Microsoft word - ivf manual 2004 2004.doc

ASSISTED REPRODUCTIVE TECHNOLOGY PROGRAM
PATIENT MANUAL
WILLIAM P. HUMMEL, M.D.
L. MICHAEL KETTEL, M.D.
SAN DIEGO FERTILITY CENTER
Making Dreams Come True …
IVF PROGRAM
Patient Manual
WILLIAM P. HUMMEL, M.D.
L. MICHAEL KETTEL, M.D.
Copyright 2004 by San Diego Fertility Center Medical Group, Inc.
San Diego Fertility Center
TABLE OF CONTENTS
WELCOME.4
IVF PROGRAM .5
ART ASSISTED REPRODUCTIVE TECHNOLOGY.6
MEET THE EXPERTS.7
BEFORE YOU START.9
MALE INFERTILITY .12
STARTING YOUR IVF CYCLE .14
IN VITRO FERTILIZATION EXAMPLE CALENDAR.14
MEDICATIONS .17
OVARIAN STIMULATION.19
IVF PROCEDURE .22
EGG RETRIEVAL.22
GIFT PROCEDURE .23
SEMEN COLLECTION INSTRUCTIONS .24
POST EGG RETRIEVAL/GIFT INSTRUCTIONS .24
EMBRYOLOGY LAB UPDATES & EMBRYO GRADING.25
EMBRYO TRANSFER .29
PROGESTERONE .30
PREGNANCY TEST.31
POST IVF APPOINTMENT .31
FROZEN EMBRYO TRANSFER (FET) CYCLE .32
A POSITIVE PREGNANCY TEST!.34
QUESTIONS AND ANSWERS.35
IMPORTANT REMINDERS DURING YOUR CYCLE.37
THE EMOTIONAL ASPECTS OF INFERTILITY .38
GLOSSARY .39
San Diego Fertility Center


elcome to the Assisted Reproductive Technology (ART) program of
the San Diego Fertility Center (SDFC), one of the leading In Vitro Fertilization (IVF) programs in the United States. When SDFC began its Assisted Reproductive Technology program in 1990, we knew that the decision to proceed with assisted reproduction would be one of the toughest choices a couple could face. ART may feel like a big step. It seems that there is an overwhelming amount of information, and people usually have lots of questions as they sort through it all. We needed to provide our patients with this important information and make it convenient and easy to understand. so we made this patient handbook. It will answer most of your questions and give you a good idea of what to expect during your IVF cycle. This manual is intended to be a workbook so you can jot down any questions you have, or take notes during appointments. Our hope is that this manual will provide you with our commitment to the highest quality in IVF fertility care. We invite and encourage spouses or partners to attend as many of the appointments as possible. You can provide a tremendous amount of support to each other during infertility testing and procedures. We also encourage your partner to perform your injections. Not only will this save time and money, but also it provides an opportunity for partners to be more involved in the treatment cycle. We look forward to working with you to achieve your goal of a successful pregnancy and a healthy baby!
L. Michael Kettel, M.D.
William P. Hummel, M.D.
San Diego Fertility Center

IVF PROGRAM
San Diego Fertility Center
ART
ASSISTED REPRODUCTIVE TECHNOLOGY
ART is a term used to describe advanced infertility therapies, most commonly IVF (In Vitro Fertilization) and GIFT (Gamete Intrafallopian Transfer), but it also includes other techniques such as ZIFT (Zygote Intrafallopian Transer) and FET (Frozen Embryo Transfer). These procedures all involve the removal of a woman's eggs from her ovaries, processing these eggs with sperm, and returning the eggs to the woman, sometimes already fertilized, in order to achieve pregnancy. The differences in these procedures involve where the eggs become fertilized, and how far along the fertilization process has progressed before they are returned to the woman's uterus.
During IVF, the eggs and sperm are taken to the laboratory and allowed to incubate together for
several days. The fertilized eggs, now called embryos, are returned to the woman's uterus
through the cervix. GIFT requires the immediate return of the eggs and sperm (gametes) to the
woman's fallopian tubes, and it is here that fertilization takes place. The embryos will proceed
down the fallopian tubes into the uterus in the usual manner.
The San Diego Fertility Center also offers the latest advanced techniques available, such as intracytoplasmic sperm injection (ICSI), assisted hatching, blastocyst transfer, egg donation, and surrogacy in order to provide a full scope of services to optimize your outcome.
Our physicians will carefully and thoroughly review your medical history with you to determine the procedure most appropriate for achieving your goal of a pregnancy. Several factors of your medical history will be considered, and additional testing may be requested prior to determining the appropriate treatment for you and your partner. On occasion, an alternative treatment plan may be recommended.
After your doctor establishes your treatment plan, you will meet with one of our administrative personnel to discuss the financial aspects of your procedure. You will be advised of any required pre-procedure testing and given lab slips for these tests. Once your testing is completed, you will then begin working closely with our nurse practitioners to coordinate your upcoming ART cycle.
The IVF process from the start of medication until egg retrieval takes approximately 4-6
weeks. Monitoring your response to these medications will require several office visits prior to
your procedure. Ovarian stimulation monitoring is performed at the San Diego Fertility Center
with aspiration of the eggs or GIFT, and embryo transfers accomplished in our new state-of-the-
art surgery center next door.
San Diego Fertility Center

MEET THE EXPERTS
Dr. Kettel (l.) and Dr. Hummel (r.)
The San Diego Fertility Center
Dr. William P. Hummel founded The San Diego Fertility Center in 1989 and is Board
Certified in OB/GYN and a specialist in Reproductive Endocrinology and Infertility. Dr.
Hummel has received extensive training in the most advanced methods of fertility treatment and
published extensively on the subject of IVF and advanced reproductive technology.
Dr. L. Michael Kettel is a Board Certified Reproductive Endocrinologist who joined Dr.
Hummel at the San Diego Fertility Center in 1996. From 1989 through 1996, Dr. Kettel was the
director of Infertility Services at UCSD and has published over 100 articles, book chapters and
abstracts on the use of assisted reproductive technology and the treatment of other disorders
which can lead to infertility
Chris M. O'Kane, R.N., C.N.P. is a Certified Nurse Practitioner with special recognition for
her expertise in the care of patients with infertility. She has over 20 years of experience in the
diagnosis and treatment of infertility. Her exceptional skills, which are unique to the San Diego
area, help to provide patients of the San Diego Fertility Center with the finest medical care
available. She will assist in coordinating your upcoming ART procedure.
Caroline L. Conner, R.N.C., S.M.N., W.H.N.P.-C. graduated from Vanderbilt University
School of Nursing with her Masters of Science in Nursing, and her Women's Health Nurse
Practitioner Certificate. She has been working in the field of Women's Health since 2002. She
started at SDFC in 2004 and is a great addition to our team.
San Diego Fertility Center
Tammi L. Massaglia, M.S.N., M.P.H., R.N., has a Masters degree in nursing and is one of the
Center's ART Coordinators. With over 8 years experience in the fertility field, she is highly
qualified and skilled in the management and treatment of the health care needs of women. Her
experience and commitment to the treatment of patients with infertility and to the mission of the
team at San Diego Fertility Center make her a valued member of the team. She is also the
Clinical Research Specialist handling all clinical research studies for the Center.
Lisa Souza, R.N., MBA, is a registered nurse and the CEO of the San Diego Fertility Center.
She shows her valuable skill and experience of over 15 years in the exceptional medical
treatment of our patients as well as the excellent management of the business center. She is
always available to listen to your concerns in hopes that we can resolve any issues that may
arise and improve what we do.
William C. Venier, M.Sc. is our senior embryologist. With over 16 years of experience, he is
highly trained and skilled in the advanced technique of micromanipulation including
intracytoplasmic sperm injection (ICSI) at the San Diego Fertility Center. His training and
experience reaches from New York, Australia, London to San Diego. He is the only
embryologist in San Diego with a graduate degree in Human Reproductive Biology.
