Fatigue fractures séminaire radio-clinique 08/01/2013
Colloque de médecine du sport et de l'appareil locomoteur Libramont
Medial tibial stress
syndromes chez le coureur
Dr Prist Vincent
Médecine Physique et Réadaptation
VIVALIA - Libramont
Medial tibial stress syndrome (MTSS) is an overuse injury or repetitive-stress injury of the shin area.
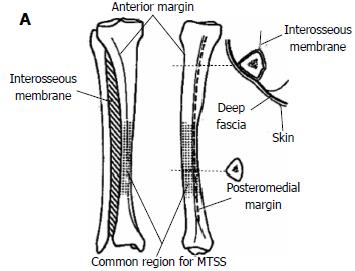
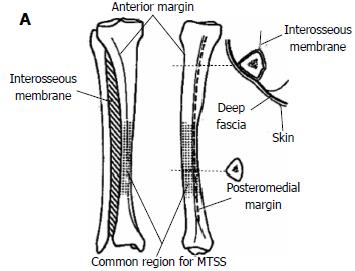
(A) Anterior and medial views of the tibia with the main features shown, with the larger insert demonstrating the deep fascial attachments.
S. Mubarak et al (1982). The medial tibial stress syndrome: a cause of shin splints. American Journal of Sports Medicine, 10, 4, 201-205. R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133. Oakes BW. Tibial pain or shin soreness ("shin splints")-its cause, differential diagnosis and management. In: Draper J, editor. Second Report on the National Sports Research Program. Canberra, Australia: Australian Sports Commission; 1986: 47-51
Three types exist and may coexist:
tibial microfracture, bone stress reaction or cortical fracture
periostalgia from chronic avulsion of the periosteum at the periosteal-fascial junction
chronic compartment syndrome syndrome
Detmer DE. Chronic shin splints. Classification and management of medial tibial stress syndrome. Sports Med. 1986 Nov-Dec;3(6):436-46. Oakes BW. Tibial pain or shin soreness ("shin splints")-its cause, differential diagnosis and management. In: Draper J, editor. Second Report on the National Sports Research Program. Canberra, Australia: Australian Sports Commission; 1986: 47-51
Fractures de stress du
tibia et des métatarsiens
Etiology and Pathophysiology
Most common locations for stress fractures Risk Factors
Intrinsic factors
Extrinsic factors
History Physical examination Imagery
Differential diagnosis
Prognosis and Complications
Complications Prognosis
Treatment Recommendations for Stress Fractures
Conservative therapy Surgery Prevention
Stress fracture
A stress fracture occurs when a bone breaks after being subjected to repeated
tensile or compressive stresses, none of which would be large enough individually
to cause the bone to fail.
From an etiologic standpoint, two types of stress fractures are encountered: fatigue fractures and insufficiency fractures.
Fatigue fracture
A fatigue fracture is caused by the application of abnormal muscular stress or
torque to a bone that has normal elastic resistance.
Devas MB. Stress fractures. London: Churchill Uvingstone, 1975 Daffner RH. Stress fractures: current concepts. Skeletal Radiol 1978;2:221-229. Matheson GO, Clement DB, Mckenzie DC, Taunton JE, Lloyd-Smith DR, Maclntyre JG. Stress fractures in athletes: a study of 320 cases. Am J Sports Med 1987:15:46-58. Wilson ES, Katz FN. Stress fractures: an analysis of 250 consecutive cases. Radiology 1969;92:481-486.
Insufficiency fracture
An insufficiency fracture occurs when the mechanical strength of a bone is reduced to the point that a stress, which would not fracture a healthy bone, breaks the weak one.
The condition that causes reduced bone strength typically does so throughout the skeleton (eg, osteoporosis, osteomalacia, or osteogenesis imperfecta), but may be more localized (eg, demineralization in a limb due to disuse).
Pentecost AL, Murray RA, Brindley HH. Fatigue, insufficiency, and pathologic fractures. JAMA 1964;187:1001-1004
Etiology and Pathophysiology:
Wollf's law
In most activities of daily living, when
the force is removed, the bone elastically rebounds to its original position.
The force that a bone can endure and
still rebound back to its original state
without damage is within the elastic
range. (A1 to A2)
Forces that exceed a critical level
above the elastic range are in the
plastic range. (B)
Once forces reach the plastic range, a
lower load causes greater
deformation, permanent deformity
occurs as the result of microfractures
within the bone (C); it is at this level
that forces summate to permanently
damage the bone. (D)
Richard H. Daffner and Helene Pavlov. Stress Fractures: Current Concepts. AJR 159:245-252, August 1992.
Etiology and Pathophysiology:
Two competing, but not mutually exclusive, theories may explain the
development of stress fractures
Remodeling theory holds that during the initial increase in exercise activity, the skeleton
experiences repetitive loading in its role of providing internal support to counteract the force of
gravity and in forming levers for motion.
This damage is a natural phenomenon and is typically of little consequence as bone is capable
of self-repair through targeted remodelling.
Determinants of damage formation in bone include the magnitude and rate of introduction of
applied loads, and the absolute number of loading cycles.
Damage is threshold related, such that strain magnitudes above a certain level result in its
formation. Influencing the damage formation is the rate at which the strain is introduced.
Strains that are introduced over shorter periods result in considerably greater damage formation.
The interaction between strain magnitude and rate ultimately reduces the number of loading cycles a bone can withstand before fatigue failure.
During this initial increase in exercise activity period, osteoblastic activity lags behind
osteoclastic activity by a few weeks, resulting in a period during which bone is more susceptible
to accumulate damages.
Etiology and Pathophysiology:
Two competing, but not mutually exclusive, theories may explain the
development of stress fractures
Muscular imbalance theory emphasizes bone as a dynamic architectural substance that
responds to changes in the muscular activity imposed on it.
Increased muscular activity results in an increase in the strength of both muscles and bone. Conversely, a decrease in activity or muscular atrophy results in muscular and bony atrophy.
Under normal circumstances, the muscles tone up at a faster rate than the bones do.
Strong and repetitive stress on bone at the insertion point of muscles may provoque focal
bending stresses beyond the ability of the bone to tolerate.
Fatigue of opposing muscle groups that usually prevent one group of muscles from having an
overexerting effect on the bone may result in a further imbalance and lead to bone failure
Etiology and Pathophysiology:
Additional factors contribute to the increased muscular pull, producing overload on stressed
bones
poor posture, typically causes a change in the center of gravity for which the body
compensates. This increases the effect of direct muscular pull and also leads to fatigue of
opposing muscle groups.
the operating conditions in which the activity is practiced.
To a runner, changes in terrain, running surface, or equipment can cause a change or
an increase in muscular pull on the bones of the leg.
Changing from a grass surface to a hard surface may lead to protective curling of
the feet to cushion the footfall.
Running up or down a hill increases the forces by a factor of seven.
Devas MB. Stress fractures. London: Churchill Uvingstone, 1975 Daffner RH, Martinez 5, Gehweiler JA Jr, Harrelson JM. Stress fractures of the proximal tibia in runners. Radiology 1982;1 42 :63-65
Etiology and Pathophysiology:
Example of crack initiation in bone From Nalla RK, Kinney JH, Ritchie RO. Letters: mechanisistic fracture criteria for the faillure of human cortical bone. Nat Mater 2003;2:164-8.
Epidemiology: most common
locations for stress fractures
tibia: 23.6%
navicular: 17.6%
metatarsal: 16.2%
fibula: 15.5%
femur: 6.6%
pelvis: 1.6%
spine: 0.6%
Brukner P, Bradshaw C, Khan KM, White S, Crossley K. Stress fractures: a review of 180 cases. Clin J Sport Med. 1996;6(2):85-89. Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sport Med.1987;15(1):46-58.
