Cats.rwth-aachen.de
Annals of Biomedical Engineering (! 2010)DOI: 10.1007/s10439-010-0228-7
Hypothermic Machine Perfusion of Kidney Grafts:
Which Pressure is Preferred?
B. M. DOORSCHODT,1 M. C. J. M. SCHREINEMACHERS,2 M. BEHBAHANI,3 S. FLORQUIN,2 J. WEIS,4 M. STAAT,5
1Institute for Laboratory Animal Science and Experimental Surgery, RWTH-Aachen University, Pauwelsstr. 30, 52074 Aachen,
Germany; 2Department of Pathology, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ
Amsterdam, The Netherlands; 3Chair for Computational Analysis of Technical Systems, RWTH-Aachen University,
Schinkelstr. 2, 52062 Aachen, Germany; 4Institute of Neuropathology, RWTH-Aachen University, Pauwelsstr. 30,
52074 Aachen, Germany; and 5Institute of Bioengineering and Biomechanics Laboratory, Aachen University of Applied
Sciences, Heinrich-Mußmann-Str. 1, 52428 Ju¨lich, Germany
(Received 27 April 2010; accepted 26 November 2010)
Associate Editor Stefan Jockenhoevel oversaw the review of this article.
Abstract—To assess the effect of the perfusion pressure (PP)
during machine perfusion (MP) on the preservation quality ofkidney grafts, we compared mean PPs of 25 and 30 mmHg
Currently, hypothermic machine perfusion (MP) is
using a porcine autotransplantation model. After assessment
gaining ground as the preservation method of choice
of the microcirculation, animals underwent left nephrectomy.
for kidney grafts since the first large clinical random-
Thereafter, kidneys were washed out followed by 20 h of MPat 25 mmHg (MP25, n = 7) or 30 mmHg (MP30, n = 7)
ized study demonstrated a beneficial effect of MP over
using a novel MP system for hypothermic pulsatile perfusion.
cold storage The benefit of MP is probably that
After MP preservation, the contralateral kidneys were
it ensures a uniform distribution of preservation fluid
removed and the preserved kidneys heterotopically auto-
throughout the organ, which is better than a single
transplanted. Ten minutes after reperfusion, the microcircu-
flush.Although MP provides favorable preservation
lation was reassessed. Seven days posttransplant, animalswere euthanized and the kidney grafts removed for histolog-
quality over CS, it remains a more complex and
ical analysis. MP using a mean PP of 25 mmHg resulted in
expensive procedure. Therefore, simple CS preserva-
higher capillary blood flow after reperfusion. In the MP30
tion is still the preservation method of choice. Inter-
group, 6 out of 7 animals survived, whereas in the MP25
estingly, in addition to the favorable results of MP
group all animals survived. Overall, improvement in recovery
regarding renal function, recently, two studies on the
of renal function and a better preservation of structuralintegrity were seen in the MP25 group compared to the MP30
cost-effectiveness of MP as a preservation method for
group. Using a novel system for hypothermic MP, a mean PP
kidney grafts demonstrated that MP is preferable to
of 25 mmHg is preferred over a mean PP of 30 mmHg.
CS since it adds substantial value, not only from afunctional perspective but foremost from a cost-
Keywords—Perfusion pressure, Preservation, Transplanta-
effective perspective.Therefore, it is expected that
MP will gain a wider clinical acceptance in the nearfuture.
Nowadays, three MP systems are commercially
available; The LIFEPORT (Organ Recovery SystemsInc., Des Plaines, IL, USA), the RM3 (Waters Medical
Perfusion pressure
Systems LLC, Plymouth, MN, USA), and the KIDNEY
Machine perfusion
ASSIST (Organs Assist BV, Groningen, the Nether-
lands). These systems are used in combination withKPS-1 (Organ Recovery Systems Inc., IL, USA) which
Address correspondence to R. H. Tolba, Institute for Laboratory
is currently the only commercially available MP solu-
Animal Science and Experimental Surgery, RWTH-Aachen Uni-
tion. In the MP systems, the mean perfusion pressure
versity, Pauwelsstr. 30, 52074 Aachen, Germany. Electronic mail:
(PP) with which the perfusion medium is provided to the
This study was performed at the House of Experimental Therapy,
organ can be altered by the operator. In a survey of 12
University Clinic of Bonn, Sigmund-Freud-Str. 25, 53105 Bonn,
organ procurement organizations in the US which used
Germany and in part at the affiliations mentioned above.
! 2010 Biomedical Engineering Society
DOORSCHODT et al.
