Certified registered nurse anesthetist burnout related to moral distress: a replication study
Southern California CSU DNP Consortium
California State University, Fullerton
California State University, Long Beach
California State University, Los Angeles
POST BURN PRURITUS RELIEF PROTOCOL
A DOCTORAL PROJECT
Submitted in Partial Fulfillment of the Requirements
For the degree of
DOCTOR OF NURSING PRACTICE
Doctoral Project Committee Approval:
Gail Washington, DNS, RN, PHN, Project Chair
Ayman Khalil Tailakh, PhD, RN, Committee Member
Copyright Yeon Sook Kim 2015
Post burn pruritus is pervasive, occurring in over 90% of burn patients. Moreover,
post burn pruritus continues in greater than 40% of patients for years even after burn
wounds are healed. Post burn pruritus is a syndrome of stressful symptoms experienced
by burn survivors that requires medical management with effective interventions.
Unfortunately, many burn patients suffer from pruritus-related post burn injury regardless
of current standard therapies. Therefore, in this Doctor of Nursing Practice project,
published evidence including studies/reviews of post burn pruritus relief served as a basis
for development of an advanced practice nurse (APN)-driven post burn pruritus relief
protocol. A systematic review was conducted and relevant empiric articles from
September 1, 2013 to November 17, 2014 were critically appraised. Initially, 79 articles
were found; 38 articles were selected using pre-established inclusion criteria. Two
frameworks were used to guide this project. The Preferred Reporting Items for
Systematic Reviews and Meta-Analyses (PRISMA) model was applied for the literature
review and the Rosswurm and Larrabee's model for evidence-based practice change was
used for clinical application. The newly developed APN driven post burn pruritus
protocol is driven by burn healing phase (pre-healing, healing, post-healing), and
emphasizes non-pharmacological interventions; it includes both non-pharmacological and
pharmacological methods specifically intended for reducing burn associated pruritus.
TABLE OF CONTENTS
ABSTRACT . iii LIST OF TABLES . vi LIST OF FIGURES . vii ACKNOWLEDGMENTS . viii BACKGROUND .
Problem Statement .
Purpose Statement.
Supporting Framework .
REVIEW OF LITERATURE .
Pharmacological Topical Interventions .
Non-pharmacological Interventions . 14
Summary of Literature Review. 18
PRISMA Model . 20
The Model for Evidence-based Practice Change . 21
Search Strategy . 23
Data Extraction and Quality Assessment. 24
Eligibility Criteria . 24
Study Selection and Data Collection process . 24
PROJECT MANUSCRIPT . 35 DISCUSSION . 40 REFERENCES . 41
APPENDIX A: 5 – D ITCH SCALE . 49
APPENDIX B: VISUAL ANALOGUE SCALE . 50 APPENDIX C: ITCH MAN SCALE . 51 APPENDIX D: TABLE OF EVIDENCE FOR PROPOSAL . 52
1. Characteristics of Included Studies.
2. Post Burn Pruritus Relief Protocol guideline .
1. PRISMA 2009 flow diagram .
2. A model of evidence-based practice change .
3. Flow diagram for selection of studies .
4. Post burn pruritus relief protocol .
It is I gratefully acknowledge the absolute and unwavering support of my family,
especially, my husband Harrison and my autistic son, Joon. Also, I truly appreciate the
expertise of Dr. Mathew Reiss at Torrance Memorial Medical Center.
BACKGROUND
In 1992, a Burn Nursing Delphi study classified pruritus as one of the highest
priority areas in nursing research. However, there has been a lack of research examining
the etiology and treatment of this highly distressing symptom (Goutos, 2010). Multiple
studies (Carrougher et al., 2013; Goutos, Clarke, Upson, Richardson, & Ghosh, 2010;
Goutos, Dziewulski, & Richardson, 2009) have examined post burn pruritus or itching
and have varying findings. Each study, however, has consistently demonstrated a
considerable level of pruritus in post burn populations. Casaer, Kums, Wouters, Van den
Kerckhove and Van den Berghe (2008) reported that 49% of patients, even with small
burn injury, experienced pruritus. Post burn pruritus can be defined as a severe itching
sensation as a result of burn injury. Pruritus has been identified as one of the most
general debilitating and stressful symptoms that post burn survivors experience (Bell &
Gabriel, 2009; Goutos, 2010; Goutos, Dziewulski, & Richardson, 2009).
The prevalence of post burn pruritus is seen in over 90% of burn patients and can
persist in greater than 40% of those patients for 4 to 10 years after burn injury
(Carrougher et al., 2013). According to Brooks et al. (2008), among patients with four
years after burn injury, 79% reported intermittent problems with pruritus while 29% of
patients reported persistent itching. However, twelve years after injury, these numbers
decreased to 44% and 5%, respectively.