Epidemiology: Intrinsic Risk Factors
potentially modifiable
Low bone turnover rate
Decreased thickness of cortical bone
potentially modifiable
Lower limb malalignment
potentially modifiable
Height - Tall stature
Muscle fatigue/poor overall conditioning
modifiable
Weakness/strength imbalance
modifiable
Pathologic bone states
potentially unmodifiable
Menstrual/hormonal irregularities
potentially modifiable
Genetic predisposition
Previous stress fracture - approximately 60% of persons unmodifiable
Epidemiology: Extrinsic Risk Factors
Excessive volume or intensity of training
modifiable
Sporting discipline
modifiable
Change in training regimen - "New coach" phenomenon potentially modifiable
Rapid increase in physical training program
modifiable
Excessive physical activity with limited rest periods modifiable
Poor preparticipation physical condition
modifiable
Change in training surface: irregular or angled surfaces modifiable
Change in density or topography in training surface modifiable
Worn-out training shoes
modifiable
Inappropriate footwear
modifiable
Cigarette smoking
modifiable
Inadequate nutrition including dieting, calcium, vitamin D
modifiable
Medication usage: ex: long-term steroid use
potentially modifiable
Epidemiology: Extrinsic Risk Factors
Training regimen
Surveys report that up to 86% of injured athletes could identify some change in their
training prior to a stress fracture.
Goldberg B, Pecora C. Stress fractures: a risk of increased training in freshman. Phys Sportsmed 1994;22:68–78. Sullivan D, Warren RF, Pavlov H, et al. Stress fractures in 51 runners. Clin Orthop 1984;187:188–92.
Multiple studies in runners have demonstrated that higher weekly running mileage
correlates with an increased incidence of stress fractures and overall running injuries:
0,7 FF / 1000 h of training (Bennet et al., 1996).
Recreational runners who average more than 64 km per week are at increased risk
of stress fractures
Brunet ME, Cook SD, Brinker MR, et al. A survey of running injuries in 1505 competitive and recreational runners. J Sports Med Phys Fitness 1990;30(3):307-15. Macera CA, Pate RR, Powell KE, et al. Predicting lower-extremity injuries among habitual runners. Arch Intern Med 1989;149(11):2565–8. Marti B, Vader JP, Minder CE, et al. On the epidemiology of running injuries: the 1984 Bern Grand-Prix study. Am J Sports Med 1988;16(3):285–94. Walter SD, Hart LE, McIntosh JM, et al. The Ontario cohort study of running-related injuries. Arch Intern Med 1989;149(11):2561–4
Epidemiology: Extrinsic Risk Factors
Equipment factors: shoes
Shoe age has been shown to be a better indicator of shock-absorbing quality than shoe cost.
Military recruits who started training in shoes older than 6 months (an indicator of possible
reduced shock absorptive capacity) were at a greater risk of developing a stress fracture.
Frey C. Footwear and stress fractures. Clin Sports Med 1997;16(2):249–57. Wong PL, Chamari K, Mao de W, et al. Higher plantar pressure on the medial side in four soccer-related movements. Br J Sports Med 2007;41:93–100. Gardner LI, Dziados JE, Jones BH, et al. Prevention of lower extremity stress fractures: a controlled trial of a shock absorbing insole. Am J Public Health 1988;78:1563–7.
Epidemiology: Intrinsic Risk Factors
In athletic populations, most studies have found that women have a higher incidence of stress fractures compared with men.
FF exposure risk / 1000 h of training: 0,86 for women / 0,54 for men
In the United States military, the risk of stress fractures in female recruits undergoing
the same training program as men is up to 10 times higher.
Niva MH, Mattila VM, Kiuru MJ, Pihlajamäki HK. Bone stress injuries are common in female military trainees: a preliminary study. Clin Orthop Relat Res. 2009;467(11):2962-2969. Nattiv A, Armsey Jr TD. Stress injury to bone in the female athlete. Clin Sports Med 1997;16(2):197–224.
This higher incidence is secondary at least in part to gender-associated risk factors such as
dietary deficiencies
menstrual irregularities
lower BMD
narrower bone width
neuromuscular control (women have a slower rate of force development in the muscle
rg B, Pecora C. Stress fractures: a risk of increased training in freshman. Phys Sportsmed 1994;22:68–78.
Bell DG, Jacobs I. Electro-mechanical response times and rate of force development in males and females. Med Sci Sports Exerc 1986;18(1):31–6. Hakkinen K. Force production characteristics of leg extensor, trunk flexor and extensor muscles in male and female basketball players. J Sports Med Phys Fitness 1991;31(3): 325–31. Winter EM, Brookes FB. Electromechanical response times and muscle elasticity in men and women. Eur J Appl Physiol 1991;63(2):124–8. Johnson AW, Weiss Jr CB, Wheeler DL. Stress fractures of the femoral shaft in athletes: more common than expected: a new clinical test. Am J Sports Med 1994;22(2):248–56. Zernicke RF, McNitt-Gray J, Otis C, et al. Stress fracture risk assessment among elite collegiate women runners. J Biomech 1994;27:854.
Diagnosis: History
The patient must be questioned closely about the sequence of events leading to the sudden onset of pain in the affected limb
Stress fracture should be suspected in persons with a drastic recent increase in
physical activity or repeated excessive activity with limited rest
Even conditioned professional athletes may have stress fractures when they have
broken training or decided to increase the amount of effort involved in performing
their particular athletic feat
Many middle-aged and elderly persons are now engaged in this activity, a fact that
accounts for the increasing number of insufficiency-type stress fractures that are
encountered.
Recreational walking is a low-impact activity with excellent aerobic cardiovascular effects.
Diagnosis: History
Pain is a common presenting symptom that can vary by location, such as knee
pain with a proximal tibial injury, hip pain with a femoral neck injury, or groin pain with a pelvic fracture
Early on, the pain typically is mild and occurs toward the end of the inciting
activity (81%)
Subsequently, the pain may worsen and occur earlier, limiting participation in
sports activities
While rest may provide transient relief of symptoms in the early stages, as the
stress injury progresses, the athlete's pain may persist even after cessation of activity
Night pain is a frequent complaint.
H, Mattila VM, Kiuru MJ, Pihlajamäki HK. Bone stress injuries are common in female military trainees: a preliminary study. Clin Orthop Relat Res. 2009;467(11):2962-
t DB, Ammann W, Taunton JE, et al. Exercise-induced stress injuries to the femur. Int J Sports Med. 1993;14(6):347 352.
Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23(4):472-481
Diagnosis: Physical examination
Individuals with stress fractures typically report pain, demonstrate focal tenderness
(65.9% to 100%) upon palpation or percussion of the affected area.
Inspection of the site may reveal localized swelling (18% to 44%) and possibly,
erythema.
Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sports Med.
1987;15(1):46-58.
Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new
magnetic resonance imaging grading system. Am J Sports Med. 1995;23(4):472-481.
Ishibashi Y, Okamura Y, Otsuka H, Nishizawa K, Sasaki T, Toh S. Comparison of scintigraphy and magnetic resonance imaging for stress injuries of bone.
Clin J Sport Med. 2002;12(2):79-84.

Diagnosis: Physical examination
The hop test
single leg hopping produces severe localized pain
is often used and cited in texts as a diagnostic test for lower extremity fractures
no recent literature was found to validate its accuracy
In some studies, a positive hop test was an inclusion criterion or a common finding (70% to
100%) in patients with presumed stress fractures, but was also noted in nearly one-half
(45.6%) of patients with suspected medial tibial stress syndrome (shin splints).
n GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987;15(1):46-
Clement DB, Ammann W, Taunton JE, et al. Exercise-induced stress injuries to the femur. Int J Sports Med. 1993;14(6):347 352. Ishibashi Y, Okamura Y, Otsuka H, Nishizawa K, Sasaki T, Toh S. Comparison of scintigraphy and magnetic resonance imaging for stress injuries of bone. Clin J Sport Med. 2002;1
E, Ugalde V, Anderson MW, Shelton DK. A prospective controlled study of diagnostic imaging for acute shin splints. Med Sci Sports Exerc. 1998;30(11):1564-1571.