MP for kidney preservation, a variety of PPs were
GmbH, Ulm, Germany), all administered intrave-
nously (IV) by means of a butterfly cannula inserted
Although Moers et al. applied a fixed systolic PP of
into an external marginal ear vein and maintained after
30 mmHg in the aforementioned clinical trial, other
intubation by mechanical ventilation with isoflurane.
clinical and preclinical investigators applied different
Thereafter, the right internal jugular vein was cannu-
mean PPs. In a study comparing CS and MP for the
lated with a PE (polyethylene) catheter for infusion
preservation of kidney grafts using a porcine kidney
and daily collection of blood samples. After the
autotransplantation model, Nicholson et al.applied
assessment of the microcirculation at four pre-defined
a mean arterial PP of 60 mmHg. Treckmann et
locations on the renal surface using a combined laser
applied a systolic PP of 40–50 mmHg, whereas
Doppler and flowmetry system (oxygen-to-see, O2C
Maathuis et aldemonstrated that a PP of 30/20 mmHg
system, LEA Medizintechnik, Giessen, Germany), a
provided favorable results over 60/40 mmHg.
left nephrectomy was performed. Immediately there-
Recently, a new MP system with a gas pressure-
after, kidneys were washed out ex vivo using 500 mL of
driven perfusion pump has been developed for hypo-
POLYSOL (Doorzand Polysol B.V., Amsterdam, The
thermic pulsatile perfusion of kidney This
Netherlands) at 4 "C at a hydrostatic pressure of
system is used in combination with POLYSOL, a new
100 cm H2O followed by weighing of the grafts.
low viscosity solution (cP at 5 "C: 1.8 vs. 2.5 of KPS-1)which has been developed for washout and hypother-
mic MP and CS preservation of abdominal organs.
POLYSOL demonstrated favorable results in CS kid-
Subsequently, kidneys were connected to the MP
ney preservation as demonstrated by an improved
microcirculatory status and improved graft functi
Amsterdam, The Netherlands) for a 20 h period. The
The aim of this study was to assess the effect of the PP
features of the AIRDRIVE MP system have been
during hypothermic MP preservation of kidney grafts.
described in detail previously.Oxygen pressure gener-
To this end, pulsatile perfusion preservation at a mean
ated by a 2 L medical oxygen cylinder is used to propel
PP of 25 mmHg was compared to MP at a PP 30 mmHg
a pulsatile membrane pump and to actively oxygenate
using a porcine kidney autotransplantation model.
the perfusion medium during perfusion at 4 "C. Forthis study, the mean PP of the pressure-controlled MPsystem was preset according to the group assigned,
MATERIALS AND METHODS
MP25 or MP30. The mean PP was calculated by the
Animals and Experimental Protocols
onboard electronic control system from continuousrecordings of the pressure sensor and defined as the
All experiments were performed in accordance
mean area under the pressure curve during 10 pump
with the German legislation governing animal studies
cycles. For in line recording of the PP, a temperature
following the Principles of Laboratory Animal Care
compensated and calibrated silicon pressure sensor
(NIH publication, 85–23, revised 1985). Kidneys were
was used (MPX2010GST1, Freescale Semiconductor,
retrieved from female German landrace pigs, weighing
Chandler, AZ, USA) which has a full scale span
24.9 ± 4.1 kg (mean ± SD). This study describes two
pressure hysteresis of ±0.1% and temperature hyster-
groups, both representing a different PP during MP,
esis of ±0.5%. The perfusion flow was calculated in
MP at 25 mmHg (MP25, n = 7) and MP at 30 mmHg
real time by the amount of pump strokes per minute
(MP30, n = 7). Randomization of the groups was
times the stroke volume of 12 mL (±2%). Perfusion
performed using a roulette wheel.
parameters, flow and renal resistance (mmHg/mL/(100 g) kidney weight), were continuously monitored.
Surgical Procedures
Kidney weights after 20 h MP were recorded.
Animals were premedicated with ketamine (90 mg/
kg, Parke-Davis GmbH, Berlin, Germany), xylazine
(10 mg/kg, Bayer Vital GmbH, Leverkusen, Ger-
Twenty hours after left nephrectomy, the contra-
many), and atropine (10 lg/kg, Bremer Pharma
lateral kidney was removed, followed by immediate
GmbH, Warburg, Germany) administered intramus-
heterotopic transplantation of the preserved kidney.
cularly (IM). General anesthesia was induced by
The renal artery was anastomosed end-to-end to the
midazolam (0.5 mg/kg, Roche GmbH, Grenzach-
right renal artery and the renal vein end-to-side to the
Wyhlen, Germany), and fentanyl (12.5 lg/kg, Janssen-
inferior vena cava. Before completion of the arterial
Cilag GmbH, Neuss, Germany), muscle relaxation was
anastomosis, a bolus of 3,000 IU of heparin was
achieved by pancuronium (0.2 mg/kg, Ratiopharm
injected to prevent vascular thrombosis. Following
Perfusion Pressures During Machine Perfusion of Kidneys
reperfusion, 250 mL of 20% glucose was administered
from 0 to 5: 0 = no abnormality, 1 = mild, lesions
intravenously to induce osmotic diuresis. The ureter
affecting up to 10% of the field, 2 = moderate lesions,
was cannulated with a PE tube (CH 10) to allow free
affecting 10–25%, 3 = severe, affecting 25–50%,
outflow of urine through an ureterocutaneostomy. Ten
4 = very severe, affecting 50–75%, and 5 = extensive
minutes after reperfusion, the renal microcirculation
damage, involvement of more than 75% of the field.
