Bimehc

Technical and pictorial file
Table of content
Executive summary
Background information
Major areas of intervention
Vision and mission
Geografical location
Modernisation of the centre
Health care facilities
Occupational therapy and income generating facilities
Support facilities
Preparation of traditional medicine
Function of the centre
Statistics in mental health (traditional and modern)
Frequencyof hospitalisation
Frequency of external consultation
Prevelance of mental illnesses in BIMEHC
Most prescribed psychiatric medication
Partner organisations
Conclusion and perspectives
WHO: Seven good reasons for integrating mental health into primary care
Summary
Cameroon has just few government run mental health care facilities.
Babungo Integrated Mental Health Care (BIMEHC) is a traditional/modern mental and
primary health care facility in the Ngoketunjia Division in the North West Region.
The variety of care, therapies and income generating activities as well as the comfortable,
hygienic housing facilities offers a unique and therapeutic setting to treat people with mental
disorders and basic health problems.
BIMEHC has the facilities and capacity to function as a training center for community based
integrated health care. Collaboration with the government would serve the disadvantaged
people, staffs in training (both medical and paramedical) and the promotion of mental health
enormously.
BIMEHC can help to realise the goals that are mentioned in the Strategic Planning of the
Ministry of Public Health 2001-2015.
I-Introduction
Cameroon has few government run mental health facilities to care for psychiatric patients
(Hôpital Jamot Yaoundé and Laquintinie in Douala), where the few psychiatrists are working.
In nearly all the regions, the mental health units in the Regional Hospitals are not functional
due to a lack of specialised staff. Traditional practitioners try to fill the gap and are treating
mental health patients; often to no avail.
The lack of sufficient mental health facilities in Cameroon in general and the North West
Region more specific justifies a setup like Babungo Integrated Health Care (BIMEHC). It is a
reality that Cameroon's population values/frequents visits to traditional healers
The integrated combination of traditional and modern psychiatric care and basic health care
in BIMEHC fills the gap that is tangible in Cameroonian communities.
WHO states that integrated care helps to reduce the stigma associated with seeking help
from stand-alone mental health services. An integrated service encourages the early
identification and treatment of such disorders and thus reduces disability. Among other
possible benefits are the provisions of care in the community and opportunities for
community involvement in care ¹
¹The mental health context. Geneva, World Health Organization, 2003 (Mental Health Policy
and Service Guidance Package).
II- The way forward
There is a necessity to reinforce and reorganize the national system of mental health.
Building new hospitals in other parts of the country would imply huge budgets. More efficient
is exploiting the existing means and improve them systematically.
BIMEHC has a proven record of being successful in integrating mental and basic health care
in the community and can therefore serve as an example for future projects.


III- Background information
The founder of BIMEHC, Pa Mathias TUMENTA (1935-2009), started in 1959
treating his first patients traditionally.
In 1989, he was granted an official recognition from the government as a traditional
In 2001, Charity Health Foundation (registration number LT/GP/30/01/3399) took the
traditional home as an annex to carry out primary health care with modern medication.
In June 2003, a Dutch VSO (Voluntary Services Overseas) volunteer took up a
placement, which was succeeded by a Kenyan VSO volunteer in September 2006, Currently the Dutch VSO volunteer and a UK VSO volunteer are working in BIMEHC.
The home was registered as a Common Initiative Group in May 2004 with
registration number NW 30/04/8492 with the name Babungo Integrated Health Care (BIHC).
Since the end of 2003 BIMEHC has developed itself enormously. Through national
and international assistance; the infrastructure improved drastically.
Papa Matthias Tumenta Wambo (1935-2009) founded a traditional psychiatric home in the early sixties. In 2004 BIMEHC was registered as a CIG.
Tweke John Tumenta General Manager BIMEHC
(community nurse and traditional
IV-The major areas of intervention:
modern and traditional mental health care primary health care health education support programme for People Living With HIV & AIDS (PLWHA)
Activities are expanded to cover other areas such as Human Rights and advocacy for
underprivileged groups, income generating activities, capacity building workshops,
watershed protection, sustainable agriculture, entrepreneurship, education and livelihoods.
Target group
• People with a mental health problem • People in need for primary health care • People living with HIV&AIDS • Vulnerable children and orphans




Psychiatric wards
Patients shared rooms, slept on broken bamboo beds with grass matresses and cooked inside the rooms
Primary Health Care
Consultation room
Pharmacy and dressing room
V- Vision and mission.
Vision: A society in which, all persons, especially the underprivileged, are accepted and
have access to basic health care, economic resources and social facilities enabling them to
live a satisfying life.