D et al . Utilization of Modified NFL Combine Testing to Identify Functional Deficits in Athletes Following ACL Reconstruction. J Orthop Sports Phys The
Diagnosis: Physical examination
The tuning fork test
applying a vibrating tuning fork to the fracture site to produce focal pain
One small study found that the tuning fork test had a sensitivity of 75%, a specificity of
67%, a positive predictive value of 77%, and a negative predictive value of 63% for tibial
stress fractures.
r P, Bennell K, Matheson G. Stress Fractures. 1st ed. Melbourne, Australia: Blackwell Science Asia; 1999.
Lesho EP. Can tuning forks replace bone scans for identification of tibial stress fractures? Mil Med. 1997;162(12):802-803 Schneiders AG, Sullivan SJ, Hendrick PA, Hones BD, McMaster AR, Sugden BA, Tomlinson C. The ability of clinical tests to diagnose stress fractures: a systematic review and meta analysis. J Orthop Sports Phys Ther. 2012 Sep;42(9):760-71.
Diagnosis: Physical examination
No single physical examination test is sufficiently sensitive and specific to permit
the unequivocal diagnosis of a stress fracture
Schneiders AG, Sullivan SJ, Hendrick PA, Hones BD, McMaster AR, Sugden BA, Tomlinson C. The ability of clinical tests to diagnose stress fractures: a systematic review and meta analysis. J Orthop Sports Phys Ther. 2012 Sep;42(9):760-71.
As part of a thorough physical examination, the practitioner should assess
the athlete's flexibility
lower limb alignment including leg lengths
foot structure: pes cavus vs pes planus
motor function: evaluating for strength imbalances
Diagnosis: Imagery
Deepak S. Patel, Matt Roth, Neha Kapil. Stress Fractures: Diagnosis, Treatment, and Prevention. American Family Physician Volume 83, Number 1, January 1, 2011.


Diagnosis: Imagery of Metatarsal
Radiographie du pied gauche de face montant une fracture de la tête du 2° métatarsien
Diagnosis: Imagery of Metatarsal
Diagnosis: Imagery of Tibia shaft
Diagnosis: Imagery of proximal Tibia
Diagnosis: Imagery of proximal Tibia
Deepak S. Patel, Matt Roth, Neha Kapil. Stress Fractures: Diagnosis, Treatment, and Prevention. American Family Physician Volume 83, Number 1, January 1, 2011.
Differential diagnosis:
If any possibility exists that a bone lesion may represent a healing stress fracture, biopsy should be avoided unless evidence is clear-cut that the appearance of the lesion on radiographs has not changed over several weeks
A biopsy specimen of a stress fracture may contain immature bone cells, which are part of the healing fracture process but which may be misinterpreted by an inexperienced pathologist as representing a bone sarcoma
Fayad LM, Kamel IR, Kawamoto S, Bluemke DA, Frassica FJ, Fishman EK. Distinguishing stress fractures from pathologic fractures: a multimodality approach. Skeletal Radiol. 2005;34(5):245-259
Differential diagnosis: tibia
compartment syndrome
nerve or artery entrapment syndrome
medial tibial stress syndrome
chronic sclerosing osteomyelitis of Garré
osteogenic sarcoma
Deepak S. Patel, Matt Roth, Neha Kapil. Stress Fractures: Diagnosis, Treatment, and Prevention. American Family Physician Volume 83, Number 1, January 1, 2011.
Differential diagnosis: foot
Metatarsophalangeal synovitis
Avascular necrosis of metatarsal head
Inflammatory arthritis
Deepak S. Patel, Matt Roth, Neha Kapil. Stress Fractures: Diagnosis, Treatment, and Prevention. American Family Physician Volume 83, Number 1, January 1, 2011.
Concern about complications is warranted when stress fractures are displaced or do not demonstrate adequate healing, despite time and appropriate interventions
Stress fractures may lead to complications:
progression to complete fractures
development of avascular necrosis
delays in healing or non-union
posttraumatic arthrosis
persistent disabling pain
Kaeding CC, Yu JR, Wright R, Amendola A, Spindler KP. Management and return to play of stress fractures. Clin J Sport Med. 2005;15(6):442-447 Entwistle RC, Sammons SC, Bigley RF, et al. Material properties are related to stress fracture callus and porosity of cortical bone tissue at affected and unaffected sites. J Orthop Res. Apr 20 2009
Prognosis:
The prognosis for recovery is dependent on the location and severity of the fracture and on the age and underlying condition and associated comorbidities of the affected athlete
Most stress fracture carry a favorable prognosis for full recovery when
appropriate treatment has been provided
Sites at LOW risk of complications: are unlikely to have any of these complications
and are generally amenable to conservative management.
-fourth metatarsal shafts
-posteromedial tibial shaft
Sites at HIGH risk of complications: are managed more aggressively, often
surgically.
-anterior cortex of the tibia
-tarsal navicular
-proximal fifth metatarsal
-great toe sesamoids
-base of the second metatarsal
Treatment Recommendations:
Conservative therapy
Treatment should begin as soon as the injury is suspected, because delayed
treatment has been correlated with prolonged return to activity.
Ohta-Fukushima M, Mutoh Y, Takasugi S, Iwata H, Ishii S. Characteristics of stress fractures in young athletes under 20 years. J Sports Med Phys Fitness. 2002;42(2):198-206.
The patient can be examined every two to three weeks to ensure pain-free
functioning, monitor changes in symptoms, and evaluate improvement in provocative
testing
When patients are pain free, they may increase activity in a slow, graduated
manner.
Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987;15(1):46-58.
Treatment Recommendations:
Conservative therapy
Zelko R et al. Sress fracture in athletes: diagnosis and treatment. Postgrad AdvSport Med. 1986;I-IX:1-20.
Treatment Recommendations:
REST protocol
Bone remodeiling activity and rehabilitation goals based within each phase of cyclic rehabilitation protocol
Zelko R et al. Sress fracture in athletes: diagnosis and treatment. Postgrad AdvSport Med. 1986;I-IX:1-20. William A. Romani et al. Mechanisms and Management of Stress Fractures in Physically Active Persons. Journal of Athletic Training 2002;37(3):306–314.
Treatment Recommendations:
REST protocol
Zelko R et al. Sress fracture in athletes: diagnosis and treatment. Postgrad AdvSport Med. 1986;I-IX:1-20. William A. Romani et al. Mechanisms and Management of Stress Fractures in Physically Active Persons. Journal of Athletic Training 2002;37(3):306–314.
Treatment Recommendations:
REST protocol phase I
Initial treatment should include:
daily ice massages or contrast baths to decrease swelling.
analgesics
may be helpful if pain persists or becomes further limiting
Paracetamol may be considered for pain control
NSAIDs: !! inhibit the production of prostaglandins, which are demonstrated to be involved in normal bone remodeling and fracture healing.
Wheeler P, Batt ME. Do non-steroidal anti-inflammatory drugs adversely affect stress fracture healing? A short review. Br J Sports Med. 2005;39(2):65-69.
Treatment Recommendations:
REST protocol phase I
The use of pneumatic splints : splinting, casting, stirrup leg brace, boots
reduce abnormal tibial loading
provide support around the fracture site
reduce the length of the rehabilitation process
can significantly reduce pain and healing time in tibial and fibular stress fractures
more rapid return to sports participation [Evidence level A, meta-
analysis/RCT]
Whitelaw GP, Wetzler MJ, Levy AS, Segal D, Bissonnette K. A pneumatic leg brace for the treatment of tibial stress fractures. Clin Orthop 1991; 270:301-5. Brukner P. Exercise-related lower leg pain: bone. Med Sci Sports Exerc 2000;32(3 Suppl):S15-26. Shearman CM, Brandser EA, Parman LM, el-Khoury GY, Saltzman CL, Pyevich MT, Boles CA. Longitudinal tibial stress fractures: a report of eight cases and review of the literature. J Comput Assist Tomogr 1998;22:265-69. Rome K, Handoll HH, Ashford R. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 2005;(2):CD000450. Swenson EJ Jr, DeHaven KE, Sebastianelli WJ, Hanks G, Kalenak A, Lynch JM. The effect of a pneumatic leg brace on return to play in athletes with tibial stress fractures. Am J Sports Med 1997; 25:322-8. Matheson GO, Brukner P. Pneumatic leg brace after tibial stress fracture for faster return to play. Clin J Sport Med 1998;8(1):66. Gillespie WJ, Grant I. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev 2000;(2):CD000450.
