Mbainstitute.eu
NÚMERO 4. MAYO DE 2013
Resultados clínicos a largo
plazo de la prótesis total de
cadera Furlong H.A.C
25 años del implante pionero
en el uso de hidroxiapatita

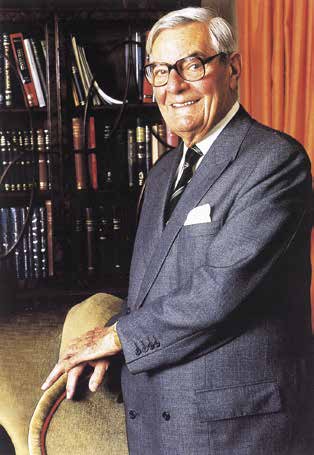
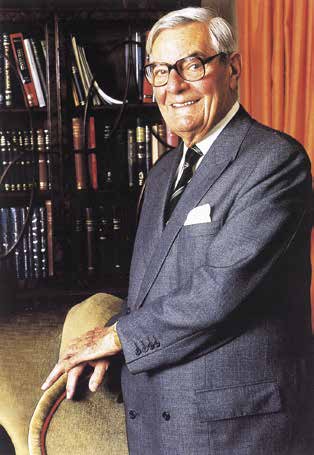
Ronald Furlong, pionero de la prótesis total de cadera recubierta con
hidroxiapatita, nació en Woolwich (Londres, Reino Unido) en 1909. Fue alumno
de Rowley Bristow, Director de Ortopedia del londinense Hospital St Thomas.
Estudiante brillante, se licenció en cirugía a una edad excepcionalmente
temprana.
En 1969 fue nombrado Director del Departamento de Ortopedia del Hospital St
Thomas, donde una de sus responsabilidades fue la enseñanza de la cirugía de
reemplazo de cadera. Sus dudas acerca de los implantes disponibles en aquel
momento le llevaron a estudiar biomecánica, y en 1978 fue galardonado con
la Medalla de Pauwels, siendo uno de los cinco poseedores de tal distinción en
todo el mundo.
Gracias a sus conocimientos de biomecánica comenzó a diseñar una nueva
prótesis, buscando en primer lugar la estabilidad mecánica de la misma.
El segundo objetivo era recubrir el implante con un agente bioactivo, que
permitiera una fijación fisiológica de larga duración. Su investigación acerca del
uso de hidroxiapatita le puso en contacto con el profesor Johannes Osborn, que
había escrito un libro y más de 30 artículos sobre la hidroxiapatita y su uso en el
tratamiento de las fracturas conminutas abiertas de la mandíbula.
Trabajando en colaboración con una empresa alemana de expertos en
tecnología de pulverización de plasma de llama, Furlong y Osborn lograron
desarrollar un recubrimiento para la prótesis de cadera. El resultado fue Furlong
HAC®, el primer implante revestido con recubrimiento de hidroxiapataita
osteoconductor.
La primera prótesis Furlong HAC® fue implantada en septiembre de 1985 y,
tras su éxito, en 1988 se fundó la Furlong Research Foundation, para apoyar la
investigación científica, la evaluación clínica y la difusión del conocimiento en
este campo. A la vista de los excelentes resultados los cirujanos siguen indicándola hoy
en día, convencidos de haber encontrado el buen camino para solucionar la
patología coxofemoral con una prótesis segura.
Artículos originales publicados en The Bone and Joint Journal (JBJS Br)
THE BRITISH EDITORIAL SOCIETY OF BONE & JOINT SURGERY
Registered charity no: 209299
BJJ Print ISSN: 2049-4394
Online ISSN: 2049-4408
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
Reemplazo total de
cadera primaria con
un vástago Furlong de
aleación de titanio con
recubrimiento completo
de hidroxiapatita
Resultados con un seguimiento mínimo de
20 años
Presentamos la extensión del seguimiento (≥ 20 años)
de una serie de vástagos femorales recubiertos con hi-
droxiapatita utilizados en 72 prótesis primarias de cade-
ra (PTC). Los resultados tempranos de esta cohorte ya
habían sido publicados previamente. Todos los procedi-
mientos fueron realizados entre 1986 y 1991. La serie
incluía a 45 mujeres, 15 hombres y 12 procedimientos
bilaterales. Su edad media en el momento de la cirugía
era de 60 años (46 a 80) y la duración media del segui-
miento ha sido de 22.5 años (20 a 25). En el seguimiento
final, la media de la escala de Merle d'Aubigne y Postel
fue de 5.5 (4.5 a 6), 3.8 (3.5 a 5) y 3.3 (3.0 a 5.0) para
dolor, movilidad y función, respectivamente. El 92% de
los pacientes estaban muy satisfechos en el momento del
seguimiento final.
Ha habido siete revisiones: seis del componente aceta-
bular por aflojamiento aséptico y otra por aflojamiento
acetábulo y del vástago debido a una infección profunda.
La supervivencia de esta prótesis a 22.5 años tomando
la revisión por cualquier causa como punto final es del
91.7% (intervalo de confianza al 95% de 84 a 99). La su-
pervivencia con aflojamiento aséptico del vástago como
punto final fue del 100% (intervalo de confianza al 95%
de 90 a 100).
Esta prótesis alivia el dolor en el largo plazo. La supervi-
vencia de este componente es comparable a los mejores
resultados en PTC primaria que emplee cualquier método
de fijación.
MBA Institute. Número 4. Mayo de 2013 / 3
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
HIP
Primary total hip replacement with a Furlong
fully hydroxyapatite-coated titanium alloy
femoral component
RESULTS AT A MINIMUM FOLLOW-UP OF 20 YEARS
We present the extended follow-up (≥ 20 years) of a series of fully hydroxyapatite-coated
C. Doctor,
femoral components used in 72 primary total hip replacements (THRs). Earlier results of this
S. S. Rajaratnam,
cohort have been previously published. All procedures were performed between 1986 and
S. Ahmed,
1991. The series involved 45 women and 15 men with 12 bilateral procedures. Their mean
D. J. East,
age at the time of surgery was 60 years (46 to 80) and the mean duration of follow-up was
K. Miles,
22.5 years (20 to 25). At final follow-up, the mean Merle d'Aubigné and Postel hip scores
were 5.5 (4.5 to 6), 3.8 (3.5 to 5) and 3.3 (3.0 to 5.0) for pain, mobility and function,
J. A. N. Shepperd
respectively. Of the patients 92% were very satisfied at the time of final follow-up.
There were seven revisions: six of the acetabular component for aseptic loosening and
From Conquest
one of both the stem and the acetabular component for loosening due to deep infection.
Hospital, St Leonards The survival of this prosthesis at 22.5 years with revision for any reason as the endpoint was
on Sea, United
91.7% (95% confidence interval (CI) 84 to 99). Survival with aseptic loosening of the stem as
the endpoint was 100% (95% CI 90 to 100).
This prosthesis provides pain relief in the long term. Survival of this component is
comparable to the best results for primary THR with any means of fixation.
N. Sandiford, MRCS,
Cite this article: Bone Joint J 2013;95-B:467–71.
MSc(SEM), SpR Trauma and Orthopaedics
Primary uncemented total hip replacement
prosthesis was used in our department for all
C. Doctor, MRCS, Senior House Officer in Trauma and
(THR) has become an accepted method of pro-
patients in whom an uncemented THR was
viding pain relief and return to function in
required. All procedures were performed by or
D. J. East, DPT, MSc, Head of Research
patients with symptomatic osteoarthritis (OA)
under the direct supervision of a single surgeon
K. Miles, DPT, Research
of the hip. Good medium-term results have been
(JANS). No patients were lost to follow-up.
Physiotherapist A. Butler-Manuel, FRCS,
reported with the use of partially1,2 as well as
Bilateral procedures were performed in
Consultant Orthopaedic and
fully hydroxyapatite (HA)-coated femoral com-
12 patients (four men, eight women). These
Trauma Surgeon J. A. N. Shepperd, FRCS,
ponents at follow-up of up to ten years.3,4
were staged procedures in five patients and
Consultant Orthopaedic and
A recent review identified relatively few
under the same anaesthetic in seven. The mean
Trauma SurgeonConquest Hospital, The Ridge,
long-term survival reports on uncemented fem-
age of this cohort was 82.9 years (70 to 100) at
St Leonards on Sea, Hastings
oral components.5 Only 17 unique studies
the final follow-up. At the time of surgery
TN37 7RD, UK.
were found that included a minimum of
11 patients were < 55 years of age (Table I). All
S. S. Rajaratnam,
50 patients. Two reviews of registry data com-
patients presented with disabling hip pain.
FRCS(Orth), Consultant Orthopaedic and Trauma
paring > 150 patients were found with follow-
Surgical technique and prosthesis. All proce-
up periods > 15 years. A total of 16 femoral
dures were performed via a Watson Jones
S. Ahmed, MRCS, SpR Trauma and Orthopaedics
components were included, both HA- and non-
approach6 with the patient in the supine posi-
Eastbourne District General
HA coated. Survival rates > 90% were found
tion. Each patient received three doses of pro-
Hospital, King's Drive, Eastbourne, East Sussex BN21
for these uncemented stems.5
phylactic antibiotics and subsequently were
This study presents the results at a minimum
allowed to bear full weight on the first post-
Correspondence should be sent
20-year follow-up of a previously reported
operative day.
to Mr N. A. Sandiford; e-mail: [email protected]
cohort of patients treated with a fully HA-
The Furlong femoral component (JRI Ltd)
coated femoral component.
was used in all cases. This is manufactured from
2013 The British Editorial Society of Bone and Joint
a titanium alloy (Ti-6Al-4V). The surface of the
Patients and Methods
body and distal stem are plasma sprayed with a
doi:10.1302/0301-620X.95B4. 30445 $2.00
This prospective study was performed between
200 μm-thick layer of hydroxyapatite of high
1986 and 1991 and includes 72 primary THRs
crystallinity. The stem is collared and designed
Bone Joint J 2013;95-B:467–71.
performed in 60 patients (45 women and
to achieve primary stability via a metaphyseal
Received 13 July 2012;
15 men) using the Furlong femoral component
fit, and has a trunnion with a 12/14 Morse
Accepted after revision 10 January 2013
(JRI Ltd, London, United Kingdom). This
taper. A Furlong UHMWPE acetabular
VOL. 95-B, No. 4, APRIL 2013
4 / MBA Institute. Número 4. Mayo de 2013
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
N. SANDIFORD, C. DOCTOR, S. S. RAJARATNAM, S. AHMED, D. J. EAST, K. MILES, A. BUTLER-MANUEL, J. A. N. SHEPPERD
Table I. Characteristics of the 60 patients at operation
Kaplan-Meier method with 95% confidence intervals (CI).
All analyses were performed using GraphPad software
Characteristic
Gender (n, %)
(GraphPad, San Diego, California).
Results
The mean duration of follow-up was 22.5 years (20 to 25).
Mean age at surgery (yrs) (range)
At the last follow-up the mean scores for the pain, mobility
and function components of the MDP score were 5.5 (4.5to 6), 3.8 (3.5 to 5) and 3.3 (3.0 to 5.0), respectively. Two
patients (3.3%) were not satisfied, three (5%) were moder-
ately satisfied and 55 (91.7%) were very satisfied with their
result up to the last follow-up. The latter group had a VAS
Bilateral procedures
≥ 8. Clinical improvement was noted at the six-week fol-low-up and was maintained. All patients reported excellentpain relief at their last review.