Kathy Smith, B.S. is one of our embryologists. She has a B.S. in Physiology-Neurobiology
from the University of Maryland, College Park and is currently pursuing her Masters Degree in
Embryology and Andrology from Eastern Virginia Medical School. She has 5 years experience
in infertility treatment, including responsibilities as an embryology lab supervisor in a private
physician's office and as an embryologist and andrology supervisor at Union Medical Hospital
in Baltimore. She is also highly skilled in micromanipulation, including ICSI and assisted
hatching.
Shannon Lee, B.S. is one of our embryologists. She earned her Bachelors Degree from the
University of San Diego, California in General Biology with an emphasis in Human
Reproduction. Currently, she is pursuing her Masters Degree in Embryology and Andrology
from Eastern Virginia Medical School. Before joining SDFC, she worked at UCSD as a Lab
Technician, researching cell-to-cell communication and differentiation.
We want to help you achieve your goal
We are pleased that you are interested in the San Diego Fertility Center as a partner in your
search for solutions to infertility. Dr. Hummel, Dr. Kettel and the entire staff wish to provide
you with the personal attention you deserve and the best medical care available today!
San Diego Fertility Center
BEFORE YOU START.
Insurance Coverage and Fees
Fees will vary according to your treatment plan and your response to the medications. We look forward to meeting with you in person to review the fees involved, and discuss any options available to you. Financial advisors are available to assist you.
Embryology Presentation
We highly recommend that you and your partner attend our monthly presentation, given by our embryology team, called "The Mystery behind the Microscope." They will review ICSI, assisted hatching, fertilization, embryo grading and more.
Preconception Health
Smoking is absolutely contraindicated during pregnancy and may result in an increased risk of
premature labor, intrauterine growth retardation as well as other complications. Studies have
shown that smoking may decrease fertility by 30%. We strongly feel that if you smoke, you
must stop.
Alcohol
Heavy alcohol intake can impair male and female fertility. An occasional drink has not been shown to be detrimental, however once pregnancy is established, alcohol intake is absolutely contraindicated because of the effects it can have on the developing baby.
Caffeine Intake
Several studies have demonstrated that an increase in caffeine intake may decrease the chance of conceiving. We recommend limiting caffeine intake to 200 mg per day. One cup of coffee contains 100 mg caffeine.
The use of recreational drugs is contraindicated while attempting to conceive and during pregnancy.
Vitamin Supplementation
Several studies have indicated that folic acid supplementation can significantly reduce the occurrence of neural tube defects in infants. We encourage all women attempting to get pregnant to take at least 4 mg of folic acid daily. This is prescription strength and we will give it to you at your IVF consultation. We also recommend that you take an over-the-counter prenatal vitamin daily.
San Diego Fertility Center

Baby or children's aspirin (81mg) is also recommended every day. There has been a lot of research regarding the benefits of baby aspirin in increasing the circulation around the ovaries and the uterus, which could help stimulation and implantation. Baby aspirin may also help prevent the microscopic formation of blood clots that can increase one's chance of a miscarriage.
There is new evidence that excessive intake of vitamin A increases the chance of birth defects. Therefore, we recommend taking only one prenatal vitamin daily.
Routine Gynecologic Care
During your fertility treatment, it is important for you to continue routine follow-up with your gynecologist or primary care physician. This includes a yearly blood pressure check, physical examination, Pap smear, and baseline mammogram for women between the ages of 35-40.
Pre-Treatment Testing
All patients and their partners are required to complete a thorough infertility evaluation prior to beginning their IVF cycle. This will allow the practitioners to assess your overall health, and ensures that your fertility will not be impaired by an easily detected and remedied cause.
• Day 3 FSH (follicle stimulating hormone) and Estradiol level. This test must be done on
day 3 of your menstrual cycle and may give insight to egg (oocyte) quality prior to the egg retrieval.
• Hepatitis B (Surface Antigen) and Hepatitis C Antibody are blood born viral infections
that can pass through the placenta and is known to have long-term health consequences for both mother and child.
• HIV infection in either parent means there is a high probability of the virus passing
through the placenta to the child.
San Diego Fertility Center
• HTLV I & II (Human T-cell Lymphotropic Virus). This virus has been associated with
Leukemia and Myelopathy.
• Syphilis (RPR)
• DHEAS (Dehydroepiandrosterone sulfate). Elevated levels of this can interfere with
ovarian stimulation.
• Prolactin and TSH (Thyroid Stimulating Hormone). Abnormal values may interfere
with ovarian stimulation.
• Blood Type and RH Factor
• Cystic Fibrosis screening
• Genetic Counseling. The incidence of birth defects increases if you are over 35 years
old. A consultation can be arranged with a genetic counselor to discuss risk factors specific to you. If either partner has a family history of a genetically transmitted disease, you should also have this consultation.
Other Things to Consider
Doing things ahead of time will help to minimize your stress throughout your procedure cycle.
Make sure your insurance authorization is settled, and any financial concerns are finalized prior
to the IVF consult with the nurse practitioner.
Have all of your medications purchased prior to needing them. There's nothing worse than
having to scramble for medications at the last minute or on the weekend. Keep track of how
much medication you've used, how much you have left, and how much more you might need.
This can help alleviate any last minute problems.
Consider the amount of time needed for your monitoring appointments, and make arrangements
for your three days of bed rest (think of it as a vacation!). You may want to plan some
flexibility into your work schedule during the 5-6 days of monitoring appointments. Some of
you have physically demanding jobs that may require limitations. If a signed physician's excuse
would be helpful, we will be happy to provide one.
And last, but by no means least, consider taking advantage of the resources available for stress
reduction and communication enhancement offered by our office and the community.
Testing will include blood work for Hepatitis B and C, HIV, HTLV I & II, and RPR (Syphilis). This is in compliance with the California State Health and Safety Law, which mandates testing prior to using a man's sperm for insemination.
San Diego Fertility Center
Our embryologists will also perform a comprehensive semen assessment in order to determine the most appropriate manner for processing your sample on the day of egg aspiration. In men with significantly low sperm counts, motility, or morphology there is a possibility of carrying a genetic abnormality or mutation on the Y chromosome. This genetic mutation is the reason for the abnormal sperm count and may be passed on to male offspring.
MALE INFERTILITY
Male infertility factors contribute to approximately 50% of all infertility cases.
What Causes Male Infertility?
A man may be infertile because he produces too few sperm or no sperm at all. Reasons for a
low sperm count may include:
• Excessive use of alcohol, tobacco, or other illicit drugs
• Testicular exposure to overheating such as a prolonged high fever
• A genetic disorder such as Klinefelter's syndrome, cystic fibrosis, or a defective gene on the
• Infections of the genital organs such as the prostate or urethra, sexually transmitted diseases
that can cause sperm blockage, and severe mumps infection
• Hormone disorders of the pituitary gland, thyroid gland, or adrenal glands
• Exposure to toxins and chemicals in the environment may cause the body to release oxygen-
free radicals (oxidants) in the body which can damage sperm
• Exposure to radiation • Men who bicycle may develop scrotal abnormalities affecting sperm quality Abnormal sperm may occur when the sperm have a short lifespan or they are malformed, which prohibits them from swimming correctly. Abnormal sperm may be caused by the following: • Inflammation of the testicles
• Twisted or swollen veins in the scrotum (varicocele) • Abnormally developed testicles
• Genetic trait
• Exposure to toxins and chemicals • Increased testicular temperature Male infertility may also occur from physical or structural abnormalities such as: • Premature ejaculation
• Retrograde ejaculation (semen forced back into the bladder)
• Erectile dysfunctions • Any structural abnormalities that affect the testes, tubes, or other reproductive structures
San Diego Fertility Center
Other potential causes of male infertility include the following:
• Age:
The effect of aging is not clear, however there is some evidence of decreased sperm quality with advancing age, especially after age 70
• Autoantibodies (Antisperm antibodies):
Antibodies may cause sperm to stick together (agglutinate) and be unable to penetrate the egg
• Medications:
The effects of medications on sperm quality and count have not been extensively studied and many medicines are commonly prescribed without knowing whether they impair fertility. Known medications that may affect male fertility include: steroids, cimetidine (Tagamet), sulfasalazine (Azulfidine), metronidazole (Flagyl), salazopyrine, colchicine, methadone, methotrexate (Folex), phenytoin (Dilantin), corticosteroids, spironolactone (Aldactone), clonidine (Catapress), thioridazine (Mellaril), and calcium channel blockers (for high blood pressure)
• Medical Conditions:
Other medical conditions such as severe injury, major surgery, diabetes, HIV, thyroid disease, liver or kidney failure, heart attack, and chronic anemia may effect sperm quality
Male Infertility Potential Treatments
• Antibiotic treatment for infection or hormone treatment if a hormone imbalance is identified
• Avoiding radiation and environmental toxins, chemicals, pesticides, and lubricants • Avoiding excessive alcohol, smoking, and drug abuse
• Therapy to treat ejaculation problems
• Surgery to correct structural abnormalities • Antioxidant therapy to possibly improve sperm quality such as
• Vitamin C, Vitamin E, selenium and coenzyme Q10 supplementation. Vitamin C may also
help the body to absorb trace elements of zinc, cooper, magnesium, potassium, and calcium, which improve the vitality of sperm
• Dietary supplements such as Proxeed and Fertile One. These supplements are specially
formulated to enhance male fertility and may improve overall sperm quality
*Semen parameters can change from month to month and any impairments or improvements may take several months before becoming apparent due to the amount of time required for sperm development.