Treatment Recommendations:
REST protocol phase III
During the functional phase of the program, the athlete continues the phase II exercises and progresses to mobility and jumping activities in the pool before their initiation on dry land.
Once the athlete can squat 1½ times body weight, higher-level plyometric training may begin.
Zelko R et al. Sress fracture in athletes: diagnosis and treatment. Postgrad AdvSport Med. 1986;I-IX:1-20.
Treatment Recommendations:
REST protocol phase III
The running portion of phase III is completed in a cyclic fashion that mimics bone growth.
As bone is being resorbed in the first 2 weeks of activity, running is encouraged to promote the formation of trabecular channels (functional phase).
In the third week, when the newly formed osteocytes and periosteum are maturing, running activity is decreased (rest phase).
As the running program progresses to sprinting and sport-specific activities, the rest days between functional activities decrease, and the athlete is gradually prepared for the return to competition.
Zelko R et al. Sress fracture in athletes: diagnosis and treatment. Postgrad AdvSport Med. 1986;I-IX:1-20.
Treatment Recommendations:
REST protocol phase III
Increasing activity
A good guideline is to increase activity no more than 15% to 20% per week.
A ‘‘walk-jog'' in which the injured person jogs the straightaways and walks the curves
of a track for 0.80 km
Once that distance is completed without pain, the injured person can begin walk-jogs
3 times per week.
Distance is added in 0.80 km increments per week until the athlete can complete
3.22 km.
At this point, jogging begins for 1.61 km and increases by 0.80 km per week until
4.83 km or a goal distance commensurate with the person's activity is reached.
Zelko R et al. Sress fracture in athletes: diagnosis and treatment. Postgrad AdvSport Med. 1986;I-IX:1-20.
Treatment Recommendations:
REST protocol
Zelko R et al. Sress fracture in athletes: diagnosis and treatment. Postgrad AdvSport Med. 1986;I-IX:1-20.
Treatment Recommendations:
Surgery
patients with recalcitrant stress fractures
patients with high-risk stress fractures
Kaeding CC, Yu JR, Wright R, Amendola A, Spindler KP. Management and return to play of stress fractures. Clin J Sport Med. 2005;15(6):442-447.
Périostite tibiale chez le
Etiology and Pathophysiology
Risk Factors
Intrinsic Factors
Extrinsic Factors
History Physical examination Imagery
Differential diagnosis
Treatment Recommendations
Shin splint is characterised by
diffuse tibial anteromedial or posteromedial surface subcutaneous periostitis most often on the medial border near the junction of the mid and distal thirds of
Moen MH, Tol JL, Weir A, Steunebrink M, De Winter TC. Medial tibial stress syndrome: a critical review. Sports Med 2009; 39: 523-546
Etiology and Pathophysiology:
to summarize
During the landing and propulsion of running
repetitive contraction of the posterior tibial, soleus and/or flexor digitorum longus muscles
would generate excessive stress on the tibia, resulting in inflammation from insertion of
the periosteal.
Michael RH, Holder LE. The soleus syndrome: a cause of medial tibial stress (shin splints). Am J Sports Med 1985 Mar-Apr; 13 (2): 87-94
Garth Jr WP, Miller ST. Evaluation of claw toe deformity, weakness of the foot intrinsics, and posteromedial shin pain. Am J Sports Med 1989 Nov-Dec; 17 (6): 821-7
Beck BR, Osternig LR. Medial tibial stress syndrome: the location of muscles in the leg in relation to symptoms. J Bone Joint Surg Am 1994 Jul; 76 (7): 1057-61
Craig DI. Medial tibial stress syndrome: evidence-based prevention. J Athl Train 2008 May-Jun; 43 (3): 316-8
Moen MH, Tol JL, Weir A, et al. Medial tibial stress syndrome: a critical review. Sports Med 2009; 39 (7): 523-46
Insufficient capacity for bone remodelling
due to repetitive and persistent stress on the tibia caused not only by the muscle
contraction but also on the vertical ground reaction during the landing phase in running.
Mubarak SJ, Gould RN, Lee YF, et al. The medial tibial stress syndrome: a cause of shin splints. Am J Sports Med 1982 Jul-Aug; 10 (4): 201-5
Craig DI. Medial tibial stress syndrome: evidence-based prevention. J Athl Train 2008 May-Jun; 43 (3): 316-8
Etiology and Pathophysiology:
to summarize
Despite different theories, clinical and research studies
on the cause of MTSS II, the fact that the detailed structural cause is still unknown highlights the need for prospective longitudinal investigations.
Etiology and Pathophysiology:
Cortical bone fatigue in MTSS II
The research on cortical bone cyclic testing, both in vitro and in vivo studies, provided invaluable data on the development of fatigue injury in cortical bone.
Like TSFs, cortical bone microtrauma occurring in MTSS II is likely the result of tensile
failure causing osteon debonding at the cement lines as the tibial microstructure is unable to
repair quickly enough through adaptive bone remodelling.
However, unlike a TSF, this microdamage clearly does not extend beyond the
microscopic lamellae structure, at least in many cases, so that crack development is
arrested in MTSS II before a macroscopic partial fracture transversing the osteons occurs.
Martin RB, Burr DB. Structure, Function, and Adaption of Compact Bone. 1st ed. New York: Raven Press, 1989: 189-192 Melanie Franklyn, Barry Oakes. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J Orthop 2015 September 18; 6(8): 577-589.
Etiology and Pathophysiology:
Does periostistis or cortical bone microtrauma
occur first in MTSS II?
Based on their MRI study of 14 patients with 18 symptomatic legs, Fredericson et al
postulated that periosteal oedema occurs prior to the formation of cortical bone
microcracks
as only periosteal oedema was detected in their patients with the mild injuries
while those with more severe injuries had both periosteal oedema and either a partial fracture, or marrow oedema indicating bone microtrauma.
Etherington et al studied a cohort of 40 male military recruits over 10 wk of basic training, 26 of whom completed the training, and measured a number of parameters including the velocity of ultrasound in the heel.
The authors found there was a mean decrease in the ultrasonic velocity from pre to
post training in recruits who completed the training uninjured
cortical bone microtrauma occurs prior to the development of any clinical
injury, and could be a precursor to periostitis.
Fredericson M, Bergman AG, Hoffman KL, Dillingham MS.Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med 1995; 23: 472-481. Etherington J, Keeling J, Bramley R, Swaminathan R, McCurdieI, Spector TD. The effects of 10 weeks military training on heel ultrasound and bone turnover. Calcif Tissue Int 1999; 64: 389-393
Shin splint is the main general Running-Related .Mus
culoskeletal Injuries
incidence ranging from 13.6% to 20.0%
prevalence of 9.5%
Alexandre Dias Lopes et al. What are the Main Running-Related Musculoskeletal Injuries? A Systematic Review. Sports Med 2012; 42 (10): 891-905
Epidemiology: Intrinsic Risk Factors
There is level I evidence for excessive pronation and female sex.
Level II evidence is available for the risk factors
increased internal and external hip ranges of motion
higher BMI
leaner calf girth
Studies on BMD and cortical bone geometric parameters demonstrate that patients with MTSS II have
lower BMD at the injury site than exercising controls
lower values of various cortical bone geometric factors (cross-sectional area and
section modulus) than aerobic control subjects
Maarten H. Moenet al. Medial Tibial Stress Syndrome A Critical Review. Sports Med 2009; 39 (7): 523-546. Melanie Franklyn, Barry Oakes. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J Orthop 2015 September 18; 6(8): 577-589.
Epidemiology: Extrinsic Risk Factors
Level II evidence is present for previous history of MTSS II
Maarten H. Moenet al. Medial Tibial Stress Syndrome A Critical Review. Sports Med 2009; 39 (7): 523-546.