The mean MDP scores for pain, function and mobility at
component was used in 47 patients (59 hips) and a HA-
ten years were 5.8 (4 to 6), 5.6 (3 to 6) and 5.5 (1 to 6),
coated threaded acetabular shell with an ultra-high molecu-
respectively, and at 17 years they were 5.6 (3 to 6), 5.4 (2 to
lar weight polyethylene (UHMWPE) liner (JRI Ltd) was used
6) and 3.8 (0 to 6), respectively. There was no statistically
in 13 patients (13 hips). A modular 32 mm ceramic femoral
significant difference between the ten- and 17-year MDP
head was used in all hips.
scores (p = 0.87). Similarly, there was no significant differ-
Follow-up. Clinical and radiological follow-up was per-
ence between these parameters between the 17- to 22.5-year
formed at six weeks, 12 weeks, six months and 12 months
follow-up (p = 0.82).
post-operatively, and annually thereafter. Patients were
In all, at the final review 17 patients (17 hips) had died:
interviewed, examined, the wound was assessed, and all
six at 20 years post-operatively, four at 21 years, three at
medical and surgical complications were documented. Spe-
22 years, three at 23 years and one at 25 years post-
cific enquiry was made about anterior thigh pain. Clinical
operatively. Their deaths were not related to their hip sur-
assessment of pain, mobility and function was performed
gery. These patients were all reviewed within a year of their
using the Merle d'Aubigné and Postel (MDP) scoring sys-
deaths and were therefore included in this study. We
tem.7 Patient satisfaction was assessed using a visual ana-
reviewed their clinical notes as well as their radiographs
logue scale (VAS), which ranged from 0 (poor satisfaction)
and contacted their GPs to determine whether they had any
to 10 (high satisfaction).
complaints regarding their hips, and none were identified.
Radiological review. At each visit anteroposterior (AP) and
A total of seven patients (seven hips) had undergone revi-
lateral radiographs of the pelvis and operated hip were
sion surgery. This involved both components in one patient
obtained and reviewed by two separate reviewers (NS, CD).
and the acetabular component alone in six. Loosening of the
These were examined for changes in the position or orien-
femoral component occurred in one patient 21 years after
tation of the components as well as for evidence of osseo-
their primary procedure associated with deep infection. This
integration or loosening of the prosthesis.
was the patient who had both components revised and
Signs of loosening included lytic lesions (balloon-shaped
accounted for the only stem revision in this series. There were
lucencies around the prosthesis), migration of the implant
no cases of aseptic loosening of the stem in this cohort. At final
(measured as the distance between the shoulder of the
follow-up one female patient was awaiting revision of the ace-
implant and the greater trochanter), radiolucent lines (RLL;
tabular component but had a well-fixed femoral component
linear lucencies > 2 mm at the bone–prosthesis interface8
in situ. There were no dislocations in this group.
and occupying > 30% of any Gruen zone9). Solid fixation
Survival analysis. With revision of the femoral component
was indicated by ‘spot welding' and trabeculae of cancel-
for any reason as the endpoint, survival at a mean follow-
lous bone extending to the stem as described by Engh,
up of 22.5 years was 98% (95% CI 90 to 99). With revision
Sychterz and Engh.10
for aseptic loosening as the endpoint survival was 100%
Radiographs were also assessed for signs of heterotopic
(95% CI 90 to 100) (Fig. 1). If we consider the endpoint to
ossification (HO) and stress shielding of the calcar region of
be revision for any reason, then survival of the femoral
the femur: HO was classified according to the system of
component was 91% (95% CI 88.6 to 98.9) at a mean
Brooker et al,11 and stress shielding was considered to be
22.5 years follow-up (Fig. 2).
significant if there was selective bone resorption of the cal-
Radiological results. There were no cases of subsidence of
car region of the femoral neck.12
the femoral components. Radiological evidence of solid
Statistical analysis. Statistical analysis was performed
stem fixation, including ‘spot weld' formation12 as well as
using Student's t-test. The level of significance was set at
an osteoblastic reaction at the stem tip, was observed in all
p < 0.05. Survival analysis was performed using the
radiographs (Fig. 3).
THE BONE & JOINT JOURNAL
MBA Institute. Número 4. Mayo de 2013 / 5
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
PRIMARY TOTAL HIP REPLACEMENT WITH A FURLONG FULLY HYDROXYAPATITE-COATED TITANIUM ALLOY FEMORAL COMPONENT
Radiograph of an hydroxyapatite-coated Furlong stem at
25 years post-operatively, showing an osteoblastic reaction
at the tip of the stem (A), trabeculae extending to the surface
of the prosthesis (B), and localised bone resorption immedi-
ately under the polished collar (C).
Kaplan-Meier survival curve with 95% confidence intervals, showing
revision for aseptic loosening as the endpoint.
Table II. Radiolucent lines around the femoral and acetabular com-
ponents at the last follow-up
Femoral component Acetabular component
Zones of interest
(number of patients)
15 (zones 1, 2 &3)
two lived independently at the time of final follow-up withno expressed concerns about their operated hips.
The radiolucent lines were predominantly present in
Gruen zones 2 and 3. They were 1 mm wide and non-pro-
gressive over two years (Table II). They were not associatedwith pain and there were no overt signs of movement of the
femoral components.
Kaplan-Meier survival curve with 95% confidence intervals, illustrating the
Focal areas of resorption of the calcar were noted in ten
worst-case survival scenario with all revisions considered as failures.
hips (Fig. 3). This feature was associated with signs of goodfixation of the metaphyseal segment. These patients had nocomplaints that might suggest loosening of the implant. On
Radiolucent lines were seen in 19 femoral components. Of
35 radiographs (48.6%) HO was observed. This was
this group, 16 patients (16 hips) died at a mean of 22.0 years
Brooker grade 2 or 3 in 57.1% of cases (Table III).
(20 to 23) post-operatively. One of these patients had
RLLs were noted around 29 acetabular components
undergone isolated revision of the acetabular component for
(40.3%). These were present in DeLee and Charnley13 zone
wear and loosening two years before death. Specific enquiry
1 (12 hips), zone 2 (five hips) and zones 1 to 3 (15 hips).
of their GPs, family members and review of their notes
Five patients (five hips), all of whom had RLLs in acetabu-
implied no complaints regarding their hips between their last
lar zones 1 to 3, had mild to moderate start-up pain. How-
clinical review and the time of their deaths. Of the three
ever, four patients did not wish to have any further surgery
patients who were alive, one had undergone revision of the
because of their age, and one was awaiting acetabular revi-
femoral component for septic loosening and the remaining
sion at the time of final follow-up.
VOL. 95-B, No. 4, APRIL 2013
6 / MBA Institute. Número 4. Mayo de 2013
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
N. SANDIFORD, C. DOCTOR, S. S. RAJARATNAM, S. AHMED, D. J. EAST, K. MILES, A. BUTLER-MANUEL, J. A. N. SHEPPERD
Table III. Distribution of hetero-
reports of the Furlong femoral component in primary THR
topic ossification according to
have been encouraging, with survival rates of 100% and
97.4% at ten and 17 years, respectively.3,22 In this now
extended series, survivorship of the remaining femoral com-
ponents with aseptic loosening as the endpoint at a mean
22.5-year follow-up is 100% (Fig. 1). If all revisions includ-ing those for the acetabulum and revision for infection areconsidered to be failures, then survivorship is 91%.
The mobility and functional components of the MDP
score show a gradual deterioration from ten to 22.5 years,whereas the pain score shows that pain relief continues tobe sustained. We believe this reflects an age-related decreasein general function and mobility. This change was not sta-tistically significant at any of the three measured timepoints up to a mean of 22.5 years. It is likely that the lackof pain contributed to the high levels of satisfactionreported by 96.7% of this cohort.
All femoral stems showed signs of stable fixation (Fig. 3).
Although focal areas of bone resorption were noted in thecalcar region immediately adjacent to the collar in tenpatients (Fig.3), this did not correspond to pain or decreasedfunction. This may possibly relate to localised stress shield-ing of the calcar region immediately adjacent to the collar
after full bonding of the bone to implant had occurred. RLLswere noted around acetabular components in 29 patients
Radiograph showing an asymptomatic peri-
prosthetic fracture at 25 years post-operatively.
(29 hips), which in 52% involved zones 1 to 3.
High early revision rates for uncemented primary THR are
thought by some to be due predominantly to peri-prostheticfractures occurring during stem insertion.23 Our patients
Complications. There were four calcar fractures that
experienced four such fractures but recovered without seque-
occurred at the time of the original surgery. These were
lae. Merle et al5 alluded to the paucity of true long-term
treated with cerclage wires in one hip and conservatively in
results for uncemented stems. They found good to excellent
three hips. All patients with these fractures were mobilised
results with these components at a minimum of 15 years, and
non-weight-bearing with crutches for the first six weeks
suggested that this technique of fixation is reliable and should
after their procedure. This included the one patient who
become a standard treatment option in appropriate patients.
developed a deep infection 21 years after surgery, which
The 2010 report of the Swedish Hip Registry found no
was successfully treated with a two-stage revision. No
significant differences between cemented and uncemented
patients reported anterior thigh pain.
fixation regarding the risk of revision, irrespective of
At the final follow-up a peri-prosthetic fracture was
cause.23 Data from the ninth report of the United Kingdom
noted in an asymptomatic male patient (Fig. 4) who, on
National Joint Registry24 suggest that the use of unce-
enquiry, had no history of trauma or pain. The femoral
mented components is increasing but is associated with a
stem was well fixed radiologically and there were no clini-
higher revision rate for uncemented components in the first
cal signs of pain or impaired mobility. The time and cause
ten years. The lowest revision rates up to this point have
of this injury remains uncertain.
been found for cemented components. Between four andeight years the revision rates for uncemented components
Discussion
with the ceramic-on-polyethylene bearing couple have been
Our results represent those of a non-designer surgeon
the lowest of all combinations of uncemented components.
series. They suggest that HA-coated fixation remains
Data from the Swedish registry demonstrates that after the
reliable and predictable in the long term, even as the patient
nine- to ten-year period the failure rate for cemented com-
ages and the corticomedullary ratio of the femur
ponents surpasses that for uncemented components.
increases.14 The fact that HA is soluble in vivo and possibly
There are several limitations to this study. The sample size
delaminates does not seem to affect long-term survival.15
is small, as the number of patients who remained alive has
Good long-term results of primary THR using fully HA-
decreased. No pre-operative MDP scores were recorded.
coated titanium stems have been reported in young as well as
However, our database provides an accurate record of scores
older age groups.3,16-22 Similar results have been reported
from the time of surgery, and the VAS was consistently used
when these stems are used in the revision setting.21 Previous
as a patient-reported tool to augment our clinical data.
THE BONE & JOINT JOURNAL
MBA Institute. Número 4. Mayo de 2013 / 7
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
PRIMARY TOTAL HIP REPLACEMENT WITH A FURLONG FULLY HYDROXYAPATITE-COATED TITANIUM ALLOY FEMORAL COMPONENT
Our cohort reported significant improvements in pain,
12. McCullough CJ, Remedios D, Tytherleigh-Strong G, Hua J, Walker PS. The
mobility and function in their early post-operative phase
use of hydroxyapatite-coated CAD-CAM femoral components in adolescents and
young adults with inflammatory polyarthropathy: ten-year results. J Bone Joint
that has been maintained at the ten-, 17- and now 22.5-
Surg [Br] 2006;88-B:860–864.
year follow-up. There were no cases of aseptic loosening
13. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip
of the femoral component. These results are comparable
replacement. Clin Orthop Relat Res 1976;121:20–32.
to the best long-term outcomes in terms of both survival
14. Beaupied H, Lespessailles E, Benhamou CL. Evaluation of macrostructural
bone biomechanics. Joint Bone Spine 2007;74:233–239.
of the component and maintained clinical results for
15. Epinette JA, Manley MT. Uncemented stems in hip replacement--hydroxyapatite
primary THR with any means of fixation of the femoral
or plain porous: does it matter? Based on a prospective study of HA Omnifit stems
at 15-years minimum follow-up. Hip Int 2008;18:69–74.