was reassessed. Postoperatively, the animals were
Immunohistochemical staining of paraffin sections
allowed free access to water and were supplemented
for von Willebrand factor (vWF) was performed as
with 1 L of 0.9% NaCl infusion IV. Ranitidine 50 mg
follows. After heat-mediated antigen retrieval by pre-
IV (Sigma–Aldrich Chemie GmbH) was administered
treatment in a pressure cooker for 20 min, sections
daily and postoperative analgesia was provided every
were incubated with rabbit polyclonal anti-vWF anti-
6–8 h with Tramadol (1 mg/kg IM) (Sigma-Aldrich
serum (ab6994, Abcam, Cambridge, UK) at a con-
Chemie GmbH) for up to 72 h after transplantation.
centration of 1:200 for 30 min at room temperature,
Ampicillin 500 mg (Sigma-Aldrich Chemie GmbH)
and subsequently incubated with biotinylated goat-
was administered IV perioperatively as well as on a
anti-rabbit antiserum, peroxidase-conjugated strepta-
daily basis during follow-up. Also, Aspirin 500 mg IV
vidin, and diaminobenzidine, and finally counter-
(Bayer AG, Leverkusen, Germany) was given twice
daily for the entire period of follow-up. Animals were
endothelial cells was determined semiquantitatively on
observed for 7 days after transplantation with daily
a scale of 0–3 for the following features: 0 = no
assessment of renal function. Creatinine clearance was
staining above background immunoreactivity in non-
calculated from 24 h urine production and serum cre-
endothelial cells, 1 = minor staining, 2 = moderate
atinine ((urine creatinine 9 24 h volume)/(serum cre-
staining, 3 = prominent staining.
atinine 9 24 9 60 min)). At day 7 posttransplant, thetransplanted kidney was removed for histologicalevaluation and animals were euthanized by injection of
T61 IV (Hoechst Roussel Vet, Wiesbaden, Germany).
Data are expressed as mean ± SD. Statistical anal-
ysis of kidney weights as well as MP parameters were
Noninvasive Assessment of Renal Microcirculation
performed using the repeated measurements analysis
The O2C combined Laser Doppler and flowmetry
of variance (RM ANOVA) followed by the Bonferroni
device was used to evaluate the microcirculation non-
posttest. Significant differences of the renal microcir-
invasively. Prior to left nephrectomy and 10 min after
culatory measurements at different time points within
reperfusion, capillary blood flow (flow, arbitrary units,
the groups were assessed using the Mann–Whitney
AU) and capillary blood flow velocity (velocity, AU)
U test. For renal function, area under the curve (AUC)
were simultaneously recordedat 2 and 8 mm tissue
was calculated individually using the GraphPad Prism
depths. At four predefined locations on the renal sur-
5.0 statistics package (GraphPad Software, San Diego,
face (cranially, medially, caudally, and laterally),
CA, USA). Statistical significance of differences
measurements were performed for 30 s each, to pre-
was assessed using the Mann–Whitney U test. A
vent the influence of regional heterogeneity and tem-
p value < 0.050 was considered statistically significant.
poral blood flow variations.
Histological Analysis
At euthanization, renal tissue specimens were fixed
Animal weights did not differ between the groups
in neutral 10% buffered formalin and embedded in
(MP25, 23.5 ± 4.6 kg; MP30, 26.3 ± 3.2 kg; p =
paraffin. Tissue injury was assessed on periodic acid-
0.201). All animals demonstrated normal renal func-
Schiff (PAS) stained 4 lm-thick sections by scoring
tion before the start of the experiments (serum creati-
glomerular damage (shrinking), tubular damage, infil-
nine; MP25, 1.09 ± 0.14 mg/dL; MP30, 1.13 ± 0.10
tration of inflammatory cells, interstitial edema and
mg/dL; p = 0.565). Cold ischemic times (CITs)
necrosis. Tubular damage was defined as dilatation,
of the groups were comparable (CIT, MP25, 20:32 h ±
denudation of the tubular basement membrane and
0:06; MP30, 20:28 h ± 0:17; p = 0.158). Also, times
vacuolization. Injury of each specimen was graded to
required for both anastomoses were comparable
the extent of region involvement in 10 randomly cho-
between the groups (MP25, 00:41 ± 0:08 min; MP30,
sen, nonoverlapping fields (original magnification,
00:40 ± 0:08 min; p = 0.847). At the end of the
9400). Injury was scored by a pathologist blinded for
500 mL washout, all kidneys showed a macroscopi-
the groups using a semi-quantitative score on a scale
cally asanguinous effluent.
DOORSCHODT et al.
Kidney weights after washout did not differ between
or the resistance as:
the groups (MP25, 66.0 ± 11.8 g; MP30, 72.3 ±
12.5 g; p = 0.369). Also, repeated measurement anal-
ysis of kidney weights after washout and after MPpreservation, did not differ between the groups (RM
For reasons of clarity we assumed that the vessel is a
ANOVA kidney weights, p = 0.209).
single duct with constant diameter. Using the meanflow at 10 h we estimated the shear stress on theendothelial wall as follows:
MP25: 25 mmHg = 3.33306 kPa
Data on perfusion parameters per 100 g kidney
weight are shown in Fig. Analysis of perfusion flow
showed a trend towards higher flow rates in the MP30
MP30: 30 mmHg = 3.99967 kPa
group, though not significant (RM ANOVA, MP25vs. MP30, p = 0.068, Fig. a). Overall, intravascular
resistance did not differ between the groups (RM
ANOVA, MP25 vs. MP30, p = 0.419, Fig.