San Diego Fertility Center
STARTING YOUR IVF CYCLE
When all your testing is complete and you are ready to start your IVF cycle, please call
the office on Day 1 of your period to schedule an IVF consultation with one of our nurse practitioners
Please begin birth control pills on Day 4 of your cycle. There are two main reasons for
taking birth control pills prior to your IVF cycle. One, research indicates that taking birth
control pills prior to a stimulation cycle may help the ovaries respond to the stimulation
medication. Second, taking birth control pills allows flexibility in coordinating your cycle so
that procedures can be coordinated around your work schedule, planned trips, and when all the
necessary professionals are available. Please note that many patients experience "break
through bleeding" when taking birth control pills. This is normal. Please continue taking
the birth control pills daily regardless of the bleeding. Plan to be on birth control pills a
minimum of two weeks, and sometimes up to five weeks.
On the day of your IVF consultation, you will watch a 30-minute video of what the IVF
cycle entails. After the video, you will meet with one of our nurse practitioners to review your laboratory results, plan your calendar, review your protocol, give prescriptions and answer any questions or concerns you may have.
IN VITRO FERTILIZATION EXAMPLE CALENDAR
Please note: Each case is different, but we hope to will give you an idea about the timeline of
Start Birth Control Pills (BCPs) on day 4 of your menstrual cycle
The BCP allows flexibility in the start of your treatment cycle and prepares the ovaries for stimulation. Plan to be on the BCP for 2-5 weeks.
IVF Consultation appointment with one of the nurse practitioners
This appointment will review test results, give you prescriptions and coordinate IVF cycle. You must
be on BCP to be able to coordinate your dates.
San Diego Fertility Center
Month 3
Sunday Monday Tuesday
Wednesday
Thursday Friday Saturday
8 9 10 11 12 13 14
15 16 17 18 19 20 21
22 23 24 25 26 27 28
Progesterone Progesterone Progesterone
29 30 31 1 2 3 4
Progesterone Progesterone
Day 5 transfer) Day 5 transfer)
Key to Calendar
Blood and ultrasound = blood test for hormone levels and transvaginal ultrasound to measure follicle development in ovaries. Both are performed in our office.
BCP = Birth Control Pill. Remember that the actual length of time on BCP may vary from 2 – 5 weeks.
San Diego Fertility Center
Lupron = subcutaneous injection, taken once daily to prevent ovulation.
FSH/LH = subcutaneous injections given to stimulate the ovaries. Plan 8 - 12 days of FSH/LH injections.
HCG injection = injection that rapidly matures the eggs and prepares them for fertilization
Progesterone = intramuscular injection, helps prepare the uterine lining for embryo implantation.
The calendar shown above is an example of how the cycle stimulation may evolve. It is possible that the ovarian stimulation process is shorter or longer than that shown above. The example above shows 10 days of stimulation (FSH/LH shots). Patients typically are on 8 – 12 days of stimulation. A Day 3 or Day 5 (Blastocyst) transfer will be based on the number and quality of embryo development. A pregnancy test is performed 16 days after egg retrieval.
Antagon or Cetrotide are medications that keep you from spontaneously ovulating,
and may be substituted for Lupron. These subcutaneous injections would begin
midway through your FSH/LH injections. Your physician will determine which protocol
is best for you.
San Diego Fertility Center

San Diego Fertility Center
IVF Medications Prior to Egg Retrieval
Birth Control Pills
They help to calm ovaries and prevent cysts from forming prior to ovarian stimulation
Baby Aspirin
Taking baby aspirin increases circulation to the uterus and ovaries, prevents blood clots
Folic Acid
Folic Acid reduces the chance of birth defects
Doxycycline
Antibiotic for patient and partner to treat potential bacteria such as mycoplasma, uroplasma, and
Chlamydia which can be sexually transmitted.
Lupron, Antagon, or Cetrotide
Hormone used to prevent ovulation prior to your egg retrieval
Gonal-F, Follistim or Bravelle
Follicle stimulating hormone (FSH), works directly on the ovary to stimulate multiple follicles
(potential eggs)
Repronex or Pergonal
Human menopausal gonadotropin, they have a mix of FSH and LH hormones
Ovidrel, Pregnyl, Profasi, or Novarel (hCG)
Hormone used to mature the eggs, injected when the follicles are appropriate size
After Egg Retrieval
Progesterone
Hormone needed for luteal phase support of implantation and early pregnancy
Doxycycline
Second dose given just for the female partner to prevent a possible bacterial infection from
surgery and embryo transfer
Prednisone
This medication prevents the body from rejecting the embryos after the transfer
San Diego Fertility Center
Medications
Lupron
Lupron (leuprolide acetate) is a hormone used to improve follicular development and control
ovulation. Lupron is a daily, morning, subcutaneous injection given for approximately three
weeks until your follicles are mature and ready for the IVF procedure.
Once started, do NOT stop the Lupron until instructed. If ovulation were to occur
prematurely, the cycle would need to be cancelled.
Side Effects:
• Irritation at the injection site (itchy welt lasting only minutes)
(Most side effects will often resolve with the start of gonadotropins (FSH) injections)
Antagon or Cetrotide
Antagon (ganirelix acetate) or Cetrotide (cetroelix acetate) is a synthetic hormone that also
prevents ovulation. Antagon and Cetrotide work a little differently than Lupron by suppressing
luteinizing hormone (LH) more rapidly. Therefore, Antagon and Cetrotide subcutaneous
injections are given after the start of gonadotropin (FSH) stimulation as instructed by your
physician.
OVARIAN STIMULATION
Gonal-F, Follistim, and Bravelleare the brand names for a group of medications known
as gonadotropins or FSH (follicle stimulating hormone). Repronex and Pergonal are the
brand names for another group of medications known as human Menopausal Gonadotropins
(contain both FSH and LH or lutenizing hormone). Ovarian stimulation medications are
preparations of naturally occurring hormones, which are used to develop and mature multiple
follicles by directly stimulating the ovaries. They are very similar in their efficacy and often
used interchangeably.
What To Expect:
• Subcutaneous injection given for 8-12 days depending on how your body responds to the
• Give the injection approximately the same time daily in the evening between 6-10 PM
• The average number of eggs retrieved is between 8-15
San Diego Fertility Center
• A follicle (seen on ultrasound) is the fluid
surrounding a potential egg. Not every follicle will contain an egg and some are empty "cysts"
Ultrasound Monitoring
• Transvaginal ultrasound examination takes
between 5-20 minutes to perform and provides valuable feedback for monitoring follicular growth and determining when the follicles are mature and ready for retrieval.
Ultrasound picture of a stimulated ovary
Estradiol (E2) Blood Test
• The follicles in the ovary secrete estradiol and provide feedback on ovarian function.