16. Shetty AA, Slack R, Tindall A, James KD, Rand C. Results of a hydroxyapatite
No benefits in any form have been received or will be received from a commer-
coated (Furlong) total hip replacement: a 13- to 15-year follow-up. J Bone Joint
cial party related directly or indirectly to the subject of this article.
Surg [Br] 2005;87-B:1050–1054.
This article was primary edited by G. Scott and first-proof edited by D. Rowley.
17. Robertson A, Lavalette D, Morgan S, Angus PD. The hydroxyapatite coated
JRI-Furlong hip: outcome in patients under the age of 55 years. J Bone Joint Surg
18. Hallan G, Lie SA, Furnes O, et al. Medium- and long-term performance of 11,516
1. Mannan K, Freeman MA, Scott G. The Freeman femoral component with
uncemented primary femoral stems from the Norwegian arthroplasty register. J
hydroxyapatite coating and retention of the neck: an update with a minimum follow-
Bone Joint Surg [Br] 2007;89-B:1574–1580.
up of 17 years. J Bone Joint Surg [Br] 2010;92-B:480–485.
19. Gabbar OA, Rajan RA, Londhe S, Hyde ID. Ten- to twelve-year follow-up of the
2. Muirhead-Allwood SK, Sandiford N, Skinner JA, et al. Uncemented custom
furlong hydroxyapatite-coated femoral stem and threaded acetabular cup in
computer-assisted design and manufacture of hydroxyapatite-coated femoral compo-
patients younger than 65 years. J Arthroplasty 2008;23:413–417.
nents: survival at 10 to 17 years. J Bone Joint Surg [Br] 2010;92-B:1079–1084.
20. Vidalain JP. Twenty-year results of the cementless Corail stem. Int Orthop
3. McNally SA, Shepperd JA, Mann CV, Walczak JP. The results at nine to twelve
years of the use of a hydroxyapatite-coated femoral stem. J Bone Joint Surg [Br]
21. Trikha SP, Singh S, Raynham OW, et al. Hydroxyapatite ceramic coated femoral
stems in revision hip surgery. J Bone Joint Surg [Br] 2005;87-B:1055–1060.
4. Vidalain JP. HA coating: ten-year experience with the CORAIL system in primary
22. Rajaratnam SS, Jack C, Tavakkolizadeh A, et al. Long-term results of a
THA: the Artro Group. Acta Orthop Belg 1997;63(Suppl):93–95.
hydroxyapatite-coated femoral component in total hip replacement: a 15- to 21-
5. Merle C, Clarius M, Aldinger PR. Long-term results of uncemented stems in total
year follow-up study. J Bone Joint Surg [Br] 2008;90-B:27–30.
hip arthroplasty: analysis of survival rates with a minimum 15-year follow-up. Ortho-
23. No authors listed. Swedish Hip Arthroplasty Register. Annual Report 2010. http:/
pade 2010;39:80–86 (in German).
/www.shpr.se/en/Publications/DocumentsReports.aspx (date last accessed 16
January 2013).
6. Hart FD, Watson-Jones R. Arthritis of the hip. Trans Med Soc Lond 1956;72:33–44.
24. No authors listed. National Joint Registry for England and Wales: Ninth Annual
7. Merle d'Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic
prosthesis. J Bone Joint Surg [Am] 1954;36-A:451–475.
8. Manaster JF, Andrews CL, Conway F, Fleckenstein JL, Kaplan PA. Musculo-
last accessed 10 February 2013).
skeletal radiology. Radiology 1996;198:618–621.
25. Hallan G, Lie SA, Furnes O, et al. Medium- and long-term performance of 11,516
9. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type
uncemented primary femoral stems from the Norwegian arthroplasty register. J
femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res
Bone Joint Surg [Br] 2007;89-B:1574–1580.
26. Carrington NC, Sierra RJ, Gie GA, et al. The Exeter Universal cemented femoral
10. Engh CA Jr, Sychterz C, Engh C Sr. Factors affecting femoral bone remodelling
component at 15 to 17 years: an update on the first 325 hips. J Bone Joint Surg [Br]
after cementless total hip arthroplasty. J Arthroplasty 1999;14:637–644.
11. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification fol-
27. Lehtimäki MY, Lehto MU, Kautiainen H, Savolainen HA, Hämäläinen MM.
lowing total hip replacement: incidence and a method of classification. J Bone Joint
Survivorship of the Charnley total hip arthroplasty in juvenile chronic arthritis: a fol-
Surg [Am] 1973;55-A:1629–1632.
low-up of 186 cases for 22 years. J Bone Joint Surg [Br] 1997;79-B:792–795.
VOL. 95-B, No. 4, APRIL 2013
8 / MBA Institute. Número 4. Mayo de 2013
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
PRIMARY TOTAL HIP REPLACEMENT WITH A FURLONG FULLY HYDROXYAPATITE-COATED TITANIUM ALLOY FEMORAL COMPONENT
Our cohort reported significant improvements in pain,
12. McCullough CJ, Remedios D, Tytherleigh-Strong G, Hua J, Walker PS. The
Uso de componentes
mobility and function in their early post-operative phase
use of hydroxyapatite-coated CAD-CAM femoral components in adolescents and
young adults with inflammatory polyarthropathy: ten-year results. J Bone Joint
that has been maintained at the ten-, 17- and now 22.5-
Surg [Br] 2006;88-B:860–864.
femorales recubiertos
year follow-up. There were no cases of aseptic loosening
13. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip
of the femoral component. These results are comparable
replacement. Clin Orthop Relat Res 1976;121:20–32.
de hidroxiapatita en
to the best long-term outcomes in terms of both survival
14. Beaupied H, Lespessailles E, Benhamou CL. Evaluation of macrostructural
bone biomechanics. Joint Bone Spine 2007;74:233–239.
pacientes jóvenes con
of the component and maintained clinical results for
15. Epinette JA, Manley MT. Uncemented stems in hip replacement--hydroxyapatite
primary THR with any means of fixation of the femoral
or plain porous: does it matter? Based on a prospective study of HA Omnifit stems
seguimientos de entre 16
at 15-years minimum follow-up. Hip Int 2008;18:69–74.
16. Shetty AA, Slack R, Tindall A, James KD, Rand C. Results of a hydroxyapatite
y 19 años
No benefits in any form have been received or will be received from a commer-
coated (Furlong) total hip replacement: a 13- to 15-year follow-up. J Bone Joint
cial party related directly or indirectly to the subject of this article.
Surg [Br] 2005;87-B:1050–1054.
Actualización de una publicación anterior
This article was primary edited by G. Scott and first-proof edited by D. Rowley.
17. Robertson A, Lavalette D, Morgan S, Angus PD. The hydroxyapatite coated
JRI-Furlong hip: outcome in patients under the age of 55 years. J Bone Joint Surg
En 2004 describimos los resultados prospectivos a diez
18. Hallan G, Lie SA, Furnes O, et al. Medium- and long-term performance of 11,516
1. Mannan K, Freeman MA, Scott G. The Freeman femoral component with
uncemented primary femoral stems from the Norwegian arthroplasty register. J
años de 38 reemplazos de cadera empleando el vástago
hydroxyapatite coating and retention of the neck: an update with a minimum follow-
Bone Joint Surg [Br] 2007;89-B:1574–1580.
femoral recubierto de hidroxiapatita Furlong en 35 pa-
up of 17 years. J Bone Joint Surg [Br] 2010;92-B:480–485.
19. Gabbar OA, Rajan RA, Londhe S, Hyde ID. Ten- to twelve-year follow-up of the
cientes con menos de 50 años de edad. Ahora hemos re-
2. Muirhead-Allwood SK, Sandiford N, Skinner JA, et al. Uncemented custom
furlong hydroxyapatite-coated femoral stem and threaded acetabular cup in
visado las 35 artroplastias supervivientes en 33 pacientes
computer-assisted design and manufacture of hydroxyapatite-coated femoral compo-
patients younger than 65 years. J Arthroplasty 2008;23:413–417.
nents: survival at 10 to 17 years. J Bone Joint Surg [Br] 2010;92-B:1079–1084.
20. Vidalain JP. Twenty-year results of the cementless Corail stem. Int Orthop
con una media de 16 años (10.3 a 19.9). La edad media
3. McNally SA, Shepperd JA, Mann CV, Walczak JP. The results at nine to twelve
de los pacientes supervivientes en el momento de la ope-
years of the use of a hydroxyapatite-coated femoral stem. J Bone Joint Surg [Br]
21. Trikha SP, Singh S, Raynham OW, et al. Hydroxyapatite ceramic coated femoral
ración era de 41.3 años (26.0 a 49.0). De estos, ocho han
stems in revision hip surgery. J Bone Joint Surg [Br] 2005;87-B:1055–1060.
sufrido la revisión de su componente acetabular por aflo-
4. Vidalain JP. HA coating: ten-year experience with the CORAIL system in primary
22. Rajaratnam SS, Jack C, Tavakkolizadeh A, et al. Long-term results of a
THA: the Artro Group. Acta Orthop Belg 1997;63(Suppl):93–95.
hydroxyapatite-coated femoral component in total hip replacement: a 15- to 21-
jamiento aséptico. Ninguno de los componentes femora-
5. Merle C, Clarius M, Aldinger PR. Long-term results of uncemented stems in total
year follow-up study. J Bone Joint Surg [Br] 2008;90-B:27–30.
les ha sufrido revisión por aflojamiento aséptico, siendo
hip arthroplasty: analysis of survival rates with a minimum 15-year follow-up. Ortho-
23. No authors listed. Swedish Hip Arthroplasty Register. Annual Report 2010. http:/
su tasa de supervivencia del 100% a 16 años (intervalo de
pade 2010;39:80–86 (in German).
/www.shpr.se/en/Publications/DocumentsReports.aspx (date last accessed 16
January 2013).
confianza al 95% de 89% a 100%).
6. Hart FD, Watson-Jones R. Arthritis of the hip. Trans Med Soc Lond 1956;72:33–44.
24. No authors listed. National Joint Registry for England and Wales: Ninth Annual
7. Merle d'Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic
El vástago recubierto de hidroxiapatita Furlong ofrece un
prosthesis. J Bone Joint Surg [Am] 1954;36-A:451–475.
comportamiento excelente en supervivencia a largo plazo
8. Manaster JF, Andrews CL, Conway F, Fleckenstein JL, Kaplan PA. Musculo-
last accessed 10 February 2013).
en pacientes jóvenes y activos.
skeletal radiology. Radiology 1996;198:618–621.
25. Hallan G, Lie SA, Furnes O, et al. Medium- and long-term performance of 11,516
9. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type
uncemented primary femoral stems from the Norwegian arthroplasty register. J
femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res
Bone Joint Surg [Br] 2007;89-B:1574–1580.
26. Carrington NC, Sierra RJ, Gie GA, et al. The Exeter Universal cemented femoral
10. Engh CA Jr, Sychterz C, Engh C Sr. Factors affecting femoral bone remodelling
component at 15 to 17 years: an update on the first 325 hips. J Bone Joint Surg [Br]
after cementless total hip arthroplasty. J Arthroplasty 1999;14:637–644.
11. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification fol-
27. Lehtimäki MY, Lehto MU, Kautiainen H, Savolainen HA, Hämäläinen MM.
lowing total hip replacement: incidence and a method of classification. J Bone Joint
Survivorship of the Charnley total hip arthroplasty in juvenile chronic arthritis: a fol-
Surg [Am] 1973;55-A:1629–1632.
low-up of 186 cases for 22 years. J Bone Joint Surg [Br] 1997;79-B:792–795.