The resistance per 100 g kidney weight is a function of
the geometry of the vessel and the viscosity of blood or
Perfusion Dynamics
the perfusion medium. The flow and renal resistance
The Hagen–Poiseuille law states that the volume
should be constant if the geometry and viscosity are un-
Q through a vessel with diameter d and length
changed. When we assume that the viscosity is the same
L is related to the pressure drop Dp by the equation
in both situations and the change of L can be neglected,we may conclude that the difference of the pressure drop
produces a change in diameter of the vessels leading to
the following ratio of the both values of the resistance.
where l is the dynamic viscosity of the fluid.
Blood is a two-phase fluid so that l is not strictly
constant but may decrease in vessels with diametersbetween 10 and 300 lm with decreasing diameters due
We can express this as an additional stretch k pro-
to the Fa˚hræus–Lindqvist effect. It occurs because
duced in the vessel by increasing the pressure from 25
erythrocytes move towards the center of the vessel
leaving plasma at the wall of the vessel. Introducing
the laminar resistance:
MP25 ¼ 1:092 ¼ 1:022
This corresponds to an additional Green–Lagrange
the pressure drop can be expressed by the equation:
" 1 ¼ 0:022 ¼ 2:2%
(a, b) Machine perfusion parameters. (a) Perfusion flow recorded during 20 h MP per 100 g kidney weight. (b) Intra-
vascular resistance during 20 h MP per 100 g kidney weight.
Perfusion Pressures During Machine Perfusion of Kidneys
The physiological systolic and diastolic pressures
precisely known. However, the estimated ratios repre-
are approximately 40 and 30 mmHg, respectively, in
sent the expected trends.
pre-capillary arterioles. Changes in diameter fromdiastole and systole depend strongly on the location of
Renal Microcirculation
the arteries, ranging from 1% for carotid artery to10.8% for main pulmonary artery. Although our
Overall, cortical microcirculatory flow at 2 mm tis-
simple approximation represents an average effect, it is
sue depth postreperfusion was better compared to
nevertheless in the range of the physiological values.
cortical microcirculatory flow preretrieval in both the
Accepting the effect that the pressure drop expands the
MP25 and the MP30 groups. (Capillary blood flow at
vessels, we could estimate the effect on wall shear
2 mm, postreperfusion vs. preretrieval, p < 0.001, and
Fig. a.) Capillary blood flow values assessed at 8 mm
postreperfusion did not differ from capillary blood
values preretrieval in both the MP25 and the MP30groups. (Capillary blood flow at 8 mm, postreperfu-
With the above assumptions the ratio between shear
sion vs. preretrieval, p = 0.565, and p = 0.393,
stresses shows a 18.6% reduction brought about by the
respectively, Mann–Whitney U test, Fig. All blood
16.7% reduction of the PP from 30 to 25 mmHg.
flow velocity measurements assessed postreperfusion
were higher compared to blood flow velocity mea-
surements preretrieval at both 2 and 8 mm tissue
depths in both the MP25 and MP30 groups. (Blood
flow velocity at 2 mm, postreperfusion vs. preretrieval;
MP25, p = 0.002 and MP30, p = 0.041; Blood flowvelocity at 8 mm, postreperfusion vs. preretrieval;
If the vessel diameter would be unchanged the ratio
MP25, p = 0.025 and MP30, p = 0.041, Mann–
would appear even more favorable for the MP25 case.
Whitney U test, Fig.
Directly after revascularization, macroscopically,
both the MP25 and the MP30 grafts showed a
The blood flow is nonlinear and therefore the ratios
may not be equal in all vessel diameters. The perfusion
Follow-up After Transplantation
medium finally has to flow through arterioles whichtypically have a diameter of approximately 25 lm so
In the MP30 group, 6 out of 7 animals survived
that the Fa˚hræus–Lindqvist effect applies. Therefore,
7 days. One animal in the MP30 group was killed at
the viscosity and shear stress very near a wall are not
postoperative day 2 since it was suffering from renal
(a, b) Renal microcirculation. (a) Capillary blood flow values at 2 mm and at 8 mm tissue depths, MP25 and MP30
groups (*p < 0.050, ***p < 0.001). (b) Blood flow velocity values at 2 and at 8 mm tissue depths, MP25 groups and MP30 (*p < 0.050,**p < 0.010).