An estradiol blood test is obtained frequently throughout the stimulation cycle to monitor the response of the ovaries to the gonadotropin medications.
Possible Reasons for Cycle Cancellation
• The follicles are not developing properly • An inadequate blood hormone level
• Excessive Estradiol level, indicating an increased risk for ovarian hyperstimulation
• Less than 5 maturing follicles seen on ultrasound
* If a cycle is cancelled, medication may be modified in subsequent cycles in an
attempt to improve your response.
Side Effects
Side effects of gonadotropins are generally minor but may include:
• Local discomfort at the injection site • Fatigue
Less common side effects may include:
• Multiple Births: Multiples may occur in up to 20-30 percent of pregnancies with
gonadotropin medications versus 1-2 % in the natural population. While most of the pregnancies are twins, some are composed of triplets or higher. High order multiple gestation pregnancies are associated with increased risk of pregnancy loss, premature delivery, infant abnormalities, handicaps due to the consequences of a very premature delivery, pregnancy induced hypertension, hemorrhage, and other significant maternal complications. Selective reduction is available to couples who conceive high order multiple gestations; although we do not directly perform the procedure.
• Ectopic Pregnancy (Tubal): This found at only a slightly increased rate, 1-3 % versus 1-
2 % in the general population. An ectopic pregnancy can be treated with medication or surgery. Combined tubal and intrauterine pregnancies occasionally occur with ovarian stimulation medications and need to be treated with surgery.
San Diego Fertility Center
• Adnexal Torsion (Ovarian Twisting): Torsion occurs when the stimulated ovary twists
on itself, cutting off its own blood supply. It is rare, occurring less than 1 percent of the time. Surgery will be required to untwist or remove the ovary. This is one of the reasons for activity restrictions after starting ovarian stimulation medications.
• Ovarian Cancer: Ovarian cancer seems, in part, related to the number of times a woman
ovulates. Infertility increases this risk; birth control pill use decreases it. Controversial data exists which associates ovarian stimulation medications (Gonal-F / Follistim / Repronex / Pergonal) to the risk of future ovarian cancer. While research is underway to help clarify this issue, the careful use of these medications is still reasonable, especially considering that pregnancy and breast-feeding reduce cancer risk.
• Ovarian Hyperstimulation Syndrome (OHSS): OHSS is uncommon, occurring in only
1-5 % of cycles and is more frequently seen in women who have the diagnosis of Polycystic Ovarian Syndrome (PCOS). It is characterized by rather sudden ovarian enlargement and abdominal fluid retention. If your monitoring indicates that you may develop hyperstimulation, we will bring this to your attention as soon as possible. Treatments most likely will consist of bed rest and careful monitoring of fluid levels. Hyperstimulation may be aggravated if pregnancy does occur. In such cases, we may either cancel the cycle or proceed with the egg retrieval but cryopreserve all embryos and transfer a month or two later.
In severe cases, OHSS can result in blood clots, kidney damage, ovarian twisting, and chest and abdominal fluid collections. During these times hospitalization may be required, usually for monitoring purposes, although a surgical procedure may be called for in some instances.
Symptoms occur after hCG administration or egg retrieval
• Excessive bloating
• Lower abdominal pain, some mild bloating and cramping is normal
• Nausea, vomiting, and/or diarrhea may accompany the abdominal pain • Sudden, rapid weight gain
• Urine output – noticeable increases or decreases in urination
• Shortness of breath
*Any symptoms please call our office
hCG (Human Chorionic Gonadotropin) or Ovidrel (Choriogonadotropin alfa)
Ovidrel, Profasi, Pregnyl, or Novarel are natural hormones that stimulate and induce
final maturation of the eggs, preparing them for fertilization. When your ultrasound monitoring
indicates that your body is ready for ovulation, we will call you with clear, exact instructions on
when to take your hCG injection.
It is crucial that hCG be taken at the time designated since your egg retrieval will be
scheduled exactly 36 hours later.
Side Effects:
• Rare, but may include bloating, breast tenderness, headache and fatigue • hCG is the same hormone your body releases when you are pregnant. You must be
careful not to take a pregnancy test too early, causing a false positive result.
San Diego Fertility Center
IVF PROCEDURE
IVF involves retrieving or aspirating the eggs from the ovary, fertilizing them in the
laboratory, and transferring the embryos back into the uterus a few days later. The egg retrieval is performed via vaginal ultrasound (similar to the ultrasound used for monitoring your follicles during your stimulation). Once each ovary is visualized by ultrasound, a thin needle is passed through the vaginal wall into the ovaries. Each follicle is drained, and collected into a test tube.
The embryologist examines the follicular fluid, identifies the egg, and then transfers
each egg to a special culture media. Sometimes there are ovarian cysts that contain no eggs but
appear identical to follicles that do contain eggs. Also, follicles of smaller size may not yield
eggs. The number of follicles seen with ultrasound, therefore, may not correspond to the number
of eggs retrieved.
Later, the sperm is prepared and placed with each egg. In some cases, the embryologist
will need to identify normal, motile sperm and inject it directly into each egg. This procedure is
called Intracytoplasmic Sperm Injection (ICSI). Once the eggs are inseminated or placed with
the sperm, they are placed into an incubator overnight.
PRE-OP INSTRUCTIONS:
1. Do not eat or drink anything for at least 8 hours prior to your scheduled procedure.
This includes skipping any oral medication you typically take in the morning.
2. Do not wear makeup, jewelry, or contact lenses on the day of your procedure.
3. A responsible adult must accompany you on the day of surgery and be able to drive you
home when you are discharged. It can be your partner, a friend or relative. If no adult is with you when you check in, your surgery may be delayed.
4. Wear comfortable clothes to put on after your procedure.
5. Arrive at the San Diego Fertility Center at your scheduled time.
EGG RETRIEVAL
You should arrive at the San Diego Fertility Center one hour prior to your scheduled
surgery time. About 45 minutes before your scheduled procedure, you will be escorted to the Surgery Center where you will change your clothes, have your vital signs taken, and sign consents. During this time the anesthesiologist will meet with you to review your medical history, complete a preoperative evaluation, and answer any questions.
Once the pre-op check-in is complete, you will be escorted to the operating room where
the anesthesiologist will start an IV to administer anesthesia throughout your procedure.
The lab team and an incubator are located at the foot of the operating table to assist with
San Diego Fertility Center
the collection of the eggs. If you have light sedation, you may be able to hear the embryologist and the doctor discussing the eggs as they are obtained.
When the procedure is completed, you will recover in the Post Anesthesia Care Unit.
Recovery generally takes 1 hour. The husband or partner may accompany the patient in the recovery area during this period. When you are fully awake and your vital signs are stable, you will be discharged to your car via wheelchair. An embryologist will inform you of the number of oocytes retrieved and answer any questions before you leave.
GIFT PROCEDURE
The GIFT procedure involves an egg retrieval via vaginal ultrasound, the same
procedure conducted in IVF. Once the eggs are retrieved, a laparoscopy is performed to return the eggs and sperm (gametes) into the fallopian tube(s) for natural fertilization.
The recovery period is a little longer (about 1 ½ to 2 hours) with GIFT because general
anesthesia is used to ensure the patient's comfort during the laparoscopy. When surgery is complete you will be taken to the recovery room. You can have medication for pain or nausea if needed. You will be given ice chips and then liquids to drink.
With your consent, any extra eggs not transferred during the GIFT procedure will be
taken to the lab for fertilization and freezing. The embryologist will call you daily to advise you
of the status of your eggs/embryos in the lab.
Risks:
Injuries during these procedures are extremely rare. Structures near the ovaries, such as the
bladder, bowel, or blood vessels could possibly be injured and require further surgery.
Limited bleeding from the ovary may occur, but the need for transfusion is extremely rare.
Infections following transvaginal egg retrieval are also possible but rare.
San Diego Fertility Center
SEMEN COLLECTION INSTRUCTIONS
DAY OF IVF PROCEDURE: Semen samples for use in IVF procedures may be produced
before or after the egg retrieval. Samples may be collected at home and brought to our office at
the same time as patient check-in. Samples should be produced within one hour of being
brought to SDFC. Semen samples for use in GIFT procedures need to be brought in or
produced at SDFC within two hours prior to the scheduled egg retrieval.