VOL. 95-B, No. 4, APRIL 2013
MBA Institute. Número 4. Mayo de 2013 / 9
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
Hydroxyapatite-ceramic-coated femoral
components in young patients followed-up
for 16 to 19 years
AN UPDATE OF A PREVIOUS REPORT
N. N. Shah,
In 2004 we described the ten-year prospective results of 38 total hip replacements using the
A. J. Edge,
Furlong hydroxyapatite-ceramic-coated femoral component in 35 patients < 50 years old. We
D. W. Clark
have now reviewed the surviving 35 arthroplasties in 33 patients at a mean of 16 years
(10.3 to 19.9). The mean age of the surviving patients at the time of operation was 41.3 years
From Worthing and
(26.0 to 49.0). Of these, eight have undergone revision of their acetabular component for
Southlands Hospitals
aseptic loosening. None of the femoral components has had revision for aseptic loosening
NHS Trust,
giving a survival rate of 100% at 16 years (95% confidence interval 89% to 100%).
Shoreham-by-Sea,
The Furlong hydroxyapatite-ceramic-coated femoral component gives excellent long-term
survival in young and active patients.
Previous studies have shown that cemented
in one (3%), rheumatoid arthritis in one (3%)
total hip replacement (THR) is a successful
and Still's disease in two (5%) (Table I).
procedure in elderly and low-demand patients,
Staged bilateral procedures were performed
but the failure rate is higher in young and active
in four patients and one patient had both hips
patients.1-3 Long-term failure of cemented
replaced under the same anaesthetic. Although
THR components is usually due to aseptic
the Furlong HAC-coated stem was used in all
loosening caused by wear debris stimulating
patients the acetabular components varied. The
the formation of osteoclasts and subsequent
initial 14 hips (37%) received a cemented poly-
osteolysis. Hydroxyapatite-ceramic (HAC)-
ethylene component (JRI) and the remaining 24
coated implants facilitate a biological bond
had JRI Cancellous Screw Fixation HAC-
between the implant and bone producing a
coated acetabular components with polyethyl-
ene liners. Alumina oxide ceramic modular
In November 2004 we described the results
heads were used in 36 hips of which 23 were of
at ten years of the use of the HAC-coated
28 mm and 13 of 32 mm in diameter. Cobalt-
Furlong implant (Joint Replacement Instru-
chrome heads were used in two hips, one of
mentation (JRI), London, United Kingdom)
28 mm and one of 32 mm diameter.
which showed no evidence of aseptic loosen-
The Harris hip score (HHS)7 was completed
N. N. Shah, MS, MSc, MCh(Orth), FRCS(Trauma &
ing.5 We have now reviewed the same series at
pre-operatively and at a mean follow-up of
Orth), Furlong Clinical Fellow
a mean of 16 years (10.3 to 19.9).
16.0 years (10.3 to 19.9) and the Oxford hip
A. J. Edge, FRCS, Consultant Orthopaedic Surgeon
score (OHS),8 University of California Los
D. W. Clark, FRCS, Consultant
Patients and Methods
Angeles (UCLA) activity scale9 and patient sat-
Orthopaedic SurgeonWorthing & Southlands
Between December 1988 and October 1997,
isfaction were also used as outcome measures.
Hospitals NHS Trust,
38 THRs in 33 patients (22 men, 11 women)
Radiological assessment was carried out
Southlands Hospital, Upper Shoreham Road, Shoreham-
with a mean age of 42 years (22 to 49) were
by independent observers (NNS, DWC).
by-Sea, West Sussex BN43
performed by the senior author (AJE) or under
Anteroposterior (AP) radiographs of the
his direct supervision using the Hardinge
pelvis were assessed for stability and fixation
Correspondence should be sent to Mr N. N. Shah; e-mail:
approach.6 All these patients were recalled for
of the femoral component according to the
further follow-up and clinical and radiological
criteria described by Engh, Massin and
2009 British Editorial Society
evaluation. The series has been described in
Suthers.10 Lateral radiographs were also
of Bone and Joint Surgery
detail previously5 (Table I).
reviewed at the final follow-up. The distribu-
doi:10.1302/0301-620X.91B7. 22311 $2.00
The principal diagnosis was osteoarthritis in
tion of osteolysis or radiolucencies was
19 hips (50%), developmental dysplasia of the
recorded according to the zones of Gruen,
J Bone Joint Surg [Br] 2009;91-B:865-9.
hip (DDH) in ten (26%), post-traumatic
McNeice and Amstutz11 using the criteria of
Received 16 January 2009;
arthritis in three (8%), Perthes' disease in two
Goetz, Smith and Harris.12 The femoral com-
Accepted after revision 27 February 2009
(5%), slipped upper femoral epiphysis (SUFE)
ponent was considered to be stable if there
VOL. 91-B, No. 7, JULY 2009
10 / MBA Institute. Número 4. Mayo de 2013

Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
N. N. SHAH, A. J. EDGE, D. W. CLARK
Table I. The indications for total hip replacement and the distribution of implants in the original series of 33
patients (38 hips)5
HAC* Furlong stem
Developmental dysplasia
Post-traumatic arthritis
Acetabular components
Cemented polyethylene
Slipped upper femoral epiphysis 1
JRI cancellous screw fixation HAC-coated with polyethylene liners
Rheumatoid arthritis
Modular headsAlumina ceramic
* HAC, hydroxyapatite-ceramic
heterotopic bone was recorded according to the criteria of
Brooker et al.14
Statistical analysis. The changes in the pre- and post-
operative hip scores were compared using the Mann-
Whitney U test. A p-value ≤ 0.05 was considered to be signif-
icant. Cumulative survival analysis for both components was
performed using revision for any reason and revision for
aseptic loosening or impending revision as the endpoints,
with 95% confidence intervals (CI).
Results
At the time of this review two patients (three hips) had
died from unrelated causes. One of these (one hip) had
osteoarthritis and the other had Still's disease (2 hips).
One patient had moved and was unable to attend, but
completed a postal questionnaire. The remaining 34
THRs in 30 patients (19 men, 11 women) from the origi-
nal series5 were available for follow-up and radiological
study and were included in the statistical analysis. The
mean age at operation of these patients was 41.3 years
(26.0 to 49.0).
Clinical and radiological findings. The mean pre-operative
Radiograph showing the Furlong hydroxyapatite-
HHS for the original series was 44 (31 to 55).5 The mean
ceramic-coated hip replacement with the Gruen zones.11
Increased formation of bone is seen in zones 2 to 6 and
post-operative HHS at the final review was 89 (78 to 100).
rounding of the calcar under the collar in zone 7.
For the eight patients who underwent revision of theacetabular component the mean post-operative HHS was92 (71 to 100) and for the remaining patients it was 86(78 to 100). This was statistically significant (Mann-Whit-
was evidence of osseointegration and unstable if there
ney U test, p < 0.001). The mean OHS was 16 (12 to 40) at
was evidence of migration. Additionally, the leg length
the ten-year follow-up5 and 18 (12 to 40) at this latest fol-
was measured directly from the radiographs.
low-up which was also statistically significant (Mann-
On the AP view osteolysis or radiolucencies around the
Whitney U test, p < 0.001). The UCLA activity score was 7
acetabular component were recorded as described by DeLee
or more for 21 patients with a mean of 6 (6 to 9) at the
and Charnley.13 The acetabular component was considered
final review.
to be loose if there was a continuous or progressive radio-
All the patients were asked at each review about the
lucent line at the prosthesis-bone interface or any change in
occurrence of anterior thigh pain. None had experienced
position of the acetabular component. The formation of
this at any stage.
THE JOURNAL OF BONE AND JOINT SURGERY
MBA Institute. Número 4. Mayo de 2013 / 11
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
HYDROXYAPATITE-CERAMIC-COATED FEMORAL COMPONENTS IN YOUNG PATIENTS FOLLOWED-UP FOR 16 TO 19 YEARS
Table II. The cumulative survival for the Furlong stem
Years since
Effective number
Cumulative
survival rate (%)
ments. This was reduced and fixed by a cable/plate system.
At operation it was noted that the femoral component was
well bonded. The fracture healed satisfactorily. Despite his
extensive surgery he was capable of working as an office
clerk and walked with one stick.
From measurements on the AP pelvic radiographs a leg-
length discrepancy was found in 14 hips. In six the shorten-
ing was between 5 mm and 1 cm and in eight there was
lengthening between 5 mm and 12 mm. At the latest review
of 12 surviving cemented polyethylene acetabular compo-
nents, five had required revision because of aseptic loosen-
ing associated with polyethylene wear. The mean time from
Time since operation (yrs)
primary surgery to revision was 11 years (9 to 13). Four
had a head diameter of 32 mm while the other had a mod-
The cumulative survival curve for the Furlong femoral component with
ular head diameter of 28 mm. They were all revised to can-
the 95% confidence interval shown.
cellous screw fixation acetabular components withceramic-on-ceramic bearing surfaces.
Of 22 HAC-coated cancellous screw fixation acetabu-
lar components, three were revised because of asepticloosening associated with radiolucency in DeLee and
Peri-operative complications were rare. There were no
Charnley zones 1 and 2. The diameter of the femoral head
cases of infection or thromboembolism. One patient had a
was 28 mm for these three patients. They were all revised
dislocation after 12 years. This patient had a cemented
to HAC-coated cancellous screw fixation acetabular com-
polyethylene acetabular component articulating with a
ponents with ceramic inserts. One required additional
32 mm ceramic head. Acetabular revision was performed
for aseptic loosening and polyethylene wear. There were no
Radiological assessment of the femoral components did not
peri-operative fractures associated with insertion of the
show any radiolucent lines and serial radiographs did not
Furlong stem. One late complication occurred in a 27-year-
reveal any evidence of subsidence. All were stable with evi-
old man with Still's disease with bilateral hip and knee
dence of bonding according to criteria described by Engh et
replacements. He fell two years after his second THR and
al.10 Formation of new bone with a trabecular pattern was
sustained a mid-shaft fracture of the femur at the junction
seen in relation to all femoral components in all the Gruen
of the femoral components of the hip and knee replace-
zones except zone 7 (Fig. 1). In 11 hips at the level of the calcar
VOL. 91-B, No. 7, JULY 2009
12 / MBA Institute. Número 4. Mayo de 2013
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
N. N. SHAH, A. J. EDGE, D. W. CLARK
Table III. The cumulative survival table with revision of any acetabular component as the endpoint
Years since
Effective
Cumulative
number at risk
survival rate (%)
The long-term results of cemented THR in elderly and low-
demand patients can be excellent,15-17 but in young and
active patients they are variable, although some studies have
shown excellent results in this age group.18,19 The Furlong
HAC-coated femoral stem was introduced in 1985 with the
intention of obtaining a permanent bond between the
implant and host bone. This has been substantiated by
studies which have shown excellent long-term results in both
elderly and young patients, including revisions.5,20-23
The initial report on our series of young patients at a
mean follow-up of ten years found 100% survival for the
Time since operation (yrs)
femoral component.5 Extended follow-up of the same
group at a mean of 16 years has found no aseptic loosening
The cumulative survival curve with revision of any acetabular compo-
in any of these implants.
nent as the endpoint with the 95% confidence interval shown.
New bone grows into the HA coating on the prosthesis at
about the same rate as that of the healing of a fracture.24Living bone replaces the HA over time and in these circum-
in Gruen zone 7, an area of bone resorption with rounding of
stances new bone grows on to the titanium prosthesis with-
calcar was seen extending distally from 2 mm to 5 mm.
out an intervening layer of fibrous tissue.24 The HA-coated
Grade-I heterotopic ossification was observed in 16 hips
component forms a strong bond to the host bone, which is
and grade-II in two. Of these 18 THRs, eight had required
comparable to the strength of the cortical bone itself.25
revision of the acetabular component.