Mission: To contribute to this vision we engage in domains such as the provision of mental
and primary health care for the poor; empowerment of underprivileged groups, sensitisation
of communities, promotion of sustainable agriculture and income generating activities. We
establish this through health care services, training, research, public - private partnerships
and international relations.
BIMEHC recognizes that its vision and mission can only be successfully achieved with a qualified, devoted and experienced staff working on issues developed with the active participation of the beneficiaries.
Respect for fundamental human rights Assurance of equal opportunity for all persons irrespective of ethnicity, religion, age
Professional integrity, transparency and accountability Teamwork and collaboration
VI- Objectives
Main objective:
to promote and provide traditional and modern mental and primary health care for
disadvantaged groups in Cameroon.
Specific objectives:
To promote access to mental and primary health care for disadvantaged groups To holistically assist and care for people with mental health and primary health care
problems and their families by the use of traditional and conventional medicine and approach.
To assist and equip people with mental health problems and HIV&AIDS with skills
and knowledge to facilitate their reinsertion and reintegration in society
To support income generating activities for these underprivileged groups To promote food security and sustainable agriculture To support education of the children from the underprivileged homes with focus on
To advocate for mental health and the prevention of HIV&AIDS To enhance the protection of the medicinal garden and the natural resources To collaborate with the Faculty of Medicine and Biomedical Sciences, the Training
school for psychiatric nurses in Yaoundé and other mental health training institutions.
To expand the frontiers as training, research and resource centre to the public and
other mental health associations.
To build the capacity of the association's staff To support education of the children from the underprivileged homes with focus on
Global y, BIMEHC's strategy focuses on a combination of local and external resources to enable local people, especially the poor and underprivileged to improve their own conditions of life. Gender is mainstreamed in all its endeavours.
Essentially its strategy includes:
The setting up and maintenance of basic health care facilities (mental and primary
Capacity building of the staff Target group involvement at all levels of the project cycle Seed centre, processing and demonstration units (piggery, poultry and gardening) Training, demonstrations and follow up Human rights and Advocacy Networking and maintaining collaborative partnerships with local and international
VIII- Human resources
1 General Manager 2 SR nurses (1 is a volunteer) 1 Laboratory technician 1 General Practioner (once a week) 1 Psychiatrist (monthly consultation) 1 Herbal/Convential pharmacist 1 Administrator 1 Project coordinator (medicial antropologist/sociologist) 1 Herbalist 3 Support staff 1 hotel/catering staff 2 International volunteers (psychiatric nurse/sociotherapist and management
