
the-counter medicines, antibiotics, vitamins,
or herbal products.
Any product containing aspirin may lessen the
blood's ability to form clots and may harm you
when you take Coumadin®/warfarin. If you take
a daily aspirin, talk with your doctor about
what dose it right for you.
Other medicines you get over-the-counter may have
aspirin in them. All medications must be approved
by your doctor, including medicines you have taken
before you started Coumadin®/warfarin. Following
is a list of some common medications that should
be approved by your doctor.
Pain relievers, such as:
Naproxen (Aleve®).
Ibuprofen (Advil®, Motrin®, Nuprin®,
Midol®, Pamprin HB®).
Stomach remedies, such as:
Cimetidine (Tagamet HB®).
Bismuth Subsalicylate (Pepto Bismol®).
Laxatives and stool softeners.
Herbal products, such as:

Check the Coumadin®/
warfarin you are taking.
Does the medicine seem
different from what
your doctor wrote on
the prescription or look
different from what you
expected? Does your
refill look different than
what you used before? Is the color the same as
what you were previously given? If something
seems different, ask the pharmacist to double-
check it. Most errors are first found by patients.
Medicines look different: Coumadin® pills (upper row)
and generic warfarin (lower row)
Check your medicine.
Always tell your doctor about all themedicines you are taking. Tell yourdoctor when you start taking newmedicine and when you stop. Bring alist of current medications, over-the-counter drugs—such as aspirin—andany vitamins and herbal products youtake.
Diet for Coumadin®/Warfarin
Users
The foods you eat can affect how well
Coumadin®/warfarin works for you. The most
important thing to remember is to eat what you
normally eat and not make any major changes in
your diet without calling your doctor. Do not go
on a weight loss plan while taking
Coumadin®/warfarin.
Vitamin K is important for blood to clot. Since
Coumadin®/warfarin works to keep blood from
clotting, high amounts of vitamin K might work
against Coumadin®/warfarin. The highest amount
of vitamin K is found in green and leafy vegetables
like broccoli, lettuce, cabbage, and spinach. It is
important not to change your vitamin K intake.
Keep your diet the same. If you normally eat a
salad for lunch, keep eating a salad for lunch.
Call your doctor if you are unable to eat for
several days, for whatever reason. Also call if you
have stomach problems, vomiting, or diarrhea
that lasts more than 1 day. These problems could
affect your Coumadin®/warfarin dosage.
Foods high in vitamin K:
Vegetables, such as:
Brussels sprouts.
Green onions.
Leafy greens, such as:
Turnip, collard, and
mustard greens.
Soybean oil.
Limit alcohol. Alcohol can affect your
Coumadin®/warfarin dosage but it does not mean
you must avoid all alcohol. Serious problems can
occur with alcohol and Coumadin®/warfarin when
you drink more than 2 drinks a day or when you
change your usual pattern. Binge drinking is not
good for you. Be careful on special occasions or
holidays and drink only what you usually would
on any regular day of the week.
Share Information With Your
Other Doctors
warfarin you will
be seen regularly
regularly to keep
yourself healthy.
other doctors it is
that you tell them
Coumadin®/warfarin. It is a good idea to bring
this booklet with you to your appointments. You
should also tell your dentist and the person who
cleans your teeth. If another doctor orders a new
medication for you, please call the doctor who
ordered your Coumadin®/warfarin so it can be
noted in your file.
Atrial fibrillation. Atrial fibrillation is a fairly
common heart disorder. Sometimes your heart
will beat too fast or out of rhythm and may cause
Decreases the chance of blood clots.
Helps the blood flow easier.
Deep vein thrombosis. Deep vein thrombosis
(DVT) is a blood clot that has formed in a vein.
The veins deep inside your leg, especially the calf
and thigh, are the most common areas to find the
clot. DVT can lead to damage of the blood vessels
in your leg. It can also cause a serious lung
problem. If the clot in the vein breaks away from
the wall of the vein and travels to the lungs, it can
block blood flow to the lungs. This problem is
called a pulmonary embolism.
Decreases the chance of blood clots in the
veins of your legs.
Lowers your risk for DVT.
Heart attack. A heart attack is caused by a lack of
blood supply to the heart. The lack of blood
happens when one or more of the blood vessels
pumping blood to the heart are blocked.
Decreases the chance of blood clots.
Helps blood flow easier.
Heart valve replacement. There are many types
of artificial valves that are used to replace your
own heart valve. The material used to make these
valves may cause blood to stick and form clots.
Taking Coumadin®/warfarin lowers the chance of
blood clots around the valve.
Decreases the chance of blood clots.
Peripheral vascular disease. Peripheral vascular
disease is the buildup of plaque in the blood
vessels in your legs. Plaque is a fatty buildup that
makes your blood vessels smaller. This buildup of
plaque reduces the flow of blood and increases
the chance of blood clots.