Radiographs show new trabeculae in the proximity of load-
Survivorship. There were no revisions or impending revi-
bearing areas of the femoral component indicating that new
sions because of aseptic loosening of the femoral compo-
bone is laid down where it is most needed. Relative
nent, giving a cumulative survival of the implant of 100%
osteopenia occurs in areas of stress shielding (Fig. 1). If the
at 16 years (95% CI 89 to 100) (Table II, Fig. 2). The cumu-
geometry of the implant allows new bone to grow into the
lative survival of all acetabular components was 77% at a
HA coating in this manner it will create a sealing effect and
follow-up of 16 years. The individual survivorship for
limit the migration of wear particles around the implant
cemented polyethylene components was 59% and for
thereby protecting osteolysis induced by these particles.
uncemented cancellous screw fixation components 86% at
The poor survivorship of the polyethylene acetabular
the same interval (Table III, Fig. 3).
components in our series may have been due to a variety of
THE JOURNAL OF BONE AND JOINT SURGERY
MBA Institute. Número 4. Mayo de 2013 / 13
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
HYDROXYAPATITE-CERAMIC-COATED FEMORAL COMPONENTS IN YOUNG PATIENTS FOLLOWED-UP FOR 16 TO 19 YEARS
factors such as an abducted position of the component, the
8. Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of
use of polyethylene which had to be sterilised in air and the
patients about total hip replacement. J Bone Joint Surg [Br] 1996;78-B:185-90.
use of heads of 32 mm diameter which is a known risk fac-
9. Amstutz HC, Thomas BJ, Jinnah R, et al. Treatment of primary osteoarthritis of
the hip: a comparison of total joint and surface replacement arthroplasty. J Bone
tor for polyethylene wear. Despite the fact that the HAC
Joint Surg [Am] 1984;66-A:228-41.
Furlong femoral components were exposed to the same
10. Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic
particle load associated with acetabular failure there was
fixation of porous-surfaced femoral components. Clin Orthop 1990;257:107-28.
no case of aseptic loosening and any bone loss was limited
11. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-
to Gruen zone 7 without compromising fixation. We
type femoral components: a radiographic analysis of loosening. Clin Orthop
observed bone loss of between 2 mm and 5 mm in 11
12. Goetz DD, Smith EJ, Harris WH. The prevalence of femoral osteolysis associated
patients just beneath the collar of the femoral component
with components inserted with or without cement in total hip replacements: a ret-
which we believe was due to stress shielding. We think that
rospective matched pair series. J Bone Joint Surg [Am] 1994;76-A:1121-9.
the collar of the Furlong stem helps to provide early
13. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip
replacement. Clin Orthop 1976;121:20-32.
mechanical stability until host bone has bonded to the HA
14. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification fol-
coating. The stress-shielding effect of the collar was never
lowing total hip replacement: incidence and a method of classification. J Bone
seen to produce progressive lysis.
Joint Surg [Am] 1973;55-A:1629-32.
Concerns have been expressed about the migration of
15. Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivor-
HA particles into the joint space resulting in third-body
ship of two thousand consecutive primary charnley total hip replacements: factors
affecting survivorship of acetabular and femoral components. J Bone Joint Surg
wear.26 Bauer et al27 compared the surface roughness of the
femoral head and polyethylene in HA- and porous-coated,
16. Callaghan JJ, Templeton JE, Liu SS, et al. Results of Charnley total hip arthro-
and cemented THRs. The HA hips had the best surface
plasty at a minimum of thirty years: a concise follow-up of a previous report. J Bone
Joint Surg [Am] 2004;86-A:690-5.
characteristics and they were unable to detect HA particles
17. Nercessian OA, Martin G, Joshi RP, Su BW, Eftekhar NS. A 15 to 25-year
follow-up study of primary Charnley low-friction arthroplasty: a single surgeon
In this series of young patients we did not see the crack
series. J Arthroplasty 2005;20:162-7.
microfracture phenomenon around any femoral component28
18. Joshi AB, Porter ML, Trail IA, et al. Long-term results of Charnley low-friction
and no patient reported pain in the anterior thigh. Such pain is
arthroplasty in young patients. J Bone Joint Surg [Br] 1993;75-B:616-23.
thought to occur in the presence of movement of the femoral
19. Kim YH, Kim JS, Yoon SH. Long-term survivorship of the Charnley Elite Plus fem-
oral component in young patients. J Bone Joint Surg [Br] 2007;89-B:449-54.
component and has been described with other implants with
20. Raman R, Kamath RP, Parikh A, Angus PD. Revision of cemented hip arthro-
an incidence of between 4% and 22%.10,29-31 The absence of
plasty using a hydroxyapatite-ceramic-coated femoral component. J Bone Joint
this problem in our series is probably due to the good initial
Surg [Br] 2005;87-B:1061-7.
mechanical stability provided by the geometry of the prosthe-
21. McNally SA, Shepperd JAN, Mann CV, Walzak JP. The results at nine to
sis until permanent fixation is provided by bone integration. It
twelve years of the use of a hydroxyapatite-coated femoral stem. J Bone Joint Surg
may also be related to the modulus of elasticity of the titanium
22. Shetty AA, Slack R, Tindall A, James KD, Rand C. Results of a hydroxyapatite
implant and to the bonding of the bone throughout its
coated (Furlong) total hip replacement: a 13 to 15 year follow-up. J Bone Joint Surg
At a mean follow-up of 16 years the Furlong HAC-
23. Rajaratnam SS, Jack C, Tavakkolizadeh A, et al. Long-term results of a
coated femoral component gives excellent fixation in young
hydroxyapatite-coated femoral component in total hip replacement: a 15- to 21-
year follow up study. J Bone Joint Surg [Br] 2008;90-B:27-30.
and active patients.
24. Geesink RGT, De Groot K, Klein CPAT. Bonding of bone to apatite coated
implants. J Bone Joint Surg [Br] 1988;70-B:17-22.
The authors wish to thank R. Knight for her help with the project and K. Grayson(Statistics by Design) for her help with the statistics.
25. Aebli N, Krebs D, Schwenke H, et al. Degradation of hydroxyapatite coating on
No benefits in any form have been received or will be received from a com-
a well-functioning femoral component. J Bone Joint Surg [Br] 2003;85-B:499-503.
mercial party related directly or indirectly to the subject of this article .
26. Morscher EW, Hefti A, Aebi U. Severe osteolysis after third-body wear due to
hydroxyapatite particles from acetabular cup coating. J Bone Joint Surg [Br]
27. Bauer TW, Taylor SK, Jiang M, Medendorp SBV. An indirect comparison of
1. Chandler HP, Reineck FT, Wixson RL, McCarthy JC. Total hip replacement in
third-body wear in retrieved hydroxyapatite-coated, porous, and cemented compo-
patients younger than thirty years old: five year follow up study. J Bone Joint Surg
nents. Clin Orthop 1994;298:11-18.
28. Edge AJ. Further opinion on: Long term results of a hydroxyapaptite-coated femo-
2. Don LD, Luckett M, Conaty JP. Total hip arthroplasties in patients younger than 45
ral component in total hip replacement: a 15- to 21-year study. www.jbjs.org.uk/
years: a nine to ten year follow-up study. Clin Orthop 1990;260:215-19.
cgi/content/full/90-B/1/27/DCI (date last accessed 1 May 2009).
3. Gustilo RB, Burnham WH. Long-term results of total hip arthroplasty in young
patients. Hip 1982;27-33.
29. Campbell ACL, Rorabeck CH, Bourne RB, Chess D, Nott L. Thigh pain after
cementless arthroplasty: annoyance or ill omen. J Bone Joint Surg [Br] 1992;74-
4. Rahbeck O, Overgaard S, Lind M, et al. Sealing effect of hydroxyapatite coating
on peri-implant migration of particles: an experimental study in dogs. J Bone Joint
Surg [Br] 2001;83-B:441-7.
30. Kim YH, Oh SH, Kim JS, Koo KH. Contemporary total hip arthroplasty with and
5. Singh S, Trikha SP, Edge AJ. Hydroxyapatite ceramic coated femoral stems in young
without cement in patients with osteonecrosis of the femoral head. J Bone Joint
patients: a prospective 10 year study. J Bone Joint Surg [Br] 2004;86-B:1118-23.
Surg [Am] 2003;85-A:675-81.
6. Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg [Br] 1982;64-
31. Kulkarni R, Rogers A, Downes EM. The ABG hydroxyapatite coated hip prosthe-
sis: 100 patients with a 3-8 year prospective follow up. J Bone Joint Surg [Br]
7. Harris H. Traumatic arthritis of the hip after dislocation and acetabular fractures:
treatment by mold arthroplasty: an end result study using a new method of result
32. Furlong RJ, Osborn JF. Fixation of hip prosthesis by hydroxyapatite ceramic coat-
evaluation. J Bone Joint Surg [Am] 1969;51-A:737-55.
ings. J Bone Joint Surg [Br] 1991;73-B:741-5.
VOL. 91-B, No. 7, JULY 2009
14 / MBA Institute. Número 4. Mayo de 2013
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
Resultados a largo
plazo de un vástago
femoral recubierto
de hidroxiapatita en
reemplazos totales de
cadera
Estudio con seguimientos de entre 15 y 21
años
Entre 1986 y 1991 implantamos de modo consecutivo
331 vástagos Furlong recubiertos de hidroxiapatita para
el reemplazo total de cadera de 291 pacientes. Se empleó
una prótesis acetabular cementada en 217 caderas y un
componente recubierto de hidroxiapatita en 114. Descri-
bimos la supervivencia a largo plazo tanto clínica como
radiológica del componente femoral con un seguimiento
medio de 17.5 años (15 a 21). Sólo dos pacientes (0.68%)
fueron perdidos durante el seguimiento. Tomando la re-
visión del componente femoral por cualquier causa como
el punto final, la supervivencia a una media de 17 años
fue del 97.4% (intervalo de confianza al 95% de 94.1 a
99.5), y tomando la revisión por aflojamiento aséptico
como punto final, ésta fue del 100%. La supervivencia
a un máximo de 21 años, tomando la revisión del com-
ponente femoral por cualquier motivo como punto final,
fue del 97.4% (intervalo de confianza al 95% de 81.0 a
99.5). Estos resultados superan a los mejores obtenidos a
largo plazo con componentes femorales cementados o no
cementados en el reemplazo total de cadera.
MBA Institute. Número 4. Mayo de 2013 / 15
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
Long-term results of a hydroxyapatite-coated
femoral component in total hip replacement
A 15- TO 21-YEAR FOLLOW-UP STUDY
S. S. Rajaratnam,
Between 1986 and 1991 we implanted 331 consecutive Furlong hydroxyapatite-coated
femoral components of a total hip replacement in 291 patients. A cemented acetabular
A. Tavakkolizadeh,
prosthesis was used in 217 hips and a hydroxyapatite-coated component in 114. We
M. D. George,
describe the long-term clinical and radiological survival of the femoral component at a
R. J. Fletcher,
mean follow-up of 17.5 years (15 to 21). Only two patients (0.68%) were lost to follow-up.
M. Hankins,
With revision of the femoral component for any reason as the endpoint, the survival at a
J. A. N. Shepperd
mean of 17 years was 97.4% (95% confidence interval 94.1 to 99.5), and with revision for
aseptic loosening as the endpoint it was 100%. The survival at a maximum of 21 years with
From Conquest
revision of the femoral component for any reason as the endpoint was 97.4% (95%
Hospital, St
confidence interval 81.0 or 99.5). These results compare favourably with the best long-term
Leonards-on-Sea,
results of cemented or uncemented femoral components used in total hip replacement.
� S. S. Rajaratnam, FRCS (Tr & Orth), BSc (Hons), Senior Hip &
The results of the titanium hydroxyapatite
and were allowed to bear weight fully immedi-
Knee Fellow Peninsula Orthopaedic
(HA)-coated Furlong hip replacement (Joint
ately after surgery.
Research Institute, 812
Replacement Instrumentation Ltd, London,
The patients were reviewed clinically and
Pittwater Road, Deewhy, Sydney, Australia.