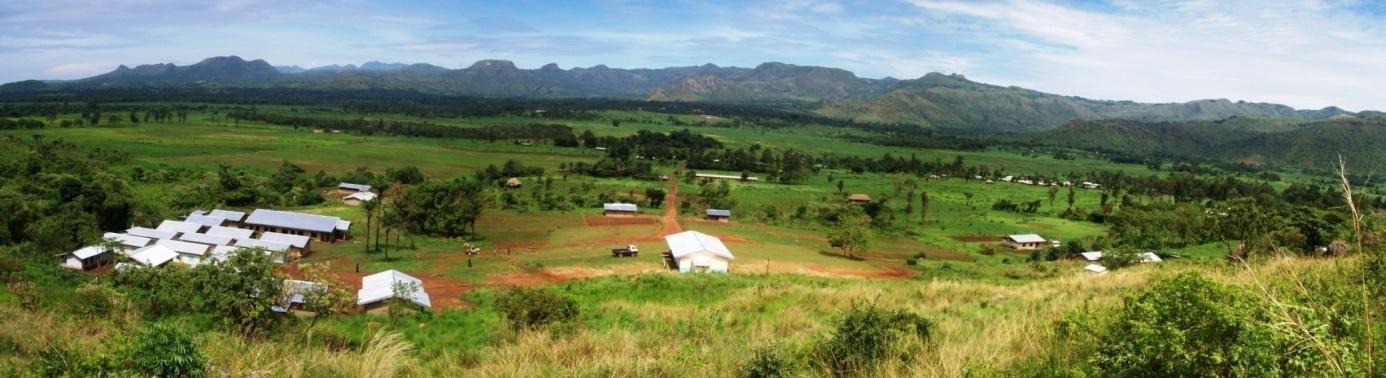
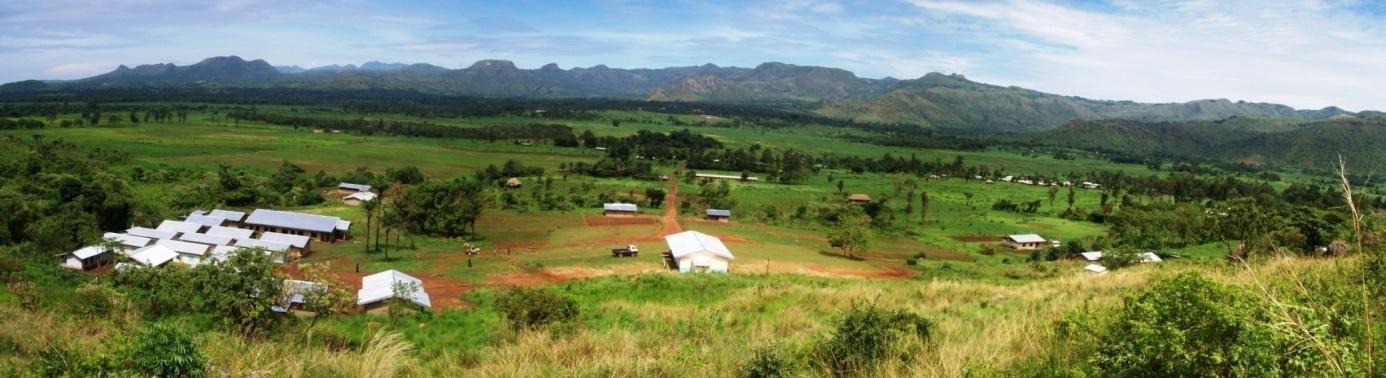
IX- Geographical location
The centre lies on a surface of 5 hectares on the foot of a mountain offering a
panoramic view of mountain chains with a waterfall, a panoramic view of rice field
cultivation of Ndop.
The centre is crossed by two rivers producing a sonore and beautiful atmosphere of water clapotis.
All along the year, the climate is cold and a bit humid offering an ideal setup for the recovery and rest of mental patients and people tired by their activities.
The presence of many bird species offers a musical boom during the first hours of the morning. Centre isolated (at 10 km from Ndop on the ring road towards Kumbo), away from sound pollution and which offers a calm surrounding, appeasing, restfully and therapeutic.
The new Primary Health Care facility
X - Modernisation of the centre
Plurality of availability of care, health democracy of care in BIMEHC: an answer to
medical nomadic health seeking behaviour.
A. Health care facilities:
Construction of modern buildings since 2005:
pro-pharmacy laboratory and examination room consultation room both in and outpatients maternity room treatment room duty room store rooms 54 beds for psychiatric patients 32 beds for the section of PHC psychotherapy hall for individual, couple and family therapy herbal pharmacy (drying,
preparation and store rooms)
Psychiatric wards: each room has two beds for the patient and the carer
Consultation rooms and duty room
Every room has 2 beds, one for the patient and one for the carer. It is not allowed to cook inside.
B. Occupational therapy and income generating facilities:
Multidisciplinary hall (occupational therapy, sanitary and health education, seminars,
conferences, formation of staff, leisure activities, church)
restaurant for patients, carers, staff and visitors piggery house poultry house grinding mill and feed store house field for outdoor games and sport medicinal plants and vegetable garden
C. Support facilities
7 lodging houses for personnel 4 guesthouses (28 beds for passerby tourists, visitors and international volunteers) restaurant for patients, carers, staff and visitors administrative block (3 rooms) souvenir shop with creative works from (ex)patients 8 toilet/bathroom blocks indoor and outdoor kitchen primary school solar energy installation for the health care centre, staff quarter and guesthouses
(also to assure cold chain for vaccines)
Community hall is being used for health education, workshops and leisure activities.
Administrative block and psychotherapy room
Patients and carers have the choice to use the canteen or cook for themselves in the indoor or outdoor kitchen.
Piggery and poultry
Income generating activities are also used as occupational therapy
D. Preparation of traditional medicine
• Garden of psychotropic medicinal
plants at the premises of BIMEHC.