DOORSCHODT et al.
failure, as demonstrated by rising creatinine levels. In
blood urea values in the MP25 group were lower
the MP25 group all animals survived 7 days. Survival
compared to peak blood urea values in the MP30
did not differ between the groups (Log rank test,
group (MP25, 104 ± 99 mg/dL; MP30, 241 ± 136
p = 0.317). Animals surviving the 7 day follow-up
mg/dL; p = 0.022). Times to peak blood urea in the
after transplantation were included in the postopera-
MP25 group were shorter compared to the MP30
tive analyses.
group (MP25, 3.3 ± 2.4 days; MP30, 5.7 ± 0.8 days;p = 0.049). At killing, blood urea values in the MP25group were lower than in the MP30 group (MP25,
75 ± 109 mg/dL; MP30, 197 ± 156 mg/dL; p = 0.022).
Overall, posttransplant serum creatinine values in
the MP25 group were lower than posttransplant serum
nephrectomy and prior to reperfusion did not differ
creatinine of surviving animals in the MP30 group
between the groups (p = 0.352). Overall, creatinine
(AUC serum creatinine, MP25 vs. MP30; p = 0.035,
clearances rates in the MP25 group were significantly
Fig. Peak serum creatinine levels were comparable
higher compared to creatinine clearance rates in
the MP30 group (AUC creatinine clearance; MP25
(MP25, 5.5 ± 5.4 mg/dL; MP30, 11.1 ± 2.9 mg/dL;
vs. MP30, p = 0.026, Fig.
p = 0.051). Times to peak serum creatinine did notdiffer between the groups (MP25, 2.9 ± 2.6 days;
Histological Examination
MP30, 5.2 ± 1.3 days; p = 0.149). At killing, serumcreatinine levels in the MP25 group were lower com-
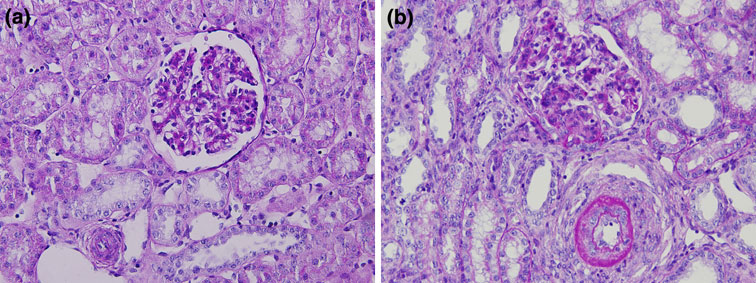
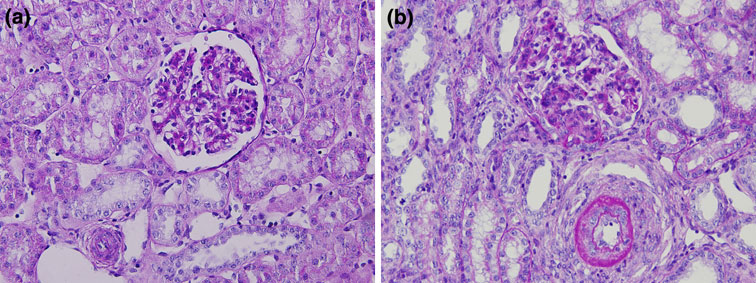
Overall, tissue injury of grafts in the MP25 group
pared to the MP30 group (MP25, 4.0 ± 5.8 mg/dL;
was significantly less compared to grafts in the MP30
MP30, 7.4 ± 3.2 mg/dL; p = 0.035).
group (Table ; Fig. ).
Posttransplant blood urea values in the MP25 group
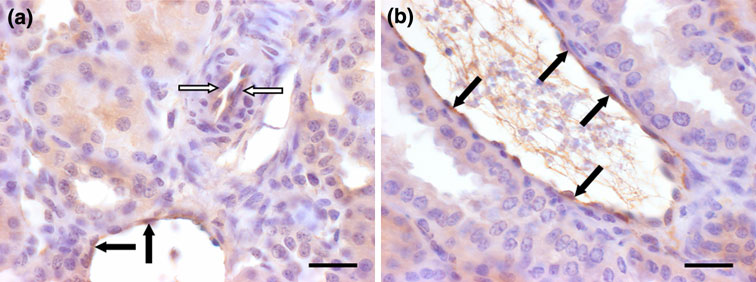
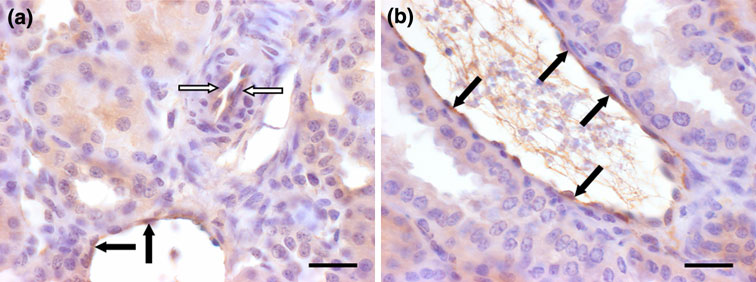
These findings were confirmed with the immuno-
were lower than posttransplant blood urea values of
histochemical staining (Fig. showing increased vWF
surviving animals in the MP30 group (AUC blood
in the MP30 group (average score 2.1) compared to the
urea; MP25 vs. MP30; p = 0.035, Fig. Also, peak
MP25 group (average score 1.4).