The specimen should be obtained by masturbation after 3-5 days of abstinence. More
than 5 days of abstinence is NOT recommended. It is important not to use any lotions or lubricants for sperm production as it may harm sperm motility.
DONOR SPERM: Please arrange to have your donor sperm samples delivered directly to the
San Diego Fertility Center IVF Laboratory. Samples should arrive at the Center by the time
FSH injections begin. Please contact our office with the date and approximate time of the
delivery.
POST EGG RETRIEVAL/GIFT INSTRUCTIONS
Following the procedure, the patient will recover in the Post Anesthesia Care Unit. It is
common for patients to experience mild vaginal bleeding and menstrual-like cramping after the
procedure. Medication can be administered during the recovery period to keep the patient
comfortable and may be taken orally at home for discomfort. Please inform our office or your
pharmacist if you are allergic to Codeine.
• You will need someone to drive you home.
• For about 24 hours after your procedure try to take it as easy as possible.
• You may take Vicodin or Extra Strength Tylenol as needed for pain. • You may return to work after 24 hours. When planning for your egg retrieval, you
may want to arrange to have 2 days off of work although you may return to work the day after your egg retrieval if you feel like it.
• You may shower, but no bathing.
• Have intercourse as desired.
• Begin intramuscular Progesterone injections as directed this evening, and continue
daily through pregnancy test. If your pregnancy test is positive, you will continue your Progesterone injections until notified to stop.
Should you experience any of the following symptoms when you leave the Del Mar
Surgery Center, please call the San Diego Fertility Center at 858-794-6363.
• Fever greater than 100 degrees.
• Increased abdominal swelling (some bloating is normal). • Intense or progressively worsening abdominal pain, unrelieved by pain medication.
• Heavy bleeding from the vagina or incisions.
• Nausea and vomiting. • Unable to urinate within 6 hours of your procedure, with increasing pain
San Diego Fertility Center
EMBRYOLOGY LAB UPDATES &
EMBRYO GRADING
You will receive a daily call from one of our embryologists to update you on the status
of your embryos beginning the day after your egg retrieval, and continuing to the day of your embryo transfer. The day after your egg retrieval (Day 1), the embryologist will give you information about the number of eggs that were mature, and of those, how many fertilized. Each day following, you will be updated with how your embryos are progressing. These calls usually occur in the afternoon, around 2 – 3 p.m. after discussing your progress with your doctor. Attending the "Mystery behind the Microscope" talk will greatly help you understand the information you will be given. We strongly encourage you to attend one of these talks prior to your IVF cycle.
Embryos are typically transferred on Day 3 or Day 5. The day of the egg retrieval is
considered Day 0. The number and quality of the embryos determine which day will be most beneficial to you. The embryologist will discuss your progress with your physician, and will help you determine which day the embryo transfer will occur. The embryologist will also inform you of your embryo transfer date and time.
OUR GUIDE TO EMBRYO GRADING
Day Zero
On the day of your retrieval an embryologist will speak with you about the number of
eggs retrieved and verify the laboratory treatment plan. On average, only about 80% of follicles yield eggs. Smaller follicles may yield immature eggs or no egg at all. Maturity does not imply age or timing, but refers to the completion of meiosis, the process where the egg chromosomally divides. The egg divides from 46XX, a normal female, to 23X, an egg that is ready to be fertilized. Only mature eggs, those that have released one polar body containing half of the chromosomes, can be inseminated. Insemination, whether it is natural (placing the sperm with the eggs) or Intra Cytoplasmic Sperm Injection (ICSI), (placing one sperm in each egg or
San Diego Fertility Center
oocyte) occurs on the afternoon of Day 0. Average fertilization rates are 60% of the eggs inseminated, regardless of the method of insemination.
If ICSI is performed, each oocyte is cleaned from the surrounding corona and cumulus
cells and will be graded at this time on a simple Good/Fair/Poor scale. If natural insemination is performed, the corona and cumulus cells remain attached to the eggs and no oocyte grading is performed.
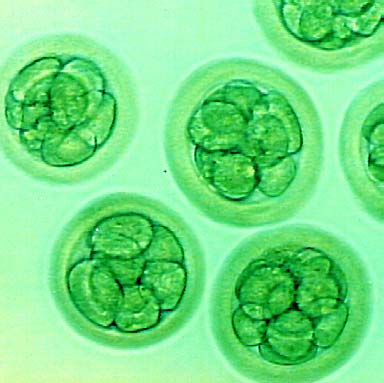
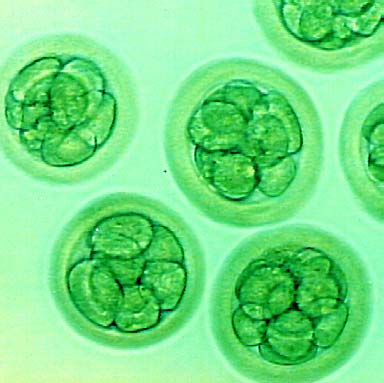
The next day, Day 1, is when fertilization check
occurs. We check fertilization 16- 22 hours after insemination and want to see two polar bodies and two pronuclei.
One pronuclei contains the genetic material from the
sperm and one contains the genetic material from the egg. If there is zero, one or three pronuclei, the fertilization process has not proceeded properly and we do not continue to culture these eggs. On Day 1 the egg has not divided yet and no additional grading is performed at this time.
Normal fertilized eggs on day 1
Day 2 is the first day of embryo cell division. About 98% of fertilized eggs will divide.
The embryo should divide every 12-24 hours after fertilization and should have between 2 – 4 cells at this time. When embryos are checked, three pieces of information are ascertained:
• The cells in each embryo are counted to see if the embryo has an appropriate number of
cells for the day in question. For Day Two this range should be 2, 3, or 4 cells. Remember, the embryos are checked for only a moment and often an odd number of cells are observed. This is not indicative of a problem with the embryo.
• We take a close look at the symmetry of the cells. Cell
symmetry is graded as very even (Good Quality), slightly uneven (Fair quality), or very uneven (Poor Quality). Most embryos are in the fair range and most people have a range of quality. This is normal. Keep in mind that each embryo is genetically unique and the benefit of IVF is to identify and transfer the best embryos back into the uterus.
• We look at fragmentation level. Sometimes, instead of
a cell dividing into two perfectly even new cells, small fragments of cytoplasm escape. Cytoplasm is the substance contained within cells. These small fragments do not contain any genetic material, unlike
Embryos without fragments on
the cells in the embryo.
San Diego Fertility Center
A fragmentation level of 0 to < 10% is preferred. If fragmentation reaches between 10
and 30 %, the embryo is not the first choice for transfer or cryopreservation and will probably continue to be observed in culture. Fragmentation of greater than 35% may indicate an embryo that is dying and the cells are breaking down. These embryos would be the last choice for transfer and will not be considered for cryopreservation. Scale for fragmentation:
A = No Fragments B = < 10% fragments C = 10 – 35% fragments D = > 35% fragments
Therefore, each embryo receives an overall grade composed of three figures. A perfectly
even four cell embryo with no fragmentation would be a 4GA, and an uneven eight cell with 20% fragments would be an 8FC.
Day Three
On Day 3 we expect 4 to 8 cells in each embryo and
grade on the same scale as Day 2.
If the best embryos are evident on Day 3, the transfer
will probably occur that day. Many patients have their transfer on Day 3 and on average, three embryos are placed into the uterus. Further, patients have a higher probability of a transfer this day if they have less than 8 embryos. It is important to note that the statistics from our lab show no difference in the pregnancy rate for a day 3 or day 5 transfer.
If there are good to fair quality embryos still in culture
Embryo with 8 cells on day 3
after the transfer, the embryologist will discuss the possibility of a freeze. We do not want to freeze any embryos that do not look strong enough to survive the freeze and thaw. If there are embryos that are slowly developing, we can continue to culture them and see if the blastocyst stage is reached. If good or fair blastocysts are formed we may be able to freeze at that time.