Epidemiology: Risk factors and
associations with MTSS II
*Pronated foot type *Cohort studies have identified altered kinematics in MTSS sufferers, which may partly explain the link between previous history of MTSS and future MTSS, but to date no prospective trial has identified a specific kinematic risk factor.
Phil Newman et al. Risk factors associated with medial tibial stress syndrome in runners: a systematic review and meta-analysis. Open Access Journal of Sports Medicine 2013:4 229–241.
Diagnosis: History
The most common complaint of patients with MTSS II is vague, diffuse pain of the
lower extremity, along the middle-distal tibia associated with exertion.
In the early course of MTSS II, pain is worse at the beginning of exercise and
gradually subsides during training and within minutes of cessation of exercise.
As the injury progresses, however, pain presents with less activity and may occur at
rest.
Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265–79. Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33.
Diagnosis: History
A comprehensive history should be obtained to evaluate:
the athlete's weekly exercise routine and running mileage, intensity, pace, terrain, and
footwear, with careful attention to recent changes in training regimens.
training errors appear to be the most common factors involved in MTSS II, especially as
athletes attempt to do ‘‘too much, too fast''.
common training errors include a recent onset of increased activity, intensity, or duration.
running on hard or uneven surfaces is also a common risk factor.
Individuals with previous lower extremity injuries and running more than 30 km
per week are especially predisposed to overuse injuries of the lower extremity,
including MTSS II.
Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33. Fredericson M. Common injuries in runners. Diagnosis, rehabilitation and prevention. Sports Med. 1996;21:49–72. Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81. Strakowski J, Jamil T. Management of common running injuries. Phys Med Rehabil Clin N Am. 2006;17(3):537–52. Dugan S, Weber K. Stress fracture and rehabilitation. Phys Med Rehabil Clin N Am. 2007;18(3):401–16.
Diagnosis: Physical examination
The medial ridge of the tibia, origin of the tibialis posterior and soleus muscles is often
tender to palpation, especially at the distal and middle tibial regions.
Examine for any subcutaneous oedema, which indicates periostitis is present and
probable associated microfractures.
The anterior tibia, however, is usually nontender.
Neurovascular symptoms are usually absent.
R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133. Melanie Franklyn, Barry Oakes. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J Orthop 2015 September 18; 6(8): 577-589.
Diagnosis: Physical examination
Physicians should carefully evaluate for possible knee abnormalities (especially genu
varus or valgus), tibial torsion, femoral anteversion, foot arch abnormalities, or a
leg-length discrepancy.
Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265–79.
Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33.
Strakowski J, Jamil T. Management of common running injuries. Phys Med Rehabil Clin N Am. 2006;17(3):537–52.
Ankle movements and subtalar motion should also be evaluated:
hyperpronation of the subtalar joint is one of the most common and well-documented risk factors for MTSS.
Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265–79.
Thacker S, Gilchrist J, Stroup D, Kimsey C. The prevention of shin splints in sports: a systematic review of literature. Med Sci Sports Exerc. 2002;34(1):32–40.
Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33.
Fredericson M. Common injuries in runners. Diagnosis, rehabilitation and prevention. Sports Med. 1996;21:49–72.
Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med.2004;23:55–81.
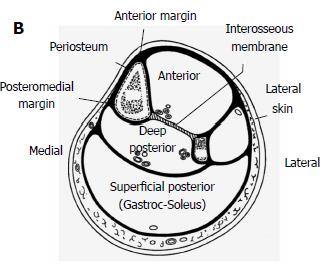
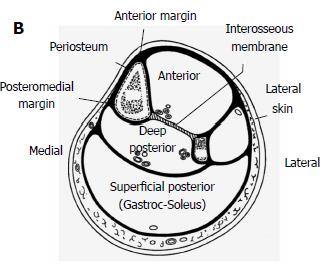
Diagnosis: Physical examination
Hyperpronation of subtalar joint. (A) Medial, (B) anterior views.
R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133
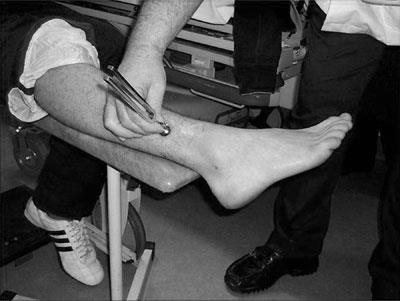
Diagnosis: Physical examination
The Navicular Drop Test (NDT) was first described as a means of quantifying the amount of foot pronation in runners.
It's intended to represent the sagittal plane displacement of the navicular tuberosity from a neutral position to a relaxed position in standing.
Measurement of navicular drop. The height of the navicular tuberosity is measured in neutral (A) and relaxed (B) stance positions, and the amount of excursion is measured.
Menz HB. Alternative techniques for the clinical assessment of foot pronation. J Am Podiat Med Assn 1998;88:119-29.
Diagnosis: Physical examination
Muscle imbalance and inflexibility, especially tightness of the triceps surae
(gastrocnemius, soleus, and plantaris muscles), is commonly associated with MTSS
II.
Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265–79.
Fredericson M. Common injuries in runners. Diagnosis, rehabilitation and prevention. Sports Med. 1996;21:49–72.
Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med.2004;23:55–81.
A weakness in one or more muscle compartments or in a myotome may indicate lumbar spinal nerve compression or other isolated motor nerve pathologies including rare entrapment syndromes.
A full strength/power assessment of all the muscles of the leg should be performed
Melanie Franklyn, Barry Oakes. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J Orthop 2015 September 18; 6(8): 577-589.
Diagnosis: Physical examination
Weakness of core muscles is an important risk factor for lower extremity injuries.
Hip and pelvis muscle strength are an important link in maintaining control and proper mechanics between the ‘‘core'' and lower extremity.
Core and pelvic muscle stability may be assessed by evaluating patient's ability to maintain a controlled, level pelvis during a pelvic bridge from the supine position, or a standing single-leg knee bend.
Niemuth P, Johnson R, Myers M, Thieman T. Hip muscle weakness and overuse injuries in recreational runners. Clin J Sport Med. 2005;15(1):14–21. Messier S. Etiologic factors associated with selected running injuries. Med Sci Sports Exerc. 1998;20:501–5. Ravin T, Cantieri M, Pasquarello G. Principles of prolotherapy,vol. 233. Denver, CO: American Academy of Musculoskeletal Medicine; 2008. p. 250–1. Thijs Y, Van Tiggelen D, Willems T, De Clercq D, Witvrouw E. Relationship between hip strength and frontal plane posture of the knee during a forward lunge. Br J Sports Med. 2007;41:723–7. Nadler F, Malanga G, DePrince M, Stitik T, Feinberg J. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000;10(2):89–97. Leetun D, Ireland M, Wilson J, Ballantyne B, Davis I. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926–34. Greenman P. Principles of manual medicine. 3rd ed., chap. 11. Philadelphia, PA: Lippincott Williams & Wilkins; 2003: p. 337–403, 489.
Diagnosis: Physical examination
The physician should perform a standing postural examination to evaluate the
entire kinetic chain, especially if the symptoms are recurrent.
Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81.
Greenman P. Principles of manual medicine. 3rd ed., chap. 11. Philadelphia, PA: Lippincott Williams & Wilkins; 2003: p. 337–403, 489.
Kibler W, Chandler T, Pace B. Principles of rehabilitation after chronic tendon injuries. Clin Sports Med. 1992;11(3):661–71.
Abnormal gait patterns should be evaluated with the patient walking and running,
either in the office hallway or on a treadmill.
Strakowski J, Jamil T. Management of common running injuries. Phys Med Rehabil Clin N Am. 2006;17(3):537–52.
Dugan S, Weber K. Stress fracture and rehabilitation. Phys Med Rehabil Clin N Am. 2007;18(3):401–16.
Diagnosis: Imagery
Imaging is usually not necessary for the diagnosis of MTSS II.
However, if the patient fails to improve with conservative management, plain film
radiography may be considered.
X-rays are usually negative within the first 2–3 weeks after the onset of injury.