(a–c) Renal function. (a) Serum creatinine values posttransplant in the MP25 and the MP30 groups (AUC serum
creatinine, MP25 vs. MP30, p 5 0.035). (b) Blood urea levels posttransplant in the MP25 and the MP30 groups (AUC blood urea,MP25 vs. MP30, p 5 0.035). (c) Creatinine clearance rates posttransplant in the MP25 and the MP30 groups (AUC creatinineclearance rates, MP25 vs. MP30, p 5 0.026).
Perfusion Pressures During Machine Perfusion of Kidneys
deceased kidney grafts, MP holds the potential for atrue comebackIn the first large multi-center,
In the early days of kidney transplantation from
prospective, randomized clinical trial performed by
deceased donors, MP was the only preservation
Moers et al.,it was demonstrated that kidney grafts
method available.However, for over two decades, the
from standard as well as extended criteria donors
less cumbersome and inexpensive cold static storage
benefit from MP as the risk of delayed graft function
method has been the standard for preservation of
was significantly reduced.
kidney grafts. Following recent studies showing the
A recent preclinical study comparing hypothermic
beneficial effect of MP over CS preservation of
MP using either a high or low PP with CS, also showedthe advantage of MP over CS for the preservation ofporcine kidney grafts. In addition to better survivaldata when a PP of 30/20 mmHg was applied, less
Quantification of morphological data.
damage to the endothelial cells was observed when
compared to a PP of 60/40 mmHThe two non-surviving animals in the 60/40 mmHg group revealed
Glomerular shrinking
diffusely black colored grafts with patent arterial and
venous anastomoses suggesting impairment of intra-
renal circulation. It was concluded that the PP was of
critical importance for transplantation outcome.
Following the aforementioned reports and the
Semiquantitative scale: 0 = no injury; 1 = lesions affecting £10%
favorable results of the clinical trial in which a PP of
of the field; 2 = 10–25%; 3 = 25–50%; 4 = 50–75%; and 5 =involvement of >75% of the field. Data expressed as mean ± SD.
30 mmHg was applied, we investigated whether a
(a, b) Light microscopy. (a) MP25 group, well preserved glomerulus, moderate tubular dilatation, and interstitial
inflammation (original magnification 320, PAS stain). (b) MP30 group, moderate shrinking of glomerulus, simplification of tubularepithelium, few inflammatory cell infiltrates (original magnification 320, PAS stain).
(a, b) vWF immunohistochemistry. (a) MP25 case: there is only minor immunoreactivity slightly above background of
endothelial cells of both small (white arrows) and larger caliber blood vessels (black arrows). Scale bar 5 50 lm. (b) MP30 case:endothelial cells (arrows) of blood vessels of these kidneys often showed a prominent vWF immunoreactivity considerably abovebackground. Scale bar 5 50 lm.
DOORSCHODT et al.
mean PP of 25 mmHg could be advantageous over a
shown that intrarenal resistance fell to a baseline level
PP of 30 mmHg. The rationale of lowering the PP
after 4–6 h, and after this period, the formation of
originates from the common regard that pressure
edema increased rapidly. Also, from preclinical studies
induced endothelial damage is one of the main draw-
a time-dependent increase in vascular resistance was
backs associated with Also, the feasibility of
observed during prolonged hypothermic pulsatile per-
the new perfusion solution POLYSOL was evaluated.
By using a similar experimental model as Maathuis
Our study did not confirm these phenomena since,
et al., parameters of microcirculatory integrity, renal
function and morphology were assessed.
remained at a basement level for the duration of the
For assessment of the microcirculation, we used the
20 h perfusion period. A steady or decreasing intrare-
O2C Laser Doppler and flowmetry system. Major
nal resistance is considered a useful indication of graft
advantages of the O2C are the possibility to quanti-
viability, suggesting preservation of structural integrity
tatively assesses the microcirculation and frequent
of the endothelium and patency of the vascular
measurements. The O2C measures every other second
which results in accurate data. A disadvantage of the
Recently, experimental preservation studies were
method is that it can only measure blood flow at a
performed comparing CS to hypothermic MP of warm
small location since it is commonly known that graft
ischemically damaged kidney grafts. Hosgood et al.
injury can be distributed heterogeneously. To assure
applied a mean PP of 30 mmHg whereas in a study by
reliable assessment of the microcirculation, we per-
our group, a mean PP of 20 mmHg was applied in
formed 30 s measurements at four predefined locations
order to minimize the possibility of MP induced
on the renal surface. The results of our study confirm
endothelial injury which is aggravated by warm
earlier findings that lowering of the PP is advantageous
ischemia.In our study, the ratio between shear
since MP using a mean PP of 25 mmHg resulted in a
stresses shows a 18.6% reduction brought about by the
higher capillary blood flow at 10 min after reperfusion.