On Day 4 we look for the separate cells to start
compressing together and become connected. This process is
called compaction. When they are completely compacted, a
tight ball is formed and no individual cells are evident, the
embryo is called a morula.
Day Five
On Day 5, ideally, the morula will pull in fluid and
begin to expand out like a bubble. Once a fluid filled cavity is established the embryo is called a blastocyst. A blastocyst has
8 Cell embryo and morula on day 4
three parts: an inner cell mass that is destined to become fetal
San Diego Fertility Center
tissue, the flattened outer cells called trophectoderm, which become the fetal part of the placenta, and the fluid filled cavity, called the blastocoel cavity. We will give a grade of good, fair or poor for the size and organization of the inner cell mass and the organization of the trophectoderm. In addition we will note the stage of expansion: early, expanding, fully expanded, and hatching blastocysts.
Only 30 to 40 % of the embryos in the best cycles
become a blastocyst. For this reason, a patient should have at
least 7 or 8 embryos to consider a Day 5 transfer. Day 5
transfers are generally performed for donor recipients and
patients with a high risk of a multiple pregnancy.
At the embryo transfer we will review the stages and
Early blastocyst on day 5
quality of all the embryos and discuss the possibility of cryopreservation. In order to be frozen at this stage, embryos must be good to fair quality blastocysts. If there are morula or compacting embryos that are candidates for freezing, we will observe them in culture for another day to see if a blastocyst forms and discuss a freeze at that time. This information is intended as a guide to help you understand what is happening with your embryos. Here at SDFC, communicating with you and making sure you understand your situation is a high priority. The process of embryo grading is complex and can be confusing. Don't be afraid to
ask questions. We are here for you!
Expanded blastocyst on day 5/6
San Diego Fertility Center
EMBRYO TRANSFER
The Embryo Transfer (ET) takes approximately 10-15 minutes, and is very similar to the
uterine measurement taken at your baseline appointment. You will not need anesthesia on this day, so there is no need to abstain from eating or drinking before your ET. Please do not apply perfume, or scented lotions on the day of your embryo transfer. An embryologist will meet with you to discuss your embryos and the number of embryos planned for your transfer.
Once you, the embryologist and physician have confirmed the plan for the embryo
transfer, the physician will insert a speculum. A vaginal ultrasound will be used to visualize the uterine cavity. The embryologist will obtain the embryos and load them into the catheter. A small catheter is gently passed to the top of the uterus, through the cervical opening, and the embryos are placed. The catheter is then carefully removed.
Following the Embryo Transfer you will remain laying for 30 minutes, then discharged
to your car via wheelchair. You must have someone accompany you and drive you home.
GUIDELINES AFTER EMBRYO TRANSFER
• For 72 hours following your Embryo Transfer you will be on bed rest. You may get up to
go to the bathroom, shower, and eat. You may also use stairs. Do not bathe.
• For two weeks following your Embryo Transfer, avoid strenuous physical activity or heavy
lifting. You may return to work 72 hours after the procedure.
• You may have intercourse as desired. • You may experience spotting and cramping after your Embryo Transfer. This is normal,
caused by the instrumentation used during your procedure.
• There may be fluid leakage from your vagina after the Embryo Transfer. You may wear a
minipad, but do not use tampons.
• Continue taking the Doxycycline as directed.
• Start Prednisone daily for 3 days. This may be started at any time of the day of embryo
• Progesterone supplementation will be continued for two weeks following the Embryo
Transfer, and continue thereafter if your serum pregnancy test is positive.
San Diego Fertility Center
Progesterone is a hormone produced by the ovarian corpus luteum during the last two
weeks of the menstrual cycle and during early pregnancy. After the seventh or eighth week of
pregnancy the placenta takes over progesterone production. Natural progesterone is prescribed
in many fertility treatments for luteal phase support of implantation and early pregnancy.
Natural progesterone is also prescribed to support the luteal phase for patients in virtually every
IVF/GIFT program today. The progesterone prescribed is derived from natural sources and
is identical to that produced in the body.
Synthetic forms of progesterone (progestins) are manufactured into medications like oral
contraceptives and Provera, and are NOT used to support the luteal phase in IVF/GIFT cycles.
Synthetic progestins have been associated with a slight increase in birth defects if taken
during early pregnancy. Unfortunately, both natural and synthetic forms of progesterone are
grouped together by the FDA. As a result, the natural progesterone medication that you receive
may contain a package insert advising against its use during pregnancy. At present, there is no
known risk of birth defects associated with natural progesterone, and the benefits of this
medication are thought to outweigh any potential risk.
You will begin taking progesterone the evening of your egg retrieval and will continue
taking it daily until your serum pregnancy test. If your pregnancy test is positive, the medication will continue until you taper off of it around the ninth week of your pregnancy.
SIDE EFFECTS:
• Vaginal spotting or irritation
• Uterine cramping • Breast fullness or tenderness
• Lightheadedness
Do NOT discontinue your Progesterone until directed by our office.
San Diego Fertility Center
PREGNANCY TEST
Bleeding or spotting can occur in a normal pregnancy. This does not mean that
you are not pregnant! Do not discontinue any medication until after your pregnancy test
and you have spoken with someone at our office.
Blood will be drawn for a serum pregnancy test approximately 16 days after your egg
aspiration. A blood pregnancy test is extremely important because it is more accurate than a urine pregnancy test, and it is critical for detecting situations such as an ectopic pregnancy. Therefore, even if you feel that you are not pregnant, a blood test must be run for thoroughness.
Your pregnancy test will be performed at The San Diego Fertility Center. We can give
you accurate results, within the same day.
If your pregnancy test is positive, it will be repeated in 48 hours, and possibly repeated a
third time in another 48 hours. This is to help assess the quality of the pregnancy. Your medications will continue, so check your supply and have us renew your prescription if necessary.
If your pregnancy test is negative, you will discontinue all medications. Your menstrual
cycle may take several days to 1-2 weeks to start and may be slightly heavier than normal. Progesterone may delay your period, even if you are not pregnant.
POST IVF APPOINTMENT
You will be advised during your IVF cycle to schedule a follow-up appointment with
your physician. If you have had your pregnancy test and still don't have this appointment scheduled, please schedule it for roughly two weeks after your pregnancy test. If you are pregnant, we will perform your first OB ultrasound at your Post IVF Appointment. If your pregnancy test is negative, your physician will discuss what new information was learned during your cycle, how this information impacts your chance of success, and what is recommended for future cycles. Since the physician will not have all your cycle information until this appointment, we recommend saving your questions for this appointment.
One month of no medication (including birth control pills) is needed before proceeding
with a frozen embryo transfer or another IVF or GIFT cycle.
San Diego Fertility Center
FROZEN EMBRYO TRANSFER (FET) CYCLE
Generally speaking, success rates with a frozen embryo transfer are slightly lower than
IVF. The reason for this is that the best embryos are usually transferred during the IVF cycle. If the remaining frozen embryos are of the same quality as those transferred, then success rates are likely to be the same. To get started with your frozen embryo transfer cycle:
• Call the office on Day 1 of your period to schedule an FET consult with one of the nurse
• Start birth control pills (BCP) on Day 4 of your cycle. Continue taking active birth
control pills until your consult. Plan to be on BCPs 2 – 5 weeks.
• During the consult, we will review your protocol, plan your calendar, give prescriptions
and answer any questions you have.
There are a few protocols for frozen embryo transfer cycles. Since we have already
obtained your embryos, the focus of the FET cycle is building an optimal uterine lining. Typically, you will start a medication to keep your ovaries from ovulating during your cycle. Ovulation causes the uterine environment to change, preventing accurate synchronizing of your uterus with your embryos. While this rarely occurs if you've taken the medication correctly, we may need to cancel this cycle if you do ovulate in order to optimize your chance of success.
You will come in for a baseline ultrasound and blood tests to confirm that your ovaries
are quiet, and hormone levels are low. Once this has been determined, you will start taking estrogen pills to build your uterine lining. You will need monitoring visits once a week for two weeks to confirm that your uterine lining is developing as planned.