Drying and storage of medicinal plants in shaded room
Daily fresh preparation of concoctions and st
orage in the refrigerator
Guesthouses and international volunteer lodging facilities
XI- Function of the centre
mental health care preventive and curative care rehabilitation and reinsertion community based care psychotherapy and conflict resolution referral system and contra referral vaccination programme health education programme of telemedicine (tele-psychiatry) HIV&AIDS support group microfinance activities for disadvantaged groups
XII- Statistics in mental health (traditional and modern)
A. Frequency of hospitalisation:
one week observation and diagnostics stabilising patients with traditional and modern medication average hospitalisation is about 3 to 6 months monthly follow up after discharge average of 20 psychiatric inpatients
B. Frequency of external consultation
average of 450 patients per year
C. Prevalence mental illnesses in BIMEHC
Depression Schizophrenia Bipolar disorder Acute psychosis Toxicomania Obsessive compulsive disorder Phobia Hysteria Post natal depression Epilepsy Dementia
D. Most prescribed psychiatric medication:
Antipsychotics:
Largactil® (Chlorpromazine)
Modecate® (Fluphenazine deconoate)
Haldol® (Haloperidol)
Risperdal® (Risperidon)
Mood stabilizers:
Tegretol® (Carbamazepine)
Depakine
Benzodiazepines:
Temesta® (Lorazepam)
Valium® (Diazepam)
Tranxene® (clorazapinezuur)
Antidepressants:
Anafranil® (Clomipraminehydrochloride)
Prozac® (Fluoxetine)
Corrector:
Artane® (Trihexyfenidyl)
Akineton® (Biperideen)
XIII- Partner organisations
National:
Habitat for Humanity Cameroon Soeur Hospitalier du Sacré Coeur de Jésus, Benoît Menni PRTC Fonta Development for Humanity Cameroon Government units (Ndop district hospital) Care Help Cameroon
International:
Babungo Foundation (Netherlands) Voluntary Services Overseas (VSO)
XIV- Conclusion and perspectives
Care : community based mental and primary health care
Training: Practical formation, academic stage, research and impregnation stages:
practical internships for students in medicine and psychiatry. Internships for paramedical students: psychology, sociology, psychiatric nurses and state registered nurses.
Research: Operational research in mental health (DPS, DLM, DRO)
International partnership: Tele-psychiatry (Switzerland, the Netherlands).
Advocacy: contribution to the promotion of mental health.
Intersectional collaboration: health-social welfare-agriculture-economy-education
Contact details
General Manager:
Tweke John Tumenta
Babungo Integrated Mental Health Care (BIMEHC)
Babessi subdivision
North West Region, Cameroon
(+237) 79834047 / 98328062
Website: Registration number: BIHC: NW/GP/30/04/8492
ANNEX
Seven good reasons for integrating mental health into primary care²
1. The burden of mental disorders is great.
Mental disorders are prevalent in all societies. They create a substantial personal burden for
affected individuals and their families, and they produce significant economic and social
hardships that affect society as a whole.
2. Mental and physical health problems are interwoven.
Many people suffer from both physical and mental health problems. Integrated primary care
services help ensure that people are treated in a holistic manner, meeting the mental health
needs of people with physical disorders, as well as the physical health needs of people with
mental disorders.
3. The treatment gap for mental disorders is enormous.
In all countries, there is a significant gap between the prevalence of mental disorders, on one
hand, and the number of people receiving treatment and care, on the other hand. Primary
care for mental health helps close this gap.
4. Primary care for mental health enhances access.
When mental health is integrated into primary care, people can access mental health
services closer to their homes, thus keeping their families together and maintaining their daily
activities. Primary care for mental health also facilitates community outreach and mental
health promotion, as well as long-term monitoring and management of affected individuals.
5. Primary care for mental health promotes respect of human rights.
Mental health services delivered in primary care minimize stigma and discrimination. They
also remove the risk of human rights violations that can occur in psychiatric hospitals.
6. Primary care for mental health is affordable and cost effective.
Primary care services for mental health are less expensive than psychiatric hospitals, for
patients, communities and governments alike. In addition, patients and families avoid indirect
costs associated with seeking specialist care in distant locations. Treatment of common
mental disorders is cost effective, and investments by governments can bring important
benefits.
7. Primary care for mental health generates good health outcomes.
The majority of people with mental disorders treated in primary care have good outcomes,
particularly when linked to a network of services at secondary level and in the community.
² Integrating mental health into primary care, a global perspective. Geneva, World Health
Organization & World Organization of Family Doctors, 2008
Source: http://www.q-fin.de/wp-content/uploads/2013/07/Technical-and-pictorial-file-presentation-BIMEHC.pdf
North American Tour Presented in association with UCLA Film & Television Archive and supported in part by grants from the Getty Foundation and The Andy Warhol Foundation for the Visual Arts. The series is curated by Al yson Nadia Field, Jan-Christopher Horak, Shannon Kelley, and Jacqueline Stewart. The Andy Warhol Foundation for the Visual Arts L.A. RebeLLioN Comes Home
Direction Régionale de la Concurrence, Lignes Direccte de la Consommation,du Travail et de l'Emploi de Basse-Normandie Publication trimestrielle de la Direction Régionale des Entreprises, de la Concurrence, de la Consommation, Conjoncture du Travail et de l'Emploi de Basse-Nor Le Bâtiment et la construction durable – Plan Bâtiment Grenelle Le Bâtiment en Basse-Normandie, ce sont 4 748 entreprises