16.7% reduction from 30 to 25 mmHg. Hypertension
Moreover, histological evaluation showed better pres-
is a phenomenon that takes considerable time to pro-
ervation of structural integrity in the MP25 group.
voke renal disease. However, at the short time intervals
Overall, improvement in recovery of renal function
used in this study, we can assume that high wall shear
was seen in the MP25 group compared with the MP30
stress rates are the root cause for endothelial damage.
group. The effect of the POLYSOL solution does not
Reducing the PP from 30 to 25 mmHg has a beneficial
appear to be of importance, since the results of this
effect on the wall shear stress. This finding was con-
study resemble the results obtained in similar studies
using KPS-1.Also, POLYSOL meets the pre-
showed increased vWF expression in the MP30 group
requisites for an effective MP solution as postulated by
compared to the MP25 group. The expression of vWF
Belzer et al.; the presence of a colloid, impermeants
is known to be higher in renal endothelial cells of
and extracellular electrolyte concentration.
patients with hypertension, acute, and chronic renal
Before starting this study, we performed a pilot
study using mean PP's of 40 and 35 mmHg duringpulsatile perfusion of porcine kidney grafts (data not
shown). In contrast to the studies by Nicholson et using a mean PP of 60 mmHg and M(mean
In a porcine autotransplantation model, MP of
PP approximately 50 mmHg), in our pilot study, none
renal grafts with the novel AIRDRIVE MP system
of the animals (n = 3) survived the intended 7 day
using a mean PP of 25 mmHg is preferred over a mean
follow-up after autotransplantation. In all three
PP of 30 mmHg. These results corroborate earlier
experiments, kidney failure, as demonstrated by a steep
studies suggesting a direct effect of the PP applied
rise of creatinine levels, was observed resulting in
during MP on vascular injury and organ viability.
premature killing of the animals. Histological exami-nation of the grafts showed severe tubular injury andnecrosis in all sections which was considered a result of
long-term renal hypertension. Although the mean PPsapplied were lower than human and porcine physio-
The authors would like to thank Mario Sitzia, Wei
logical pressure levels, endothelial damage is likely to
Lai, Mareike Schulz, and Ute Lohmer for their con-
occur even at mean PPs of 50–60 mmHg since hypo-
tinuous support. This study was in part sponsored by
thermia severely increases cell membrane stiffne
Doorzand Medical Innovations BV, Amsterdam, The
According to Nicholson et al. a period of 6 h perfusion
Netherlands (the company ceased operations as per
preservation was chosen as previous experience had
August 2008).
Perfusion Pressures During Machine Perfusion of Kidneys
J. J. Weening, and S. Florquin. Renal-associated TLR2mediates ischemia/reperfusion injury in the kidney. J. Clin.
Invest. 115:2894–2903, 2005.
Balupuri, S., P. Buckley, M. Mohamed, C. Cornell,
15Maathuis, M. H., S. Manekeller, A. van der Plaats,
D. Mantle, J. Kirby, D. M. Manas, and D. Talbot.
H. G. Leuvenink, N. A. ‘t Hart, A. B. Lier, G. Rakhorst,
Assessment of non-heart-beating donor (NHBD) kidneys
R. J. Ploeg, and T. Minor. Improved kidney graft function
for viability on machine perfusion. Clin. Chem. Lab. Med.
after preservation using a novel hypothermic machine
perfusion device. Ann. Surg. 246:982–988, 2007.
Belzer, F. O., B. S. Ashby, P. F. Gulyassy, and M. Powell.
16Matsuno, N., E. Sakurai, I. Tamaki, K. Furuhashi,
Successful seventeen-hour preservation and transplanta-
A. Saito, S. Zhang, K. Kozaki, A. Shimada, K. Miyamoto,
tion of human-cadaver kidney. N. Engl. J. Med. 278:608–
and M. Kozaki. Effectiveness of machine perfusion pres-
ervation as a viability determination method for kidneys
Belzer, F. O., B. Ashby, J. S. Huang, and J. E. Dunphy.
procured from non-heart beating donors. Transplant. Proc.
Etiology of rising perfusion pressure in isolated organ
perfusion. Ann. Surg. 168:382–391, 1968.
Moers, C., J. M. Smits, M. H. Maathuis, J. Treckmann,
Brook, N. R., A. J. Knight, and M. L. Nicholson. Intra-renal
F. van Gelder, B. P. Napieralski, M. Van Kasterop-Kutz,
resistance reflects warm ischaemic damage, and is further
J. J. van der Heide, J. P. Squifflet, E. Van Heurn,
increased by static cold storage: a model of non-heart-
G. R. Kirste, A. Rahmel, H. G. Leuvenink, A. Paul,
beating donor kidneys. Med. Sci. Monit. 9:271–275, 2003.
J. Pirenne, and R. J. Ploeg. Machine perfusion or cold
Doorschodt, B. M., M. Bessems, A. K. van Vliet, and
storage in deceased-donor kidney transplantation. N. Eng.
T. M. van Gulik. The first disposable perfusion preserva-
J. Med. 360:7–19, 2009.
tion system for kidney and liver grafts. Ann. Transplant.
18Nicholson, M. L., S. A. Hosgood, M. S. Metcalfe,
9:40–41, 2004.