According to Carrougher et al. (2013), itching prevalence is highly correlated
with females, young age, large burn areas, more grafted areas, dry skin, and raised or
thick scars. Casaer et al. (2008) more precisely reported that patients experienced more
pruritus between the ages of 2 to 50 years old; if the burn area was large; and, the area of
burn injury was on the trunk rather than the extremities. On the other hand, a study by
Thompson et al. (2013) found no significant differences between age and gender
regarding hypertrophic scars and pruritus. Thompson et al. (2013) reported burn size
over 20% of total body surface area (TBSA) had increased risk of itching. Yang et al.
(2014) found that patients with post burn pruritus had broader burned areas and more
severe scars. According to Goutos et al. (2009), burn patients tend to have significant
amount of itching within 1 month after burn injury with the highest at 6 months and a
decline over the first year after the injury. They reported that the origin of a burn can
affect associated pruritus. For example, scald injuries were most likely to provoke
pruritus, followed by flame and contact injuries (Goutos et al., 2009). The reason for
different findings from different studies was each study had different population
characteristics regarding TBSA, ages, gender, and burn areas. However, larger size of
burns are obviously more associated with post burn pruritus according to these studies
(Carrougher et al., 2013; Casaer et al., 2008; Thompson et al., 2013).
Post burn pruritus negatively impacts the quality of life in patients that included;
sleep disturbances, decreased enjoyment with leisure activities, decreased ability to
complete activities of daily living, and decreased school and work performance (Hettrick
et al.,2004). In addition, about 60% of burn patients experienced difficulty falling asleep
(Carrougher et al., 2013). According to Casaer et al. (2008), burn patients' daily life was
impacted in 42% of those suffering from moderate pruritus and 92% of those suffering
from severe pruritus. Parnell, Nedelec, Rachelska and LaSalle (2012) reported that
pruritus was related to low concentration, agitation, anxiety, and flat mood. In general,
researchers reported that pruritus triggered negative quality of life associated with
dryness, heat, sweat, activity, stress, fatigue, physical effort, and special fabric.
The problem of pruritus in post burn patients is well recognized. There are many
potential treatments available for itching (Bell & Gabriel, 2009). However, none of the
current standard therapies have been very effective (Otene & Onumaegbu, 2013). In
addition, there is currently no accord on standardized treatment of post burn pruritus
(Otene & Onumaegbu, 2013; Richardson, Upton & Rippon, 2014). Most often, therapies
include pharmacological interventions that include a selective histamine receptor
antagonist, but it is effective in only about 20% of patients (Brooks, Malic, & Judkins,
2008). This is because histamine is not the only element involved in the mechanism of
itching, but also there are non-histamine dependent pathways involved in the pruritus
mechanism according to the study by Schmelz (as cited in Brooks et al., 2008). Another
treatment is emollients which also have limited usage. For example, a eutectic mixture of
local anesthetic (EMLA) cream can be applied only to healed skin and the maximum
zone treated is 600 cm2 for patients less than 19 kg and 2000 cm2 for patients greater than
20 kg (Brooks et al., 2008). This lack of effective care is further compounded by the
absence of a standardized protocol. The Burn Nursing Delphi study (1992) identified the
need for high impact potential antipruritic strategies to improve patient care (Goutos et
Problem Statement
Post burn pruritus has been identified as one of the most general and stressful
symptoms that burn survivors experience and should be aggressively managed (Bell &
Gabriel, 2009; Goutos, 2010; Goutos, Dziewulski, & Richardson, 2009). Pruritus from
post burn injury begins in the early stages of wound healing. Pruritus is usually
prominent in patients who have second degree burns, but patients who experience third
degree burns may also have partly second degree burns. Pruritus comes along with
wound healing in the first two weeks after burn injury (Bell & Gabriel, 2009).
Consistently research findings have strongly proposed that post burn pruritus
management should be one of the top priorities for burn research (Bell & Gabriel, 2009;
Brooks, Malic, & Judkins, 2008). Itching from associated burn injury that persists over a
period of time leads to disabling symptoms such as sleep disturbance, anxiety, and
interruption of daily activities (Goutos et al., 2009).
Purpose Statement
The purpose of this project was to develop an advanced practice nurse (APN)
driven post burn pruritus relief protocol that include pharmacological and non-
pharmacological interventions in outpatient settings. This protocol would be used for
patients experiencing post burn associated pruritus. Expected outcome of the protocol
would be a reduction in post burn pruritus as determined by the 5 D Itch Scale and Visual
Analogue Scale (VAS). This project has three objectives: 1) to conduct a systematic
literature review; 2) identify non pharmacological and pharmacological relief
interventions; and 3) identify an implementation change model for clinical practice.
The target population for this project was all patients experiencing pruritus from
second and third degree burns in various stages of wound healing. This project included
post burn patients. The desired outcomes and benefits of this post burn pruritus protocol
will improve the quality of life in patients with burn injuries (Casaer et al., 2008).
Supporting Framework
This project used two supporting frameworks: the Preferred Reporting Items for
Systematic Reviews and Meta-Analyses (PRISMA) model and the Rosswurm and
Larrabee's model for evidence-based practice change. Further discussion of these models
will be discussed in this paper.
