Sydneyfibroidclinic.com.au


Adenomyosis: A potentially missed, neglected and inappropriately managed condition
By Dr Eisen Liang (Interventional Radiologist) www.sydneyfibroidclinic.com.au
Adenomyosis is a benign disease of the uterus due to the presence of ectopic endometrial glands and stroma, deep within the myometrium with adjacent reactive myometrial hyperplasia. The disease can be diffuse or focal (adenomyoma).
The clinical findings are non-specific and therefore diagnosis is not easy to establish. Adenomysis can cause severe menorrhagia and dysmenorrhoea. The patients are usually multiparous in their 40s, but can be younger, nulliparous, presenting with infertility. The uterus maybe enlarged and tender. In research setting and practices with special interest in adenomyosis, transvaginal sonography (TVS) can achieve high accuracy. In real-world practice, many adenomyoses were missed or mistaken as uterine fibroids. Fibroids are present in 40% of women. Adenomyosis is also a very common finding on hysterectomy specimen. The presence of fibroids can mask the presence of adenomyosis on TVS. MRI is more accurate in detecting subtle diffuse adenomyosis and in differentiating fibroids from adenomyomas.
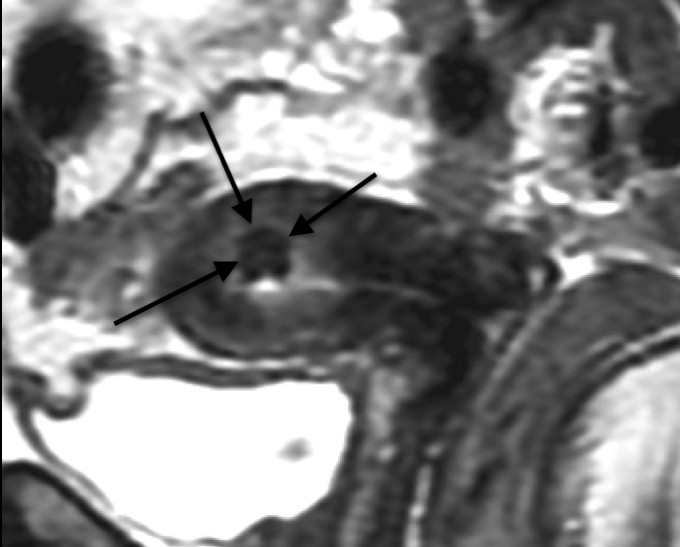
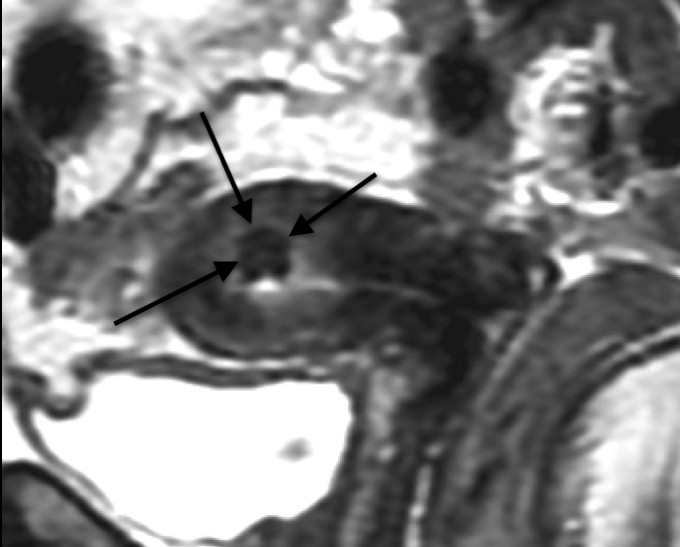
MRI showing adenomyoma before UAE and shrunken "scarred" adenomyoma post UAE.
Focal adenomyosis or adenomyoma can simulate fibroid on TVS. Open, laparoscopic or hysteroscopic resections may have been attempted with the wrong pre-operative diagnosis. Unlike fibroid, the boundary with the adjacent myometrium is indistinct and therefore adenomyoma cannot be enucleated. The resection is often abandoned. Excision of a large part of the myometrium, as may be needed to remove all affected areas, may lead to difficulty in wound apposition, decreased expansive capacity of the uterus, weakness and ultimately uterine rupture during pregnancy.
Endometrial ablation heats only a depth of few millimeters of tissue and is not useful except for the very superficial type of adenomyosis. It can seal off endometrial sinuses and potentially making dysmenorhea worse. In the setting of painful menorrhagia and an apparently normal TVS, it is prudent to exclude adenomyosis by MRI before recommending endometrial ablation.
Laparoscopy is performed when endometriosis is suspected on clinical and sonography findings (such as presence of chocolate cysts). Hysteroscopy is indicated for suspicion of endometrial pathology and polyps on TVS. These invasive procedures however are not indicated primarily for the diagnosis of adenomyosis. There is no specific blood test for adenomyosis. CA 125 may be raised but this is neither sensitive nor specific.