J. R. Waller, and N. R. Brook. A comparison of renal
Fuller, B. J., and C. Y. Lee. Hypothermic perfusion pres-
preservation by cold storage and machine perfusion using a
ervation: the future of organ preservation revisited? Cryo-
porcine autotransplant model. Transplantation 78:333–337,
biology 54:129–145, 2007.
Fung, Y. C. Biomechanics. Circulation (2nd ed.). New
19Pusztaszeri, M. P., W. Seelentag, and F. T. Bosman.
York: Springer, 1997.
Immunohistochemical expression of endothelial markers
Garfield, S. S., A. W. Poret, and R. W. Evans. The cost-
CD31, CD34, von Willebrand Factor, and Fli-1 in normal
effectiveness of organ preservation methods in renal
human tissues. J. Histochem. Cytochem. 54(4):385–395,
transplantation: US projections based on the machine
preservation trial. Transplant. Proc. 41:3531–3536, 2009.
Schreinemachers, M. C., B. M. Doorschodt, S. Florquin,
Gattone, V. H., R. S. Filo, A. P. Evan, S. B. Leapman,
M. A. van den Bergh Weerman, J. B. Reitsma, W. Lai,
E. J. Smith, and F. C. Luft. Time course of glomerular
M. Sitzia, T. M. Minor, R. H. Tolba, and T. M. van Gulik.
endothelial injury related to pulsatile perfusion preserva-
Improved preservation and microcirculation with POLY-
tion. Transplantation 39:396–399, 1985.
SOL after transplantation in a porcine kidney autotrans-
Groen, H., C. Moers, J. M. Smits, J. Treckmann,
plantation model. Nephrol. Dial. Transplant. 24:816–824,
D. Monbaliou, A. Rahmel, A. Paul, J. Pirenne, R. J. Ploeg,
and E. Buskens. Long-term cost-effectiveness of hypo-
21Schreinemachers, M. C., B. M. Doorschodt, S. Florquin,
thermic perfusion versus cold storage in kidney transplan-
M. A. van den Bergh Weerman, A. Zernecke, M. M. Idu,
tation. Am. J. Transplant. 9(Suppl 2):227, 2009.
R. H. Tolba, and T. M. van Gulik. Pulsatile perfusion
Hoffmann, R. M., J. H. Southard, M. Lutz, A. Mackety,
preservation of warm ischaemia-damaged experimental
and F. O. Belzer. Synthetic perfusate for kidney preserva-
kidney grafts. Br. J. Surg. 97:349–358, 2010.
tion: its use in 72-hour preservation of dog kidneys. Arch.
22St Peter, S. D., C. J. Imber, and P. J. Friend. Liver and
Surg. 118:919–921, 1983.
kidney preservation by perfusion. Lancet 359:604–613,
Hosgood, S., B. Yang, A. Bagul, I. H. Mohamed, and
M. L. Nicholson. A comparison of hypothermic machine
23Szust, J., L. Olson, and L. Cravero. A comparison of OPO
preservation versus static cold storage in an experimental
pulsatile machine preservation practices and results.
model of renal ischemia reperfusion injury. Transplantation
J. Transpl. Coord. 9:97–100, 1999.
89:830–837, 2010.
Treckmann, J., M. Nagelschmidt, T. Minor, F. Saner,
Krug, A. Mikrozirkulation und Sauerstoff versorgung des
S. Saad, and A. Paul. Function and quality of kidneys after
Gewebes, Methode des so genannten O2C (oxygen to see).
cold storage, machine perfusion, or retrograde oxygen
Phlebologie 36:300–312, 2007.
persufflation: results from a porcine autotransplantation
Leemans, J. C., G. Stokman, N. Claessen, K. M. Rouschop,
model. Cryobiology 59:19–23, 2009.
G. J. Teske, C. J. Kirschning, S. Akira, T. van der Poll,
Source: http://www.cats.rwth-aachen.de:8080/~mb/article-AnBiomedEng_2010.pdf
OJ/S S13923/07/2014 Member states - Supply contract - Contract notice - Open procedure This notice in TED website: United Kingdom-Larkhall: Pharmaceutical products Directive 2004/18/ECSection I: Contracting authorityI.1) Name, addresses and contact point(s)The Common Services Agency (more commonly known as NHS National Services Scotland) (‘the Authority')National Procurement, Canderside, 2 Swinhill AvenueContact point(s): National ProcurementFor the attention of: Stuart GillespieML9 2QX LarkhallUNITED KINGDOMTelephone: +44 1698794585Internet address(es): Address of the buyer profile: Electronic submission of tenders and requests to participate:Further information can be obtained from: The above mentioned contact point(s)Specifications and additional documents (including documents for competitive dialogue and a dynamicpurchasing system) can be obtained from: The above mentioned contact point(s)Tenders or requests to participate must be sent to: The above mentioned contact point(s)
Influenza Pandemic Ten Things You Need To Know About Pandemic Influenza 1. Pandemic influenza is different 5. Widespread illness will occur from avian influenza Because most people will have no immunity to the Avian influenza refers to a large group of different pandemic virus, infection and illness rates are expected to