Mellion M, Walsh W, Madden C, Putukian M, Shelton G. The team physician's handbook. 3rd ed. Philadelphia, PA: Hanley & Belfus; 2002. p. 517, 583.
Long-term radiographic changes of those with chronic MTSS II with periosteal involvement may show periosteal exostoses.
Those that progress from MTSS II to stress fracture may develop a dreaded black line on radiograph, which indicates a more ominous sign.
Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints'. Phys Sportsmed. 2002;30(6):29–36.
Diagnosis: Imagery
Medial tibial stress syndrome http://radiopaedia.org/images/2860801 January 16, 2013
Diagnosis: Imagery
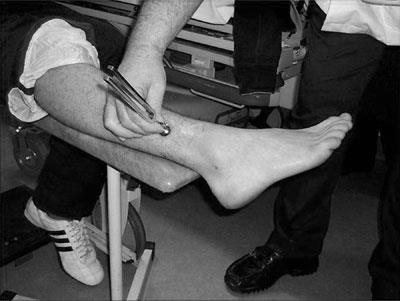
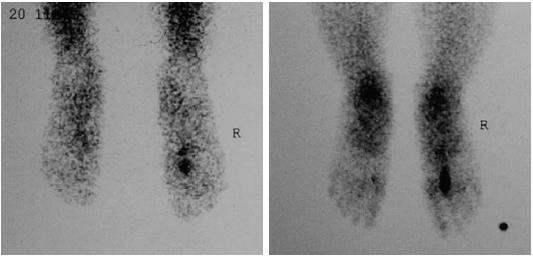
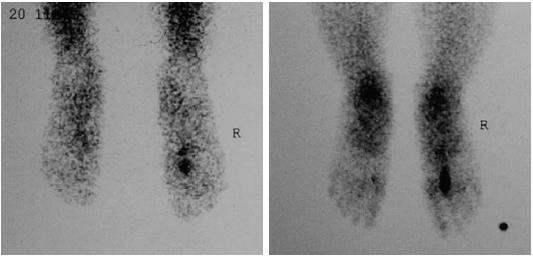
A triple-phase bone scan demonstrates evidence of a stress fracture with a diffuse,
longitudinal uptake along the posterior tibia, seen only on the delayed phase of the
scan.
Bone scans have been the gold standard for diagnosing stress fractures in the past, but now are often replaced by magnetic resonance imaging (MRI).
Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stressvsyndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33. Young A, McAllister D. Evaluation and treatment of tibial stress fractures. Clin Sports Med. 2006;25(1):117–28.
Diagnosis: Imagery
Blood pool and delay images show linear uptake increase in the cortical aspects of tibia in the two sides. Rest of exam was normal.
Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics. 2003 Mar-Apr;23(2):341-58.
Diagnosis: Imagery
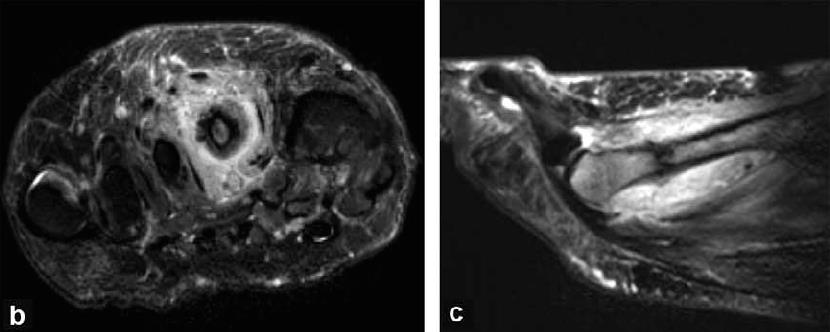
MRI has many advantages over a bone scan and plane radiography. MRI is better
able to identify other soft tissue injuries.
MRI can show progression of injury in the tibia, starting with periosteal edema, progressive marrow involvement, and finally cortical stress fracture.
With better accuracy, MRI can grade tibial injuries according to extent of involvement.
Grading tibial injuries may help clinicians make more accurate recommendations for rehabilitation, though no literature data exist about MRI findings and specific return-to-play guidelines.
M, Bergman G, Hoffman K, Dillingham M. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic
resonance imaging grading system. Am J Sports Med. 1995;23:427–81. Dugan S, Weber K. Stress fracture and rehabilitation. Phys Med Rehabil Clin N Am. 2007;18(3):401–16. Young A, McAllister D. Evaluation and treatment of tibial stress fractures. Clin Sports Med. 2006;25(1):117–28. DeLee J, Drez D, Mil er M. DeLee and Drez's orthopaedic sports medicine principles and practice. Philadelphia, PA: Saunders; 2003. p. 2155–9.
Diagnosis: Imagery
Coronal T2-weighted magnetic resonance imaging images of a 17-year-old female hockey player who was training on a concrete pitch covered with Astro Turf® for approximately 2 mo and was subsequently diagnosed with medial tibial stress syndrome. A white longitudinal line of periosteal oedema on the medial cortex can clearly be seen on the enlarged view (right), which was consistent with the region of pain and tenderness.
Melanie Franklyn, Barry Oakes. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J Orthop 2015 September 18; 6(8): 577-589.
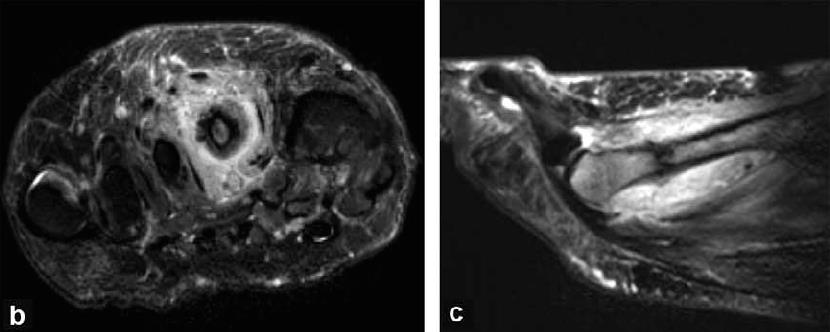
Diagnosis: Imagery
MRI image of bilateral shin splint (T2 fat sat) : limited juxta cortical hypersignal
H de Labareyre et al. Douleurs d'origine tibiale chez le sportif. J. Traumatol. Sport 2000, 17, 163-177.
Differential diagnosis:
Traditional differential diagnosis and classification of medial tibial stress syndrome.
Detmer DE. Chronic shin splints: classification and management of medial tibial stress syndrome. Sports Med. 1986;3(6):436–446 In Phil Newman et al. Risk factors associated with medial tibial stress syndrome in runners: a systematic review and meta-analysis. Open Access Journal of Sports Medicine 2013:4 229–241.
Differential diagnosis:
Physicians should also be aware of less common causes of lower extremity exertional-pain:
effort-induced venous thrombosis
peroneal nerve entrapment
R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133
Treatment Recommendations:
Conservative therapy - Goals
Summary of treatment goals for MTSS II
R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133
Conservative therapy :
4 stages program
PHASE 1- Acute Phase:
decrease acute pain and inflammation:
absolute rest- NWB with crutches
relative rest- WB boot or walker
"ICE" : ice; compression; elevation
NSAIDS and Acetaminophen depending on the severity of their symptoms
Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265–79. Fredericson M, Bergman G, Hoffman K, Dillingham M. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23:427–81. Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33. Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81. Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints'. Phys Sportsmed. 2002;30(6):29–36.
Conservative therapy – Acute Phase
Most literature supports ‘‘rest'' as the most important treatment in the acute phase of MTSS II.
Taube R, Wadsworth L. Managing tibial stress fractures. Phys Sportsmed. 1993;21:123–30.
Fredericson M, Bergman G, Hoffman K, Dillingham M. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23:427–81.
Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265–79.
Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33.
Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints'. Phys Sportsmed. 2002;30(6):29–36.
DeLee J, Drez D, Miller M. DeLee and Drez's orthopaedic sports medicine principles and practice. Philadelphia, PA: Saunders; 2003. p. 2155–9.