United Kingdom) have previously been
radiologically at 6, 12, 26 and 52 weeks after
reported, showing survival of the femoral com-
operation and annually thereafter. Antero-
� C. Jack, MRCS, Specialist
ponent of 100% at ten years and of 99% at a
posterior radiographs of the pelvis and lateral
Queen Elizabeth Hospital,
mean of 13 years.2 We report the longest pro-
radiographs of the hips were taken and the
Woolwich, London SE18 4QH, UK.
spective series to date of an HA-coated femoral
Merle d'Aubigne and Postel hip score3 was used
� A. Tavakkolizadeh, FRCS (Tr & Ortho), MSc, Specialist
for the assessment of pain, mobility and func-
Kings College Hospital, Denmark
Patients and Methods
Hill, London SE5 9RS, UK.
The stability and fixation of the femoral
Between 1986 and 1991, in Hastings, United
component was assessed by two independent
� M. D. George, FRCS (Tr & Orth), Hip Fellow
Kingdom, we performed 331 total hip
observers (SSR, CJ) by a consensus of opinion.
Guy's Hospital, St Thomas' Street,
replacements (THRs) in 291 patients with a
The appearance of radiolucencies around the
London Bridge, SE1 9RT, UK.
mean age of 71.2 years (31.1 to 89.8). A total
component according to Gruen, McNiece and
� R. J. Fletcher, MRCS,
BSc(Hons), Research Registrar
of 40 patients had bilateral THRs, 30 under
Amstutz was noted, as was subsidence on
� J. A. N. Shepperd, FRCS,
one anaesthetic and ten in a staged procedure.
serial radiographs, the presence of increased
Consultant Orthopaedic SurgeonConquest Hospital, The Ridge, St
All the patients had a Furlong HA-coated
bone density suggesting bony ingrowth, and
Leonards-on-Sea, East Sussex
THR. The operation was performed via a
the appearance of radiolucent lines and pedes-
TN37 7RD, UK.
Watson-Jones approach by, or under the
tal formation at the tip of the stem. An assess-
� M. Hankins, BSc(Hons),
supervision of a consultant orthopaedic sur-
ment of the radiographs was also made for
FRSS, Senior Research Fellow/Statistician
geon (JANS).
evidence of stress shielding and of each Gruen
Brighton & Sussex Medical
A total of 217 THRs were undertaken using
zone for osteopenia.
School, Falmer BN1 9RH, UK.
a Furlong HA-coated femoral component and
Correspondence should be sent
to Mr S. S. Rajaratnam; e-mail:
a Furlong ultra-high-density-polyethylene
cemented acetabular component. The remain-
The patients were followed up for a mean of
2008 British Editorial Society
ing 114 THRs, operated on after 1 January
17.5 years (15 to 21). A total of 184 patients
of Bone and Joint Surgery
1990, had an HA-coated threaded acetabular
(63.2%; 211 hips) had died by the final follow-
doi:10.1302/0301-620X.90B1. 19731 $2.00
component (Joint Replacement Instrumenta-
up. All had been reviewed within one year of
tion Ltd) and a HA-coated Furlong femoral
their death and were therefore included in the
J Bone Joint Surg [Br]2008;90-B:27-30.
component. A 32 mm modular ceramic head
survival analysis.
Received 22 May 2007;
was used in all patients. Each patient had three
Of the remaining 107 patients with 120
Accepted after revision 29 August 2007
doses of prophylactic antibiotics (cefuroxime)
THRs, 15 failed to attend the final review and
VOL. 90-B, No. 1, JANUARY 2008
16 / MBA Institute. Número 4. Mayo de 2013

Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
S. S. RAJARATNAM, C. JACK, A. TAVAKKOLIZADEH, M. D. GEORGE, R. J. FLETCHER, M. HANKINS, J. A. N. SHEPPERD
Anteroposterior pelvic radiograph showing well-fixed bilateral Furlong
hydroxyapatite-coated femoral components and threaded acetabular
components, 17 years after total hip replacement.
Lateral radiograph of the hip showing a well-fixed Furlong hydroxy-
apatite-coated total hip replacement 17 years after operation.
were contacted via an extended telephone interview. Theirresults are included in the study. Two hips in two patients(0.68%) were lost to follow-up. One had moved abroad 2.5years after THR and could not be contacted. The other hada well functioning THR at six years post-operatively and
There were no cases of aseptic loosening of the femoral
refused further review.
component during the study period. In all cases, the fem-
Clinical and radiological. The mean Merle D'Aubigne and
oral component remained well-fixed with no measured
Postel3 score recorded for the 92 patients (105 hips) who
migration at the latest follow-up, with radiological evi-
attended the latest follow-up was 5.63 (3 to 6) for pain,
dence of bonding in the form of spot-weld formation2 into
5.42 (2 to 6) for mobility and 4.50 (0 to 6) for function.
the stem and a blastic reaction at its tip (Figs 1 and 2). Six
No patient reported anterior thigh pain at any review.
patients (1.8%) underwent revision of the femoral compo-
Slight rounding of the femoral calcar under the collar
nent for trauma, sepsis or trunion fretting, at which stage
was seen in 43 of 105 hips (41%).
their well-fixed femoral component was removed (Table I).
Table I. Details of the revisions of the femoral components
Time since THR* (yrs) Indication for revision
Traumatic loosening of both components following road
One-stage revision of femoral component
Late infection following road traffic accident
Two-stage revision of both components
Loosening of the acetabular component
One-stage revision
Two-stage revision of both components
Acetabular loosening leading to dissociation of ceramic head One-stage revision of femoral component
Two-stage revision of femoral component
Peri-prosthetic fracture and loosening
One-stage revision of femoral component
* THR, total hip replacement
THE JOURNAL OF BONE AND JOINT SURGERY
MBA Institute. Número 4. Mayo de 2013 / 17
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
LONG-TERM RESULTS OF A HYDROXYAPATITE-COATED FEMORAL COMPONENT IN TOTAL HIP REPLACEMENT
Table II. Cumulative survival of the 331 hips (including the six revisions)
Years since operation
Number of hips Failures
Withdrawn Number at risk
Cumulative survival (%)
* 95% CI, 95% confidence interval
Time since operation (yrs)
Time since operation (yrs)
Kaplan Meier survival curve (with 95% confidence intervals) with
Kaplan Meier survival curve (with 95% confidence intervals) showing
revision of the femoral component for any reason as the endpoint.
the worst case scenario. The two cases lost to follow-up have been
included as stem failures.
There were 30 revisions (9.1%) of the acetabular
cerclage wire was used to stabilise the fracture. All
component for infection (3 hips), dislocation (4 hips),
patients with iatrogenic proximal fractures of the femur
aseptic loosening (18 hips) and polyethylene wear
sustained during insertion of the stem went on to unite
satisfactorily, and did not suffer any long-term conse-
Per-operative fracture. There were 16 (4.8%) per-opera-
tive fractures, all of which were iatrogenic fractures of
Survival analysis. The life-table survival for the femoral
the anterior femoral cortex. In 15 hips (15 patients) a
component (including the six revisions) at a mean of
minor per-operative proximal fracture of the femur was
17 years was 97.4% (95% confidence interval (CI) 94.1
identified during implantation of the femoral compo-
to 99.5) and at a maximum of 21 years was 97.4% (95%
nent, as previously described.1 All patients with per-
CI 81.0 to 99.5) (Table II, Fig. 3). Figure 4 shows the
operative fractures identified during surgery were mobi-
worst case scenario, including the two patients lost to
lised non-weight-bearing for six weeks. In one patient, a
VOL. 90-B, No. 1, JANUARY 2008
18 / MBA Institute. Número 4. Mayo de 2013
S. S. RAJARATNAM, C. JACK, A. TAVAKKOLIZADEH, M. D. GEORGE, R. J. FLETCHER, M. HANKINS, J. A. N. SHEPPERD
component loads the entire femur surrounding it ade-
Previous studies on the Furlong HA-coated femoral compo-
quately. However, we accept that we have not performed
nent have shown excellent medium-term survival when
bone densitometry of the proximal femur to accurately
used as a primary1,2,5,6 or revision implant.6,7
quantify peri-prosthetic osteopenia.
Our current series includes the first 100 Furlong HA-
A total of 16 peri-operative fractures occurred in our
coated THRs which were previously reported at a mean of
series, 11 of which were seen in the first 100 THRs, as
ten years (9 to 12), with a 100% follow-up and a survival of
reported previously,1 and comprised iatrogenic fractures of
98.95% at up to 12 years, with no cases of aseptic loosen-
the anterior femoral cortex. The prevalence of these frac-
ing of the femoral stem.1
tures in the early stages of the study most likely represents
The Furlong HA-coated THR has also successfully been
the learning experience encountered with the use of any new
used in younger patients.5,6 Singh et al5 reported the suc-
implant. Of the 16 fractures, 15 were proximal cracks of the
cessful use of this implant in patients below the age of 50
anterior femoral cortex and did not require supplementary
years with a 100% survival of the femoral component at a
fixation. This type of fracture can be avoided by recognising
mean of ten years (5.3 to 14.2). Robertson et al6 had a
that adequate space needs to be cleared in the posterolateral
95.3% survival of the femoral component at a mean of 8.8
corner of the proximal femur to accommodate the relatively
years (5 to 13.8) in patients less than 55 years of age. They
bulky body of the implant. One fracture extended further
did not identify any cases of aseptic loosening of the femo-
distally and required cerclage wire fixation to stabilise the
ral component.
implant. Nevertheless, all fractures united satisfactorily and
The Furlong HA-coated THR has provided impressive
there were no further complications.
medium-term results as a revision implant.7,8 At a mean
Anterior thigh pain has been reported previously with
follow-up of eight years (5 to 12.4) Trikha et al7 reported
the use of uncemented hip prostheses.10,11 This was not the
survival of the femoral component of 100% with aseptic
case in our study. The absence of thigh pain in our study
loosening as the endpoint, while Raman et al8 found sim-
may be related to the modulus of elasticity of the titanium
ilarly good results with survival of 95.6% at a mean
implant and to the bonding of bone throughout its length as
follow-up of 12 years when revising cemented THRs.
shown in a retrieval analysis.12
In our series of 331 consecutive THRs, survival of the fem-
We would like to thank our research assistants Mrs. K. Goddard, Ms K. Miles
oral component at a mean of 17 years was 97.4% (95% CI
and Mrs. D. East for their invaluable efforts over the last 20 years in making this
94.1 to 99.5) and at a maximum of 21 years was 97.4% (95%
prospective study possible.
No benefits in any form have been received or will be received from a com-
CI 81.0 to 99.5), with revision for any reason as the endpoint.
mercial party related directly or indirectly to the subject of this article.
With aseptic loosening of the femoral component as the end-point, the survival would be 100%. These figures are similar to
those in the literature for the same femoral component.1,2,5-8
1. McNally SA, Shepperd JAN, Mann CV, Walzac JP. The results at nine to twelve
The length of follow-up achieved in this study is largely
years of the use of a hydroxyapatite-coated femoral stem. J Bone Joint Surg [Br]
attributable to the static elderly population of our region.
2. Shetty AA, Slack R, Tindall A, James KD, Rand C. Results of a hydroxyapatite
Only two of the 331 THRs were unaccounted for, thereby
coated (Furlong) total hip replacement: a 13-15 year follow-up. J Bone Joint Surg [Br]
reducing the errors in the survival analysis highlighted by
3. Merle d'Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic
Murray, Britton and Bulstrode.9
prosthesis. J Bone Joint Surg [Am] 1954;36-A:451-75.