Once the uterus and hormone levels are optimal,
you will be advised when to begin Progesterone injections. Beginning Progesterone injections synchronizes the uterus with the embryos, so that we are putting Day 3 embryos in a "Day 3" uterus. Because the ovaries aren't producing Progesterone, as they were in the IVF cycle, more Progesterone may be required during the FET cycle. Progesterone injections are given twice a day, 12 hours apart.
Approximately 80% of the frozen embryos will
survive the thaw process. Usually, the higher the embryo
quality when it is frozen, the higher the likelihood that it
Normal uterine lining
will survive the thaw process. Because not all embryos will survive the thaw process, it may be necessary to thaw more embryos to achieve the desired number of embryos to transfer. The consent to thaw embryos must be signed by both partners, and received in the embryology lab prior to thawing your embryos. Embryos are thawed roughly an hour prior to your embryo transfer procedure.
The embryo transfer procedure is the same as your IVF procedure, followed by 72 hours
San Diego Fertility Center
of bed rest. The same guidelines apply (see Embryo Transfer section). You will continue on your Progesterone injections and Estrogen pills at least through your pregnancy test. If you have a positive pregnancy test, these medications will continue throughout most of your first trimester.
ESTROGEN
Estrogen is a hormone produced by the ovary that builds the uterine lining in the first
two weeks of the menstrual cycle, and continues throughout the pregnancy. Estrogen
medication can be given in pill, patch, and injection form. Your physician will determine which
Estrogen medication is best for you.
Side Effects:
• Breast tenderness
• Increased vaginal
San Diego Fertility Center
A POSITIVE PREGNANCY TEST!
• CONGRATULATIONS! But be cautiously optimistic because this positive test is just
the first milestone in a long process.
• Repeat your quantitative beta-HCG blood test in 48 hours (2 days).
• Continue taking your Progesterone as directed. You will stay on this medication until
approximately your 9th week of pregnancy. We will notify you when you can stop the hormonal supplementation.
• Continue taking prenatal vitamins, Folic Acid (4mg), and one baby aspirin (81mg) daily.
• Eliminate caffeine, alcohol, smoking, and all drugs (including any over-the-counter
medications). Consult with your physician regarding any prescription medications.
• Tylenol may be taken in the event of minor discomforts and should be taken if you have
an elevated temperature over 100 degrees.
• Have intercourse as desired.
• Limit activity to a sedentary level. No exercise.
• Avoid any increase in body temperature (hot tubs, saunas, etc.) as it is suspected that this
may cause neural tube defects. Avoid situations in which you may increase your exposure to colds, flu.
• It is advised that pregnant women be cautious to avoid contacting toxoplasmosis (an
organism found in cats that can cause severe injury to a developing fetus). The toxoplasmosis eggs are carried in cat feces. You should remember to wear gloves when gardening, wash your hands and vegetables well, and have your partner change the litter box.
• An ultrasound can be performed approximately 2 weeks after a positive pregnancy test.
We would like to perform the ultrasound at the San Diego Fertility Center in order to provide reassurance on the quality of the pregnancy and to confirm the number of gestations. If your insurance permits, we would be privileged to perform ultrasound monitoring up through 8-9 weeks of pregnancy or until the transition to your OB physician.
San Diego Fertility Center
ASSISTED REPRODUCTIVE TECHNOLOGY
Questions and Answers
Q. Why is the success rate with ART so low?
A. Studies of human reproduction indicate that, for a couple with proven fertility, the likelihood
of conception is only 20% per month. ART affords couples with infertility problems excellent
chances for conception; often much higher than natural rates.
Q. Is there a possibility of multiple births from ART?
A. Yes, any time more than one embryo is transferred, there is a chance for multiple
pregnancies. It appears that the rate of twin births is greater than in the normal population (1 in
80). Triplets and quadruplets have also been conceived through ART procedures. Although we
do not directly offer it, selective reduction is available to couples who conceive multiple
gestations.
Q. Is there an increased chance of birth defects if I become pregnant through ART?
A. No. Numerous studies have reported no increased risk of birth defects in children conceived
through ART compared to those conceived in the general population.
Q. Can we have intercourse while taking the hormone medications?
A. Yes. However, it is recommended that the male abstain from ejaculating for 3 -5 days
preceding the egg retrieval. This precaution assures that the semen sample on the day of egg
retrieval contains the maximum number of motile sperm. You may find that near the time of
egg retrieval your ovaries will be markedly enlarged and tender, possibly making intercourse
very uncomfortable.
Q. What activity restrictions are recommended during my stimulation?
A. As your ovaries begin to stimulate, they will become enlarged and tender. Limited activity
reduces the risk of ovarian torsion and/or rupturing the follicles on the ovaries. As a general
rule, it is advised that you stop any activity that involves bouncing, or jarring the pelvis by the
time you are returning for your first ultrasound to monitor your stimulation.
Q. What if I ovulate before the retrieval?
A. On the day of the egg retrieval, a vaginal ultrasound will confirm that the follicles are still
intact. If they are, it can be assumed that ovulation has not occurred and oocyte retrieval will be
attempted. The medications Lupron, Antagon, or Cetrotide also help to assure that ovulation
does not occur before egg retrieval has been performed.
Q. How much activity is recommended after Embryo Transfer (ET)?
A. Most doctors recommend a fairly sedentary, quiet 3 days after embryo transfer or GIFT.
Thereafter, most patients resume their normal routines. Strenuous exercises, like running or
heavy lifting, etc. should be avoided until a pregnancy test has been performed.
San Diego Fertility Center
Q. If an embryo transfer takes place, how long must we wait until we have intercourse
without risk to the embryo?
A. Nobody really knows for sure if intercourse aids or impedes implantation. Theoretically,
uterine contractions result from intercourse. We recommend that you have intercourse as
desired without fear of jeopardizing your cycle outcome.
Q. Can I swim after my transfer?
A. Yes, after 72 hours.
Q. Can I have a glass of wine or alcohol during the cycle up until the pregnancy test?
A. No alcohol after the procedure
Q. Can I travel more than 4 – 6 hours in a car after my transfer or fly in an airplane?
A. Yes
Q. Can I get my hair colored or permed?
A. Not recommended after the transfer
Q. Can I use Monistat for a yeast infection?
A. Yes
The following list of immunizations or injections are OK during a cycle:
• Tetanus shot
• Hepatitis Vaccine
• Allergy shots
• Chicken pox immunoglobulin
• Novocaine (dental procedures)
The following is a list of medications that are OK to take before or after embryo transfer:
• Tylenol Cold or PM
• Cold medications (Sudafed,
• Valium, Prozac, Zanax, Ativan
• Amoxicillin, Ampicillin, Erythromycin
• Bactrim – OK before pregnancy test
• MOM, Colace, Senekot, Immodium,
• Flagyl – OK before pregnancy test
• Doxycycline, Tetracycline (OK before
• Headache meds: Fiuricet, Fiorinal
• Nasal spray decongestants
Do NOT take the following medications:
• Echinacea, St. John's Wort, Gingko Biloba
San Diego Fertility Center
IMPORTANT REMINDERS DURING YOUR CYCLE
Calling to start your cycle When your period starts, please call the office during business hours. If your period starts after business hours, please leave a message on the machine. You will be contacted the next day to schedule any necessary appointments. Please do not page the provider on call to notify them of your menses onset. Medication supplies Once you receive all your medication, please review it all to make sure you have all your medication and supplies. Many pharmacies do not stock these medications, and there is nothing more stressful than trying to hunt down medication on the day you are supposed to take it. In addition, make sure you have enough medication to get you through a weekend. The pharmacies that do stock these medications are typically not open on the weekends. hCG Injection (Pregnyl, Novarel, Profasi) This is an intramuscular injection. There are two vials in this box: one vial of water and one vial of powder. Please draw up only 1 cc (or 1 mL) of water and discard the remaining 9 cc of water. Inject the 1 cc of water into the vial of powder. Draw up the mixed solution, switch back to the 1 ½ in. needle and inject it at the specified time, in the same place you will do your Progesterone injections. hCG Injection (Ovidrel) Ovidrel comes in two forms: one is premixed and comes in a loaded syringe with needle, the other needs to be mixed. If you are mixing Ovidrel, use ALL the water and inject it into the vial of powder. Draw up the solution using the same needles and syringes you used for your stimulation medications (Gonal F, Follistim, Bravelle). Inject this medication into your abdomen or upper, outer thigh (the same place you injected your stimulation medications). Injection Instructions Please make sure you receive your injection instructions prior to starting your injections. We may not have staff available to give you instructions on the day you need to begin. Sperm Collection for IVF The stress of being asked to produce a specimen at a specific time causes some men to be unable to produce. If there is any chance that specimen production will be difficult, please talk to your physician or embryologist prior to the day of the egg retrieval. There are solutions to this situation, but we need to know prior to the day of the procedure. Doctor on Call We want you to feel as comfortable throughout your cycle as possible. For some patients, coordinating the cycle around your schedule is more important than scheduling with a certain physician. If you would like a certain week, it is possible to have the physician on call perform your procedure. Because we have a team approach, the physician on call is aware of your particular situation.