Patients may require ‘‘relative'' rest and cessation of sport for prolonged periods of time (from 2 to 6 weeks)
Conservative therapy – Acute Phase
It is the opportunity to discover other completely complementary sports, soft and "low gravity":
For all these sports, it is possible to realize as well sessions of endurance as session of strong cardiac request
Conservative therapy – Acute Phase
It is even possible, with precaution (strapping), to realize sessions of ascents of staircase to make cardiovascular workout.
Self-made compression sockets
Conservative therapy – Acute Phase
Cryotherapy
is also commonly used in the acute period. Ice may be applied to the affected area directly after exercise for approximately 15–20 min.
R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133
Conservative therapy – Acute Phase
Physical therapy modalities:
augmented soft tissue mobilization
electrical stimulation
Fredericson M, Bergman G, Hoffman K, Dillingham M. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23:427–81.
Fredericson M. Common injuries in runners. Diagnosis, rehabilitation and prevention. Sports Med. 1996;21:49–72.
Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265–79.
Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33.
Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints'. Phys Sportsmed. 2002;30(6):29–36.
DeLee J, Drez D, Miller M. DeLee and Drez's orthopaedic sports medicine principles and practice. Philadelphia, PA: Saunders; 2003. p. 2155–9.
Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81.
Dugan S, Weber K. Stress fracture and rehabilitation. Phys Med Rehabil Clin N Am. 2007;18(3):401–16.
R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133
Conservative therapy – Acute Phase
Depending on the severity of the problem the acute phase can be bypassed but should always be considered especially if clinical symptoms are significant.
When palpation of the involved shin area exhibits minimal to no discomfort the rehabilitation phase can be initiated.
Conservative therapy :
4 stages program
PHASE 2- Rehabilitation Phase:
Further decrease pain and inflammation:
decrease scar formation:
transverse friction/deep tissue massage
augmented soft tissue mobilization
Maintain/increase flexibility of injured (and surrounding) tissue:
active > passive joint range of motion
stretching exercises
Strengthen fascial/bone interface:
open to closed chain therapeutic exercise (isometric > isotonic > isokinetic)
Conservative therapy –
Rehabilitation Phase
Stretching and strengthening exercises
Literature has widely supported a daily regimen of calf stretching and eccentric calf
exercises to prevent muscle fatigue.
Other exercises focus on strengthening the tibialis anterior and other muscles
controlling both inversion and eversion of the foot.
Bec k B. Tibial stress injuries: an aetiological review for the purposesof guiding management. Sports Med. 1998;26(4):265–79.
Fredericson M, Bergman G, Hoffman K, Dillingham M. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23:427–81.
Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33.
Fredericson M. Common injuries in runners. Diagnosis, rehabilitation and prevention. Sports Med. 1996;21:49–72.
Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81.
Dugan S, Weber K. Stress fracture and rehabilitation. Phys Med Rehabil Clin N Am. 2007;18(3):401–16.
Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints'. Phys Sportsmed. 2002;30(6):29–36.
Korkola M, Amendola A. Exercise-induced leg pain. Sifting through a broad differential. Phys Sportsmed. 2001;29(6):35–50.
Taube R, Wadsworth L. Managing tibial stress fractures. Phys Sportsmed. 1993;21:123–30.
Herring K. A plyometric training model used to augment rehabilitation from tibial fasciitis. Curr Sports Med Rep. 2006;5(3): 147–54.
R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133
Conservative therapy –
Rehabilitation Phase
Stretching and strengthening exercises
R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133. Therasa Timmons, John Locke, Jennifer Brennan, Anna Foster, Chad Gabbard, Jennifer Johnson, Justin Miller, Richard Santerre, Craig Stull.TREATMENT OF SHIN SPLINTS. St. Vincent Hospital and St. Vincent Sports Performance in Indianapolis.
Conservative therapy –
Rehabilitation Phase
Patients may also benefit from strengthening core and hip muscles.
Developing core stability with strong abdominal, gluteal, and hip muscles can improve running mechanics and prevent lower-extremity overuse injuries.
Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265–79. Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81. Strakowski J, Jamil T. Management of common running injuries. Phys Med Rehabil Clin N Am. 2006;17(3):537–52. Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints'. Phys Sportsmed. 2002;30(6):29–36. Plastaras C, Rittenberg J, Rittenberg K, Press J, Akuthota V. Comprehensive functional evaluation of the injured runner. Phys Med Rehabil Clin N Am. 2005;16(3):623–49. Sommer H, Vallentyne S. Effect of foot posture on the incidence of medial tibial stress syndrome. Med Sci Sports Exerc. 1995;27:800–4. Niemuth P, Johnson R, Myers M, Thieman T. Hip muscle weakness and overuse injuries in recreational runners. Clin J Sport Med. 2005;15(1):14–21. Hootman J, Macera C, Ainsworth B, Martin M, Addy C, Blair S. Predictors of lower extremity injury among recreationally active adults. Clin J Sport Med. 2002;12:99–106.
Conservative therapy –
Rehabilitation Phase
When patient can complete these exercises without symptoms then the functional phase can begin.
The techniques used to decrease scar formation can initially exacerbate the condition especially when using augmented soft tissue mobilization.
Conservative therapy :
4 stages program
PHASE 3- Functional Phase:
Functionally strengthen fascial/bone interface and surrounding tissue
continue open to closed chain therapeutic exercise
plyometric training : trampoline > jumping rope > "vertical jumps"
Protect injured area during functional activity:
neoprene shin sleeve
consider leg brace (Air Cast)
appropriate athletic foot gear
Conservative therapy – Functional Phase
Footwear
Shoes should fit properly with a stable heel counter.
Some physicians recommend alternating running shoes especially when one pair is wet, as this compromises the shoe's integrity.
Runners should also change running shoes every 400–800 km, a distance at which
most shoes lose up to 40% of their shock-absorbing capabilities and overall support .
Athletes should seek out shoes with sufficient shockabsorbing soles and insoles,
as they reduce forces through the lower extremity and can prevent repeat episodes of
MTSS II.
Beck B. Tibial stress injuries: an aetiological review for the purposesof guiding management. Sports Med. 1998;26(4):265–79.
Thacker S, Gilchrist J, Stroup D, Kimsey C. The prevention of shin splints in sports: a systematic review of literature. Med Sci Sports Exerc. 2002;34(1):32–40.
Level I evidence is available
Marinus Winters et al. Treatment of Medial Tibial Stress Syndrome: A Systematic Review. Sports Med (2013) 43:1315–1333.
Conservative therapy – Functional Phase
Orthotics
Individuals with biomechanical problems of the foot may benefit from orthotics.
Fredericson M, Bergman G, Hoffman K, Dillingham M. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23:427–81.
Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33.
Fredericson M. Common injuries in runners. Diagnosis, rehabilitation and prevention. Sports Med. 1996;21:49–72.
Strakowski J, Jamil T. Management of common running injuries. Phys Med Rehabil Clin N Am. 2006;17(3):537–52.
Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints'. Phys Sportsmed. 2002;30(6):29–36.
DeLee J, Drez D, Miller M. DeLee and Drez's orthopaedic sports medicine principles and practice. Philadelphia, PA: Saunders; 2003. p. 2155–9.
Often, over-the-counter orthosis (flexible or semi-rigid) are sufficient to help with excessive foot pronation and pes planus.
Mal-alignments caused by forefoot or rearfoot abnormalities may benefit from custom orthotics.
Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33.
Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints'. Phys Sportsmed. 2002;30(6):29–36.
Sommer H, Vallentyne S. Effect of foot posture on the incidence of medial tibial stress syndrome. Med Sci Sports Exerc. 1995;27: 800–4.
Conservative therapy – Functional Phase
Lower leg braces
Marinus Winters et al. Treatment of Medial Tibial Stress Syndrome: A Systematic Review. Sports Med (2013) 43:1315–1333.
Conservative therapy – Functional Phase
This is probably the most important phase because it prepares the patient for their return to activity.