The Merle D'Aubigne and Postel hip scoring system3 for the
4. Gruen TA, McNiece GM, Amstutz HC. "Modes of failure" of cemented stem-type
assessment of pain, mobility and function has been used since
femoral components: a radiographic analysis of loosening. Clin Orthop 1979;141:17-
the commencement of this study. However, the mobility and
5. Singh S, Trikha SP, Edge AJ. Hydroxyapatite ceramic-coated femoral stems in
function scores achieved at the latest follow-up were influ-
young patients: a prospective 10 year study. J Bone Joint Surg [Br] 2004;86-B:1118-
enced by the advancing age of the patients as the follow-up
extended. This explains the good mean scores of 5.63 for pain
6. Robertson A, Lavalette D, Morgan S, Angus PD. The hydroxyapatite coated JRI-
Furlong hip: outcome in patients under the age of 55 years. J Bone Joint Surg [Br]
and 5.42 for mobility, but the relatively modest score of 4.50
for function.
7. Trikha SP, Singh S, Raynham OW, et al. Hydroxyapatite ceramic coated femoral
The collar on the femoral component prevents early subsid-
stems in revision hip surgery. J Bone Joint Surg [Br] 2005;87-B:1055-60.
ence of the prosthesis after implantation. Once bone has
8. Raman R, Kamath RP, Parikh A, Angus PD. Revision of cemented hip arthroplasty
using a hydroxyapatite-ceramic-coated femoral component. J Bone Joint Surg [Br]
bonded to the prosthesis, its function becomes redundant.
This may account for the rounding of the bone under the fem-
9. Murray DW, Britton AR, Bulstrode C. Loss to follow-up matters. J Bone Joint Surg
oral collar seen on the radiographs at the final follow-up.
10. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors
Stress protection osteopenia occurs when a distally well-
governing bone ingrowth, stress shielding and clinical results. J Bone Joint Surg [Br]
fixed femoral component takes the load in preference to the
proximal femur. From the plain radiographs we were
11. Engh CA, Massin P. Cementless total hip arthroplasty using the anatomic medullary
locking stem: results using a survivorship analysis. Clin Orthop 1989;249:141-56.
unable to identify any consistent pattern of osteopenia in
12. Furlong RJ, Osborn JF. Fixation of hip prosthesis by hydroxyapatite ceramic coat-
our series and believe that the Furlong HA-coated femoral
ings. J Bone Joint Surg [Br] 1991;73-B:741-5.
THE JOURNAL OF BONE AND JOINT SURGERY
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
Resultados de un
reemplazo total de
cadera recubierto de
hidroxiapatita (Furlong)
Seguimiento de entre 13 y 15 años
Describimos la supervivencia de 134 reemplazos totales
de cadera JRI Furlong recubiertos de hidroxiapatita im-
plantados de modo consecutivo. El seguimiento medio
fue de 14.2 años (13 a 15).
Los pacientes fueron valorados clínicamente utilizando
la escala de Merle d'Aubigne y Postel. Las radiografías
fueron evaluadas usando las zonas de Gruen para el vás-
tago y las zonas de DeLee y Charnley para el acetábulo.
Signos de movilización, líneas de radiotransparencia,
formación de hueso endóstico (soldadura por puntos) y
formación en pedestal fuero usados para evaluar la fija-
ción y la estabilidad del vástago de acuerdo con los cri-
terios de Engh. El ángulo del cotilo, migración y radio-
transparencia fueron usados para evaluar el aflojamiento
del acetábulo. El criterio para el fallo fue la revisión o
una necesidad de la misma debido a dolor o aflojamiento.
El análisis de supervivencia fue realizado utilizando una
tabla vital y la curva de Kaplan-Meier.
La media total de la escala Merle d'Aubigne y Postel fue
de 7.4 antes de la cirugía y de 15.9 durante el seguimien-
to. Durante el período de estudio 22 pacientes fallecieron
y 6 fueron perdidos para el seguimiento. Ninguno de los
acetábulos fue revisado. Un vástago fue revisado por una
fractura periprotésica tras caída, pero ninguna fue revisa-
da por aflojamiento, arrojando una tasa de supervivencia
del 99% a 13 años. Nuestras observaciones sugieren que
los resultados a largo plazo de estas prótesis recubiertas
con hidroxiapatita son más que satisfactorios.
20 / MBA Institute. Número 4. Mayo de 2013
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
Results of a hydroxyapatite-coated (Furlong)
total hip replacement
A 13- TO 15-YEAR FOLLOW-UP
A. A. Shetty,
We describe the survival of 134 consecutive JRI Furlong hydroxyapatite-coated
R. Slack,
uncemented total hip replacements. The mean follow-up was for 14.2 years (13 to 15).
A. Tindall,
Patients were assessed clinically, using the Merle d'Aubigné and Postel score.
K. D. James,
Radiographs were evaluated using Gruen zones for the stem and DeLee and Charnley zones
for the cup. Signs of subsidence, radiolucent lines, endosteal bone formation (spot welds)
and pedestal formation were used to assess fixation and stability of the stem according to
From Medway
Engh's criteria. Cup angle, migration and radiolucency were used to assess loosening of the
Maritime Hospital,
cup. The criteria for failure were revision, or impending revision because of pain or
Kent, England
loosening. Survival analysis was performed using a life table and the Kaplan-Meier curve.
The mean total Merle d'Aubigné and Postel score was 7.4 pre-operatively and 15.9 at
follow-up. During the study period 22 patients died and six were lost to follow-up. None of
the cups was revised. One stem was revised for a periprosthetic fracture following a fall but
� A. A. Shetty, MCh, FRCS,
none was revised for loosening, giving a 99% survival at 13 years. Our findings suggest that
FRCS(Orth), Senior Fellow in Orthopaedics
the long-term results of these hydroxyapatite-coated prostheses are more than
King's College Hospital,
Denmark Hill, London SE5 9RS, UK.
� R. Slack, MRCS, FRCS(Orth), Specialist
Previous studies have reported a 100% ten-
Table I. Pre-operative diagnoses
Registrar in Orthopaedics
year survival for the JRI Furlong (Joint
William Harvey Hospital,
Number of hips
Ashford, Kent TN24 0LZ, UK.
Replacement Instrumentation Ltd, London,
UK) hydroxyapatite (HA)-coated femoral
� A. Tindall, MRCS,
Specialist Registrar in
prosthesis.1 Although the theoretical advan-
Avascular necrosis
Guy's Hospital, St Thomas'
tages of an uncemented prosthesis, especially
Street, London SE1 9RT, UK.
in the younger patient, are becoming more
� K. D. James, BSc, MBBS,
established, little long-term data exist on their
Rheumatoid arthritis
Orthopaedic Senior House
use in practice. We present a prospective study
* dysplasia (four hips), slipped upper femoral epi-
Medway Maritime Hospital,
of the HA-coated uncemented JRI Furlong
Gillingham, Kent ME7 5NY,
femoral component.
� C. Rand, FRCS,
Patients and Methods
Table II. Pre-operative Charnley category3 for the 116
FRCS(Orth), Consultant
Orthopaedic Surgeon
All patients who required a primary total hip
Princess Royal University
Number of
Hospital, Farnborough
replacement under the care of one surgeon
Common, Orpington, Kent
(CR) between November 1989 and December
Class A, unilateral hip disease only
BR6 8ND, UK.
1991 were entered into the study. There were
Class B, bilateral hip disease only
Correspondence should be
no exclusion criteria. This longitudinal cohort
Class C, multiple orthopaedic and/or
sent to Mr A. A. Shetty at 6
Barncroft Drive, Hempstead,
of 116 consecutive patients (134 hips) was fol-
Gillingham, Kent ME7 3TJ,
lowed up prospectively. The mean age of
UK; e-mail: [email protected]
patients was 75 years (26 to 95) with 88women and 28 men; 66 hips were right-sided,
(Watson-Jones) approach. All had a fully HA-
2005 British Editorial Society of Bone and
32 were left-sided and 36 were bilateral (ten
coated JRI stem and either a 28-mm cobalt-
simultaneous, eight consecutive). The indica-
chrome or ceramic head. The acetabular com-
doi:10.1302/0301-620X.87B8. 16011 $2.00
tions for surgery and the pre-operative Charn-
ponent was either an HA-coated threaded or a
ley functional categories3 are shown in Tables I
surface fixation cup (JRI Ltd, London, UK)
J Bone Joint Surg [Br] 2005;87-B:1050-4.
(Table III). The change to a surface fixation cup
Received 23 September
The patients were operated upon by the
during the study was a result of it being readily
2004; Accepted after revision 14 December 2004
same surgeon (CR) through an anterolateral
available and, for the surgeon, technically sim-
THE JOURNAL OF BONE AND JOINT SURGERY
MBA Institute. Número 4. Mayo de 2013 / 21
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
RESULTS OF A HYDROXYAPATITE-COATED (FURLONG) TOTAL HIP REPLACEMENT
Table III. Details of the implants used
quently recalled for clinical and radiological review for thisstudy. The mean follow-up was 14.2 years (13 to 15).
Number of hips
Clinical assessment was performed using Charnley's
modification of the Merle d'Aubigné and Postel scores.4 In
Surface fixation cup
addition to overall pain, range of movement and walking
score, we specifically asked about thigh pain.
Standardised anteroposterior (AP) and lateral radio-
graphs were used for radiological assessment. The AP pro-
* all cups had a polyethylene insert† femoral heads were all 28 mm in size and all fem-
jection was based on the symphysis pubis and was taken at
oral stems were fully hydroxyapatite-coated
a standard distance of 1 m. The post-operative radiographswere assessed by Gruen zones5 for the femoral componentand DeLee and Charnley6 zones for the acetabular compo-
pler to use. Ten patients also had a femoral head autograft
for acetabular deficiency. Immediate weight-bearing was
The fixation and stability of the stem were assessed using
encouraged post-operatively and all patients received rou-
Engh's radiological score for uncemented prostheses.7 This
tine antibiotic and deep-vein thrombosis prophylaxis.
has two scales, fixation (maximum ten points) and stability
The patients were assessed pre-operatively and at six
(maximum 17 points). The higher the score, the better the
weeks, three months, one, two and five years, and subse-
fixation and stability. The degree of subsidence was also
Annotated radiograph showing the reference line used
to measure subsidence and the Gruen zones5 with the
incidence of endosteal bone formation (EBF) or spot
welds and reactive lines (RL).
VOL. 87-B, No. 8, AUGUST 2005
22 / MBA Institute. Número 4. Mayo de 2013
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
RESULTS OF A HYDROXYAPATITE-COATED (FURLONG) TOTAL HIP REPLACEMENT
A. A. SHETTY, R. SLACK, A. TINDALL, K. D. JAMES, C. RAND
Table III. Details of the implants used
quently recalled for clinical and radiological review for this
DeLee and Charnley zones
study. The mean follow-up was 14.2 years (13 to 15).
Number of hips
Clinical assessment was performed using Charnley's
modification of the Merle d'Aubigné and Postel scores. In
Surface fixation cup
addition to overall pain, range of movement and walking
score, we specifically asked about thigh pain.