San Diego Fertility Center
THE EMOTIONAL ASPECTS OF INFERTILITY
When a couple deals with problems of infertility, attention is focused on the physical
aspects of the problem. The goal of "getting pregnant" becomes a journey through medical procedures. The emotional aspects of infertility are often neglected, although how one feels during this journey is equally important.
The first time a couple is confronted with the possibility of not conceiving they feel
shocked. Most people assume that when they choose to have a child, they will. Suddenly, self-image issues arise that can be devastating. Men often feel a tremendous sense of failure, a basic loss of masculinity in their inability to father a child. Women speak of feeling as if their bodies are "broken". They worry that they are not completely female if they cannot become pregnant and give birth to a child.
Anger and disappointment are feelings that alternate with guilt. The couple feels
cheated. Everywhere they look, women are pregnant and parents are pushing a baby stroller. They ask, "why us". The infertile partner, if pinpointed, feels tremendous guilt, fearing he/she is depriving the partner of his/her chance to be a parent.
Frustration and shame will cause couples to isolate themselves from friends and family.
They do not want to hear those often repeated and untrue myths such as "just relax, have a glass of wine, and let nature take care of itself". Becoming pregnant becomes the focus of one's life, and permeates everything.
Infertility causes stress in the best of marriages. Scheduled sex seems impersonal and
ritualized. Spontaneity is missing and resentment can build as each partner feels pressure to perform according to a calendar. If medical procedures are involved, one partner is sometimes briefly incapacitated. Medical costs lead to economic pressures. Communication breaks down and the partners feel isolated, just when they need each other the most.
The most painful feeling of absolute infertility is grief, which precedes a resolution. The
couple faces a true sense of loss, which due to the vagueness of infertility, never is exactly clear. The time at which this happens can vary between partners, but the grief in losing the opportunity ever to have a child is devastating, a time of pain. And yet, if the grief is worked through, there is resolution. The couple again finds a sense of moving on in life.
Infertility is complicated both physically and emotionally. With support and awareness,
the myriad feelings surrounding these issues can be managed successfully. Please let us know if you desire any additional support.
San Diego Fertility Center
ASPIRATION
The application of light suction to the ovarian follicle to remove the eggs.
ASSISTED HATCHING IN IVF
Assisted hatching is an IVF technique in which the zona is broached prior to embryo transfer
thus improving the likelihood of successful hatching and embryo implantation. Recommended
for all women over 40 years of age and any patient with thick or dark zona pellucida.
CORPUS LUTEUM
A special gland that forms on the surface of the ovary at the site of ovulation and produces
progesterone during the second half of the menstrual cycle. It is necessary to prepare the uterine
lining for implantation by the fertilized egg.
CRYOPRESERVATION
A procedure used to preserve and store embryos by freezing, which will allow them to be
utilized at a later date.
EMBRYO TRANSFER
Procedure to place the "embryos" (fertilization and cleavage of eggs has occurred) back into the
woman's uterus. Embryo transfer takes place on day 3 or day 5 (counting retrieval as day 0).
ENDOMETRIUM
The mucus membrane lining the uterus where the embryo implants.
ESTRADIOL
The naturally occurring estrogen produced by the follicles in the ovary.
San Diego Fertility Center
ESTROGEN
The primary female hormone produced mainly by the ovaries from puberty to menopause.
FALLOPIAN TUBE
Either of a pair of tubes that conduct the egg from the ovary to the uterus. Normal fertilization
tales place within this structure.
FERTILIZATION
A spermatozoa has penetrated the egg and two pronuclei are present within each egg. The
pronuclei contain the DNA or chromosomes, one set from the male spermatozoa and the other
from the female egg. The fertilized egg is now called an early embryo or zygote.
FOLLICLE
The fluid filled sac in the ovary that has nurtured the ripening egg and from which the egg is
released during ovulation.
FOLLICLE STIMULATING HORMONE (FSH)
A hormone produced and released from the pituitary gland in the brain that stimulates the ovary
to ripen a follicle for ovulation.
HYPERSTIMULATION SYNDROME
A syndrome which may include enlargement, gastrointestinal symptoms, abdominal distention,
pelvic pain, and weight gain.
IMPLANTATION
The embedding of the embryo in the lining of the uterus.
INSEMINATION
The placement of sperm into a woman's vagina/cervix for the purpose of conception.
San Diego Fertility Center
INTRACYTOPLASMIC SPERM INJECTION (ICSI)
Laboratory procedure developed to help infertile couples undergoing in vitro fertilization (IVF)
due to severe male factor infertility. ICSI involves the insertion of a single sperm directly into
the cytoplasm of a mature egg (oocyte) using a microinjection pipette (glass needle).
LAPAROSCOPY
Abdominal surgery using laparoscope (fiberoptic system) to view the uterus, fallopian tubes,
and ovaries.
LH SURGE
Luteinizing Hormone (LH) has been released by the pituitary gland, which will trigger the
release of mature eggs from the follicles (ovulation is occurring).
LUTEAL PHASE
The last fourteen days of the menstrual cycle after ovulation has occurred. It is associated with
progesterone production.
POLYSPERMIA
The egg has been fertilized by more than one sperm and therefore cannot be used for Embryo
Transfer during an IVF procedure.
PROGESTERONE
A hormone produced and released by the corpus luteum of the ovary during the second half of
an ovulatory cycle. It is necessary for the preparation of the lining of the uterus for the
implantation of the fertilized egg. It is also produced by the placenta during pregnancy.
ULTRASOUND
A technique for visualizing the follicles in the ovaries, the uterine lining, and the fetus in the
uterus allowing for an estimation of size. Also known as a Sonogram.
UTERINE SOUND
The placement of a small sterile catheter through the cervix to measure the length of the
intrauterine cavity for the purpose of the future embryo transfer.
San Diego Fertility Center
Source: https://www.sdfertility.com/content/2-fertility-treatments/3-ivf-procedure/ivf-manual.pdf
Contents Definition, epidemiology, burden and etiology of osteoporosis………………………. 1 I-1 Definition and concept . 1 I-2 Epidemiology of osteoporosis and osteoporotic fractures…………………………… 1 2.1 Worldwide epidemiology . 1 2.2 Epidemiology in Asia and Thailand. 2 I-3 Burden and impact of osteoporosis and osteoporotic fractures . 2 3.1 3 Osteoporosis related mortality and morbidity). 3 3.2 Health economic aspect of osteoporotic fractures)………………………………. 3 I-4 Pathogenesis and etiology . 4 4.1 Pathogenesis . … 4 References . 5
Joint Action for ResultsUNAIDS Outcome Framework2009–2011 UNAIDS/09.13E – JC1713E (English original, May 2009) Updated version March 2010 © Joint United Nations Programme on HIV/AIDS (UNAIDS) 2010. All rights reserved. Publications produced by UNAIDS can be obtained from the UNAIDS Content Management Team. Requests for permission to reproduce or translate UNAIDS publications—whether for sale or for noncommercial distribution—should also be addressed to the Content Management Team at the address below, or by fax, at +41 22 791 4835, or e-mail: [email protected].