Care needs to be taken at this stage not to allow the patient to overdo these exercises and stay within their limits as re-injury can easily occur.
Conservative therapy :
4 stages program
PHASE 4- Return To Activity
Return to desired sport activity:
gradual, systematic, "to tolerance"
Initiate preventive strategies:
appropriate athletic shoewear
functional exercises (i.e., Pilates, plyometrics)
revise training program
Conservative therapy –
Return To Activity Phase
Graded Running Program, Stretching/Strengthening and Sports Compression
Stockings
RCT study performed in an athletic population n=74
The study design was randomized and multi-centered
Primary outcome measure was: time to complete a running program (able to run 18 minutes with high intensity)
Secondary outcome was: general satisfaction with treatment
Moen MH, Holtslag L, Bakker E, et al. The treatment of medial tibial stress syndrome in athletes; a randomized clinical trial. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(1):12.
Conservative therapy –
Return To Activity Phase
Graded Running Program
The first four phases of the graded running program consisted of interval training in which duration was increased from 16 to 20 minutes and intensity increased from light jogging to a running speed where speaking became difficult. When "meters run at 10 km/hour" was between 0-400 meters, the athlete started the running program in phase one. When 401-800 meters could be run, the athlete started in phase two. When 801-1200 meters could be run the athlete started in phase three. When 1201-1600 meters could be run, the athlete started phase four. When 1600 meters or more could be run, athletes started phase five. In phases 5 and 6, continuous running was performed for 16 and 18 minutes, respectively, and the intensity was increased from light jogging to running at a speed where speaking became difficult. A new phase of the running program was commenced when a phase was finished without a pain score of 4 or higher on the 1–10 VAS. Training was performed three times a week, on non-consecutive days.
Moen MH, Holtslag L, Bakker E, et al. The treatment of medial tibial stress syndrome in athletes; a randomized clinical trial. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(1):12.
Conservative therapy –
Return To Activity Phase
Graded Running Program
+ Exercises with 5 days a week stretching of the calf and strengthening
+ Stabilizing exercises of the ankle
Moen MH, Holtslag L, Bakker E, et al. The treatment of medial tibial stress syndrome in athletes; a randomized clinical trial. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(1):12.
Conservative therapy –
Return To Activity Phase
Graded Running Program
+ Compression Stockings
Moen MH, Holtslag L, Bakker E, et al. The treatment of medial tibial stress syndrome in athletes; a randomized clinical trial. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(1):12.
Conservative therapy –
Return To Activity Phase
Graded Running Program, Stretching/Strengthening and Sports Compression
Stockings
No differences were found between the groups for the time to completion of
the graded running program.
Moen MH, Holtslag L, Bakker E, et al. The treatment of medial tibial stress syndrome in athletes; a randomized clinical trial. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(1):12.
Conservative therapy –
Return To Activity Phase
Modify the training routine
Decreasing weekly running distance, frequency, and intensity by 50% will likely
improve symptoms without complete cessation of activity.
Runners are encouraged to avoid running on hills and uneven or very firm
surfaces.
Synthetic track or a uniform surface of moderate firmness provides more shock absorption
and cause less strain on the lower extremity.
During this time, athletes can benefit from cross training with other low-impact
exercises, such as
pool running, swimming, using an elliptical machine, or riding a stationary bicycle.
Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265–79. Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33. Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81. Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints'. Phys Sportsmed. 2002;30(6):29–36. Stanitski C, McMaster J, Scranton P. On the nature of stress fractures. Am J Sports Med. 1978;6(6):391–6. DeLee J, Drez D, Miller M. DeLee and Drez's orthopaedic sports medicine principles and practice. Philadelphia, PA: Saunders; 2003. p. 2155–9. R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133
Conservative therapy –
Return To Activity Phase
There is an approximate one month window after the patient returns to their activity where the chance of reinjury is great.
Patients must realize their limits and be patient!
Treatment Recommendations:
Conservative therapy - shock wave therapy
Non-randomized clinical trial studied the effect of radial ESWT in addition to a 12-week home training program, relative rest and ice appliance compared with a 12-week home training program, relative rest and ice appliance only,
radial ESWT in addition to an exercise home training program was found to
improve global perceived effect and severity of pain when compared with a home
training program only.
Rompe JD, Cacchio A, Furia JP, et al. Low-energy extracorporeal shock wave therapy as a treatment for medial tibial stress syndrome. Am J
Sports Med. 2010;38(1):125–32.
Non-randomized clinical trial studied the effect of a six-phase graded running program compared with the same running program with the addition of focused ESWT This study was performed in an athletic population.
focused ESWT in addition to a graded running program reduced time to
completion of a graded running program significantly more than a graded running
program alone.
Moen MH, Rayer S, Schipper M, et al. Shockwave treatment for medial tibial stress syndrome in athletes; a prospective controlled study. Br J
Sports Med. 2012;46(4):253–7.
Treatment Recommendations:
Conservative therapy - Injections
Newer methods, such as dry-needling, autologous blood injection, platelet-rich plasma, and prolotherapy, seek to stimulate a local healing response in injured tissues.
Some physicians have proposed injecting the spring and short plantar ligaments to treat laxity and poor mechanics of the foot arch, which are common factors contributing to hyperpronation.
However, no RCTs have been performed with these different injection techniques for
MTSS II.
Ravin T, Cantieri M, Pasquarello G. Principles of prolotherapy, vol. 233. Denver, CO: American Academy of Musculoskeletal Medicine; 2008. p. 250–1. R. Michael Galbraith, Mark E. Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133
Treatment Recommendations:
Conservative therapy - Acupuncture
Studies identified benefit of acupuncture for MTSS II, but had a small sample size
and various methodological shortcomings.
Callison M. Acupuncture and tibial stress syndrome (shin splints). J Chinese Med. 2002;70:24–7.
Schulman RA. Tibial shin splints treated with a single acupuncture session: case report and review of the literature. J Am Med Acupuncture 2002; 13 (1): 7-9]
Treatment Recommendations:
Surgical options
Surgery for MTSS II is usually reserved for recalcitrant cases who do not respond with conservative treatment.
A ‘‘posterior fasciotomy'' is the common procedure performed.
This may include cauterization of the posteromedial ridge of the tibia.
Surgical results are variable and not likely to cause complete resolution of symptoms but may improve pain and function.
Intramedullary nail placement has been used for those with stress fractures in season.
Detmer D. Chronic shin splints. Classification and management of medial tibial stress syndrome. Sports Med. 1986;3(6):436–46. Kortebein P, Kaufman K, Basford J, Stuart M. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–33. Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81 Sommer H, Vallentyne S. Effect of foot posture on the incidence of medial tibial stress syndrome. Med Sci Sports Exerc. 1995;27: 800–4. DeLee J, Drez D, Mil er M. DeLee and Drez's orthopaedic sports medicine principles and practice. Philadelphia, PA: Saunders; 2003. p. 2155–9. Yates B, Allen M, Barnes M. Outcome of surgical treatment of medial tibial stress syndrome. J Bone Joint Surg. 2003;85:1974–80. Abramowitz A, Schepsis A, McArthur C. The medial tibial syndrome: the role of surgery. Orthop Rev. 1994;23(11):875–81.
Merci de votre attention!
Source: http://www.ardenne-orthopedie.be/wp-content/uploads/2015/12/29eColloqueM%C3%A9decineSport_Dr-PRIST.pdf
O'Shaughnessy's • Winter 2015/16 —7— Cannabis in the Treatment of Pediatric Epilepsy By Bonni Goldstein, MD The author documents the progress of more than 100 patients using CBD-rich cannabis oil to treat seizure disorders. I have been a medical cannabis physician seeing adult tion they are going to give their child. They cannot give oil, the added expense of testing every bottle becomes pro-
Carola Fortelius ERASMUS intensive course Tikkurila, 1st of June 2010 • Microbes – who are they? • Microbes – how to work with them • Cultivation of microbes • Factors affecting microbial growth • How to control microbial growth in restoration work Intoduction to Microbiology What do you know about nothing ? -------------------------------------------- a lot