Adenomyosis is often neglected due to the lack of specific treatments. Clinicians have been focusing on symptomatic relief of menorrhagia and dysmenorrhoea. NSAID and tranexamic acid are used to treat menorrhagia. Oral progestrogen might have been tried but may not be tolerated due to side effects such as headache, nausea, bloating sensation and mood changes. Low-dose, continuous combined oral contraceptives with withdrawal bleeds every 4–6 months maybe used for symptom control. Progestrogen-releasing IUD (Mirena) has patient satisfaction rate of 56% at 1 year, 66% at 2 year and 73% at 3 year. It may not be immediately effective. The side effects are irregular spotting or continuous bleeding in the first few months, acne, weight gain, bloating sensation and mood changes. Gonadotropin-releasing hormone (GnRH) agonist can be used only in the short term, due to its side effects of hypoestrogen state such as hot flushes, mood changes and osteoporosis.
In the past, hysterectomy is the only definitive treatment for adenomyosis. Since 1995 uterine artery embolisation (UAE) has been used to treat symptomatic fibroids. Its safety and effectiveness have been well established, including 6 randomised control trials, demonstrating no difference in quality of life outcome compare with hysterectomy. The same procedure has been found useful in treating patient with adenomyosis. In our own UAE series, 29% of our patients have adenomyosis. Despite this, we have 96% success rate in controlling menorrhagia and 93% overall patient satisfaction rate. Currently we are reviewing our series of over 100 adenomyosis patients treated with UAE and our patient satisfaction rate is around 90%.
UAE data on adenomyosis is also available from 511 women from 15 studies (1999 – 2010). For pure adenomyosis, relief was achieved in 83% short-term and 65% long term. For combined adenomyosis and fibroids, relief was achieved in 93% short-term and 82% long term. The hysterectomy rate is around 13%, suggesting that 87% of women can potentially be spared of hysterectomy.
There were no deaths or serious adverse events reported. Minimal side effects, cost-effectiveness benefits, and retention of fertility render UAE an attractive treatment option.
Conclusions: Adenomyosis can be a debilitating condition significantly affecting women's quality of
life. Severe menorrhagia and dysmenorrhea should raise the suspicion so that TVS is scrutinized.
Presence of fibroids can potentially mask the presence of adenomyosis. MRI in selected cases maybe
required to confirm the diagnosis. When a trial of simple measures failed, uterine artery embolisation is
a safe, effective and much less invasive alternative to hysterectomy.
References on UAE and Adenomyosis
Kim MD, Kim S, Kim NK et al. (2007) Long-term results of uterine artery embolization for symptomatic adenomyosis. American Journal of Roentgenology 188:176-81
Smeets AJ, Nijenhuis RJ, Boekkooi PF et al. (2012) Long-term follow-up of uterine artery embolization for symptomatic adenomyosis. Cardiovascular & Interventional Radiology 35:815-9
Froeling V, Scheurig-Muenkler C, Hamm B et al. (2012) Uterine artery embolization to treat uterine adenomyosis with or without uterine leiomyomata: results of symptom control and health-related quality of life 40 months after treatment. Cardiovascular & Interventional Radiology 35:523-9
Bratby MJ and Walker WJ. (2009) Uterine artery embolisation for symptomatic adenomyosis--mid-term results. European Journal of Radiology 70:128-32
Lohle PN, De VJ, Klazen CA et al. (2007) Uterine artery embolization for symptomatic adenomyosis with or without uterine leiomyomas with the use of calibrated tris-acryl gelatin microspheres: midterm clinical and MR imaging follow-up. Journal of Vascular & Interventional Radiology 18:835-41
Pelage JP, Jacob D, Fazel A et al. (2005) Midterm results of uterine artery embolization for symptomatic adenomyosis: initial experience. Radiology 234:948-53
Siskin GP, Tublin ME, Stainken BF et al. (2001) Uterine artery embolization for the treatment of adenomyosis: clinical response and evaluation with MR imaging. American Journal of Roentgenology 177:297-302
Liang, E., Brown, B., Kirsop, R., Stewart, P., Stuart, A. (2012). Efficacy of uterine artery embolisation for treatment of symptomatic fibroids and adenomyosis - An interim report on an Australian experience. Australian and New Zealand Journal of Obstetrics and Gynaecology, 52(2), 106-112.
Source: http://www.sydneyfibroidclinic.com.au/Adenomyosis-Embolisation.pdf
LA LETTRE D'ACTUALITÉS N°143 - Septembre 2014 SOMMAIRE 1) Les infections respiratoires hautes Le mot de la rédaction 2) Les infections urinaires 3) Documentation Les aspects épidémiologiques concernant les maladies in-fectieuses pédiatriques sont de manière irrégulière et in- complète soumis à investigation.
AnnuAl BoArd updAte STATE OF NEVADA BOARD OF VETERINARY MEDICAL EXAMINERS From The President Richard Simmonds, DVM, MS Richard Simmonds, DVM, MS, ACLAM I am honored to have been selected by my is regulatory in nature and charged with enforcing colleagues on the Nevada Board of Veterinary the Nevada Practice Act and the Association is a Craig Schank, DVM