Helps blood flow easier through the
smaller blood vessels.
Decreases blood clots.
Pregnancy and breastfeeding.
Doctors warn against takingCoumadin®/warfarin if you are pregnantor planning to get pregnant. Coumadin®/warfarin may cause birth defects orbleeding that may harm or even lead tothe death of your unborn child.
If you are pregnant or
planning to get pregnant,
tell your doctor. If you are
pregnant and your doctor
wants you to take
Coumadin®/warfarin, you
must be watched closely
by the doctor who
Coumadin®/warfarin and
the doctor who is caring
for you while you are
If you are planning to breastfeed your baby or are
already breastfeeding, talk to your doctor. Your
doctor may need to test you and your baby for
the effects of Coumadin®/warfarin.
Pulmonary embolism. Pulmonary embolism is a
serious health problem. In pulmonary embolism,
a blood clot that formed in another part of your
body, such as in your leg, breaks loose and moves
through the blood to your lungs. The clot then
gets stuck within a blood vessel that brings blood
to the lungs. The clot blocks the blood vessel so
your lungs do not get blood flow. If the lungs
cannot get enough blood, they will be damaged,
and you will have difficulty breathing.
Decreases the chance of blood clots.
Lowers your risk of pulmonary embolism.
Stroke. A stroke is sometimes called a brain
attack. The cause of most strokes is a blood clot
that blocks a blood vessel in the brain. This
blockage cuts off the blood flow to a part of the
brain. When the brain does not get enough blood
flow, the brain cells begin to die and brain
damage can happen. Think about a hose attached
to a sprinkler for watering your lawn in the heat
of summer. If there is a blockage in the hose, the
water will not come out of the sprinkler. After a
stroke, the type of problems the patient has
depends on what part of the brain got blocked
and did not get blood flow.
Decreases the chance of blood clots in the
blood vessels of your brain.
Lowers your risk for a stroke.
Valvular heart disease. Valvular heart disease is
any problem in one or more of the four valves in
the heart. Heart valves keep blood flowing in one
direction. They act as a door that swings open
allowing blood to flow through the sections of
the heart. The valve or door tightly shuts to
prevent blood from backing up to where it came
from. Valves can become thick, stiff, and narrow.
This makes it hard for blood to get through the
door. Valves can become floppy, just like a door
that doesn't shut tightly, and blood leaks
backward. When heart valves are not working like
they should, blood flow can become slowed and
clots can form.
Lowers the chance of blood clots.
Helps blood flow easier.
U.S. Department of
Health and Human Services
Public Health ServiceAgency for Healthcare Research and Quality540 Gaither RoadRockville, MD 20850
AHRQ Pub. No. 08-0028-AFebruary 2008
Source: http://02221ed.netsolhost.com/natt_publications/coumadin.pdf
religión o creencia para todos Libertad de Religión o Creencia: Por qué, Qué y Cómo "Toda persona tiene el derecho a la libertad de pensamiento, conciencia y religión; este derecho incluye la libertad de cambiar de religión o de creencia, así como la libertad de manifestar su religión o su creencia individual y colectivamente, tanto en público como en privado, por la enseñanza, la práctica, el culto y la observancia".
Copyright 2007 by the American Psychological Association 2007, Vol. 7, No. 4, 745–754 Functional Magnetic Resonance Imaging Responses Relate to Differences in Real-World Social Experience Naomi I. Eisenberger, Shelly L. Gable, and Matthew D. Lieberman University of California, Los Angeles Although neuroimaging techniques have proven powerful in assessing neural responses, little is knownabout whether scanner-based neural activity relates to real-world psychological experience. A jointfunctional magnetic resonance imaging (fMRI)/experience-sampling study investigated whether individ-ual differences in neurocognitive reactivity to scanner-based social rejection related to: (a) moment-to-moment feelings of social rejection during real-world social interactions ("momentary social distress")and (b) the extent to which these momentary feelings corresponded with end-of-day global assessmentsof social disconnection ("end-of-day social disconnection"). Individuals who showed greater activity inregions associated with affective and pain processing (dorsal anterior cingulate cortex, amygdala,periaqueductal gray) during scanner-based social rejection reported feeling greater momentary socialdistress during their daily social interactions. In contrast, individuals who showed greater activity inregions associated with memory and self-referential memory encoding (hippocampus, medial prefrontalcortex) showed a stronger correspondence between momentary social distress and end-of-day socialdisconnection, such that greater momentary social distress was associated with greater end-of-day socialdisconnection. These findings complement previous work showing a dissociation between momentaryand retrospective reports of affect and suggest that these processes rely on dissociable neural systems.