Standardised anteroposterior (AP) and lateral radio-
graphs were used for radiological assessment. The AP pro-
* all cups had a polyethylene insert
† femoral heads were all 28 mm in size and all fem-
jection was based on the symphysis pubis and was taken at
oral stems were fully hydroxyapatite-coated
a standard distance of 1 m. The post-operative radiographswere assessed by Gruen zones5 for the femoral componentand DeLee and Charnley6 zones for the acetabular compo-
pler to use. Ten patients also had a femoral head autograft
Interteardrop line
for acetabular deficiency. Immediate weight-bearing was
The fixation and stability of the stem were assessed using
encouraged post-operatively and all patients received rou-
Engh's radiological score for uncemented prostheses.7 This
tine antibiotic and deep-vein thrombosis prophylaxis.
has two scales, fixation (maximum ten points) and stability
The patients were assessed pre-operatively and at six
(maximum 17 points). The higher the score, the better the
weeks, three months, one, two and five years, and subse-
fixation and stability. The degree of subsidence was also
Annotated radiograph to show the reference lines used to measure cup angle and migration. DeLee and Charnley zones are
marked to show the percentage of endosteal bone formation (EBF) and reactive lines (RL).
measured by changes in the vertical distance between the
Gruen or DeLee and Charnley zone.6 The formation of
Annotated radiograph showing the reference line used
tip of the greater trochanter and the most proximal point
heterotopic ossification was graded according to the
to measure subsidence and the Gruen zones5 with the
on the implant; a change of more than 2 mm was consid-
method described by Brooker et al.9
incidence of endosteal bone formation (EBF) or spot
welds and reactive lines (RL).
ered to be evidence of subsidence (Fig. 1). Spot welds were
The criteria for failure were either revision or an impend-
defined as the presence of new bone formation bridging the
ing revision because of pain or loosening.
gap between the endosteal surface and the surface of the
implant. A bone pedestal was defined as a shelf of endosteal
new bone, either partially or completely bridging the
During the study period 22 patients died and six were lost
intramedullary canal, at the tip of the implant. Calcar
to follow-up.
remodelling was recorded as hypertrophic, atrophic or
The Merle d'Aubigné and Postel scores improved for all
patients, except one who developed Brooker grade IV
Migration of the acetabular component was defined as
heterotopic ossification. The mean total score rose from 7.4
significant if there was a > 3 mm linear change (medial,
(SD 1.5) at pre-operative assessment to 15.9 (SD 1.8) at fol-
superior or both) in relation to either Kohler's or the inter-
low-up with each component of the score showing an
teardrop line.8 Rotational change was regarded as signifi-
improvement (Table IV). No patient complained of thigh
cant if there was a change of > 3˚ in the angle of the
acetabular component (Fig. 2).
The mean Engh score for fixation and stability was 24.7
Radiolucent and sclerotic lines at the acetabular and fem-
(10 for fixation and 14.7 for stability). In 109 stems (81%)
oral interfaces were also measured. A significant reactive
there was a pedestal at its tip (Fig. 3). The development of
line was classified as a lucency at the bone-implant interface
endosteal bone formation in the form of spot welds is
if it was 2 mm wide and occupied at least 50% of any one
shown in Figure 1. There were no reactive lines at the bone-
VOL. 87-B, No. 8, AUGUST 2005
THE JOURNAL OF BONE AND JOINT SURGERY
MBA Institute. Número 4. Mayo de 2013 / 23
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
RESULTS OF A HYDROXYAPATITE-COATED (FURLONG) TOTAL HIP REPLACEMENT
Table IV. Merle d'Aubigné and Postel clinical scores4*
component. There was no migration in either a vertical or ahorizontal direction and no change in cup angle.
Complications. There were two deep-vein thromboses, one
of which progressed to a fatal pulmonary embolus. There
were also two transient femoral nerve palsies and one tran-
sient common peroneal nerve palsy. There was one late
* maximum score is 18 (6 for each category)
deep infection with a persistent sinus and one femoral stemrevision for fracture after significant trauma. Five patientshad Brooker grades III and IV heterotopic ossification
Table V. Post-operative complications
Number of cases
Survival analysis. In constructing a survival analysis, we
did not assume that the six patients who were lost to fol-
low-up had similar results to those who were contactable.
Pulmonary embolism
Deep-vein thrombosis
Evidence suggests that the former group of patients may
have worse outcomes than the latter.10 None of the 22
patients (27 hips) who died during the study period were
Deep (with sinus)
revised or were awaiting revision. At their last review, two
to six years after surgery, all hips were well fixed and func-
Common peroneal†
tioning well. We therefore constructed a life table (Fig. 4)
using best and worse case scenarios to account for those
Femur - minor (anterior/posterior cortex)
patients who were lost to follow-up.11-14
Acetabulum (posterior wall)
Our series shows a survival rate of 99% at 13 years (95%
confidence interval 94 to 100), equal to other published
series of HA-coated femoral components1,15 and superior
to other cementless implants.16,17 This is also the case when
using our worst case scenario, accounting for patients who
† common peroneal palsy followed a deep-vein thrombosis
were lost to follow-up.11
Clinical results were very satisfactory with excellent
improvement in the patients' Merle d'Aubigné and Postel
stem interface, no changes at the interface and no subsid-
scores. Deterioration in this score was seen in only one
ence or osteolysis in any of the radiographs studied.
patient with unknown ankylosing spondylitis and who
With regard to the acetabular component, there was
developed Brooker grade IV heterotopic ossification.
endosteal bone formation in DeLee and Charnley zones 1
Another significant feature of our study was the absence of
and 3 in all hips and in and zone 2 in 112 hips (84%,
thigh pain, in contrast with reports of other cementless fem-
Fig. 2). No reactive lines were seen in any zone, for any
oral components without HA-coating.17,18
Radiographs showing a) spot weld and b) pedestal for-
mation around the femoral stem.
VOL. 87-B, No. 8, AUGUST 2005
24 / MBA Institute. Número 4. Mayo de 2013
Resultados clínicos a largo plazo de la prótesis total de cadera Furlong H.A.C
A. A. SHETTY, R. SLACK, A. TINDALL, K. D. JAMES, C. RAND
Cumulative survival (%)
Cumulative survival (%)
Survival curves showing the a) best and b) worst-case scenarios.
The mean Engh's radiological score in our series was
2. Theis JC, Ball C. Medium-term results of cementless hydroxyapatite-coated pri-
24.7, representing excellent stability and fixation, with the
mary total hip arthroplasty: a clinical and radiological review. J Orthop Surg (Hong
presence of spot welds and absence of radiolucent lines.
3. Charnley J. The long term results of low friction arthroplasty of the hip performed as
Engh described satisfactory bony ongrowth as a total score
a primary intervention. J Bone Joint Surg [Br] 1972;54-B:61-76.
of ten points or more.7,19,20 Calcar atrophy, a positive sign
4. Merle d'Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic
of stability,7 was noted in our study and in that by Engh
prosthesis. J Bone Joint Surg [Am] 1954;36-A:451-75.
5. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type
early in the follow-up and was found to be non-progressive.
femoral components: a radiographic analysis of loosening. Clin Orthop 1979;141:
Radiological changes around the acetabular components
showed evidence of bony ongrowth with no signs of sec-
6. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip
replacement. Clin Orthop 1976;121:20-32.
ondary or impending loosening. Gap healing and remodel-
7. Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fix-
ling of cysts around the acetabulum was also seen. For the
ation of porous-surfaced femoral components. Clin Orthop 1990;257:107-28.
ten patients who received a femoral head autograft for ace-
8. Nunn D, Freeman MAR, Hill PF, Evans SJ. The measurement of migration of the
acetabular component of hip prostheses. J Bone Joint Surg [Br] 1989;71-B:629-31.
tabular deficiency, all showed incorporation of the graft, as
9. Brooker AF, Bowerman JW, Robinson RA, Riler LH Jr. Ectopic ossification fol-
demonstrated by trabecular re-orientation without evi-
lowing total hip replacement: incidence and method of classification. J Bone Joint
dence of significant graft resorption.21
Surg [Am] 1973;55-A:1629-32.
In our series there was no specific complication related to
10. Murray DW, Britton AR, Bulstrode C. Loss to follow-up matters. J Bone Joint Surg
the implant fixation by HA-coating. The incidence of intra-
11. Murray DW, Carr AJ, Bulstrode C. Survival analysis of joint replacements. J Bone
operative fractures seemed to be related to the experience of
Joint Surg [Br] 1993;75-B:697-704.
the surgeon in using this prosthesis. All the fractures were
12. Carr AJ, Morris RW, Murray DW, Pynsent PB. Survival analysis in joint replace-
ment surgery. J Bone Joint Surg [Br] 1993;75-B:178-82.
managed conservatively and united uneventfully without
13. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am
any long-term effect on the stability, fixation, or clinical
Stat Assoc 1958;53:457-81.
outcome. HA-coating may even have improved the chance
14. Murray DW, Carr AJ, Bulstrode CJ. Which primary total hip replacement? J Bone
of fracture union. One patient, who had a deep infection
Joint Surg [Br] 1995;77-B:520-7.
with a persistent sinus, surprisingly did not show any evi-
15. Skinner JA, Kroon PO, Todo S, Scott G. Femoral component with proximal HA
coating: an analysis of survival and fixation at up to 10 years. J Bone Joint Surg [Br]
dence of stem loosening. Our incidence of heterotopic ossi-
fication was comparable with other reported series.9,22,23
16. Donnelly WJ, Kobayashi A, Freeman MAR, et al. Radiological and survival com-
parison of four types of fixation of a proximal femoral stem. J Bone Joint Surg [Br]
The only prosthetic failure in our series was one peripros-
thetic femoral fracture. However, during the revision it was
17. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors
noted that the stem was well fixed.24
governing bone ingrowth, stress shielding and clinical results. J Bone Joint Surg [Br]
Our study shows a 99% survivorship at 13 to 15 years'
18. Engh CA, Massin P. Cementless total hip arthroplasty using the anatomic medullary
follow-up for total hip arthroplasty using these compo-
locking stem: results using a survivorship analysis. Clin Orthop 1989;249:141-56.
nents, adding long-term evidence to earlier, published
19. Geesink RGT, De Groot K, Klein C. Bonding of bone to apatite coated implants.
J Bone Joint Surg [Br] 1988;70-B:17-22.
series.1,2,15,18 HA-coating of implants appears to offer a sat-
20. Furlong RJ, Osborn JF. Fixation of hip prostheses by hydroxyapatite-ceramic coat-
isfactory solution to fixation. However, a valid concern
ings. J Bone Joint Surg [Br] 1991;73-B:741-5.
may be later failure as a consequence of polyethylene wear.
21. Gerber SD, Harris WH. Femoral head autografting to augment acetabular defi-
ciency in patients requiring total hip replacement: a minimum five-year and an aver-
No benefits in any form have been received or will be received from a commer-
age seven-year follow-up study. J Bone Joint Surg [Am] 1986;68-A:1241-8.
cial party related directly or indirectly to the subject of this article.
22. Ahrengart L. Periarticular heterotopic ossification after total hip arthroplasty: risk
factors and consequence. Clin Orthop 1991;263:49-58.
23. Kasetti RJ, Shetty AA, Rand C. Heterotrophic ossification after uncemented
1. McNally SA, Shepperd JAN, Mann CV, Walczak JP. The results at nine to
hydroxyapatite coated primary total hip arthroplasty. J Arthroplasty 2001;16:1038-42.
twelve years of the use of a hydroxyapatite-coated femoral stem. J Bone Joint Surg
24. Lewallen DG, Berry DJ. Periprosthetic fracture femur after total hip arthroplasty:
treatment and results to date. J Bone Joint Surg [Am] 1997;79-A:1881-90.
THE JOURNAL OF BONE AND JOINT SURGERY
MBA Institute. Número 4. Mayo de 2013 / 25
Y PRODUCIDO POR MBA.
.1 12MK075 DISEÑADO
Avda. Jardín Botánico 1345. Silos del Intra
33203 Gijón. España
T: +34 985 195 505 F: +34 985 373 452
Source: http://www.mbainstitute.eu/recursos/boletines/12mk075-boletin-mba-institute-04.pdf
ARTICLE IN PRESS Journal of Pharmaceutical and Biomedical Analysis xxx (2010) xxx–xxx Contents lists available at Journal of Pharmaceutical and Biomedical Analysis Short communication Determination of metformin in mouse, rat, dog and human plasma samples bylaser diode thermal desorption/atmospheric pressure chemical ionizationtandem mass spectrometry John G. Swales , Richard Gallagher, Raimund M. Peter
Information for Healthcare Professionals NAME OF THE MEDICINAL PRODUCT Haldol-Janssen solution for injection 5 mg/mL QUALITATIVE AND QUANTITATIVE COMPOSITION 1 mL solution for injection contains 5 mg haloperidol. For a full list of excipients, see section 6.1. PHARMACEUTICAL FORM Solution for injection Clear, colourless solution.