The purpose of this project was to construct a post burn pruritus relief protocol
through a systemic literature review to develop a protocol in order to improve the quality
of life in burn patients. The PRISMA model used to improve the reporting of systematic
reviews and meta-analyses was used as the standard guideline for this systematic review
(Liberati et al., 2009).
The Rosswurm and Larrabee's model of evidence-based practice change was also
used as an appropriate conceptual framework for evidence based practice in this project.
The model incorporates principles of quality improvement, use of team work tools, and
evidence-based translation strategies to support implementation of a new practice
(Melnyk & Fineout-Overholt, 2011). In this project, developing a post burn pruritus
protocol will promote quality care and improve patient outcomes. These frameworks
were explained in the methods section of this project and is also integrated in reporting
REVIEW OF LITERATURE
Overview
Bell and Gabriel (2009) reported the treatment of pruritus after burn injury by
reviewing ten research articles that were clinical trials that included nine class II and one
class III studies. Class II studies are reliable data that includes observational studies,
cohort studies, prevalence studies, and case control studies. Class III studies, on the other
hand, contain evidence provided by clinical series, comparative studies, case reviews,
case reports, and expert opinion. According to their review, both pharmacologic and
non-pharmacological methods significantly decreased post burn pruritus. Effective
pharmacologic methods are selective antihistamine antagonists (cetirizine/cimetidine) in
adult & pediatric population, Atarax and colloidal oatmeal (topical agent) in adult
population, Gabapentin and EMLA (topical agent) in pediatric population. Effective
non-pharmacologic methods contain pulsed dye laser and silicone gel sheeting in adult
and pediatric patients, and massage and transcutaneous electrical nerve stimulation
(TENS) in adult population. Bell and Gabriel (2009) suggested using moisturizing cream
for all patients with post burn pruritus with different treatment plans based on the size of
TBSA. According to the review by Goutos, Clarke, Upson, Richardson, and Ghosh
(2010), a multidisciplinary approach is necessary in successful assessment and treatment.
They recommended early use of centrally acting agents and peripherally acting agents as
well as non-pharmacological interventions for the treatment of post burn pruritus in adult
and pediatric populations. Rowley-Conwy (2014) also reported emollient cream, cool
baths, pressure garments, and oral and topical antihistamines and analgesics were
effective in decreasing burn associated pruritus. Rowley-Conwy (2014) also supported
multidisciplinary team to manage burn patients' recovery for the best outcomes of
physical, emotional, and psychological aspects.
Goutos, Dziewulski, and Richardson (2009) suggested therapeutic strategies
should be classified by interventions on peripheral & central aspects of the pruritic
pathway. Interventions that focus on the peripheral aspects of burns are: cooling of the
wound; antihistamines; topical Doxepin; local anesthetics; colloidal oatmeal; Capsaicin;
Laser therapy; Aloe Vera; topical Dapsone; Unna boot; Compression garments; and,
Ondansteron. Centralized interventions are Gabapentin; TENS; massage therapy; and,
psychological support (Goutos et al., 2009; Zachariah et al., 2011).
Findings for treatments to relieve post burn pruritus have been developed from
several research studies and included diverse methods. However, there was only one
suggested protocol found in the literature. This protocol focused on pharmacological
methods and required physician orders. Therefore, this project has conducted a systemic
review to develop a nurse driven post burn pruritus relief protocol.
Pharmacological Topical Interventions
Pharmacological interventions are often used to relieve pruritus in burn patients.
The first drug of choice for pruritus is antihistaminic drugs, especially, H1 antihistamines;
approximately 90.91% of burn patients have had antihistamines prescribed for post burn
pruritus (Goutos, 2010). According to Casaer et al. (2008), 23.3% of 258 adult and
pediatric burn patients in clinical settings received antihistamines during their research
study; and, those treated with antihistamines recalled that they felt reduced pruritus after
the treatment. However, because participants also had ointments applied for pruritus, it
was unclear how effective antihistamines alone were in decreasing pruritus. Ratcliff et
al. (2005) evaluated the effectiveness of a pharmaco-therapeutic protocol for pain,
anxiety, and itching among 286 acute pediatric burn patients in the hospital setting. They
reported that 39.2% of participants received medication to control itching at the
beginning, but eventually all the children took some type of oral itch medication because
their burn wound itching intensity increased as the wound progressed. Ratcliff et al.
(2005) accordingly recommended based on their research findings (1) moisturizing body
shampoo, lotions, and topical ointments (not hydrocortisone creams); (2)
Diphenhydramine 1.25mg/kg/dose orally every six hours; (3) if itch remains poorly
controlled, subsequently add Hydroxyzine 0.6mg/kg/dose every 6hours, then
Cyproheptadine 0.1mg/g/dose orally every six hours so that one of the medications could
be given every two hours.
Goutos (2010) stated that combination of H1 antihistamines and H2 antihistamines
significantly decreased pruritus compared to using only H1 antihistamines. Goutos
(2010) mentioned a combination of moisturization and three first generation H1
antihistamines was effective in 84% of acute burn inpatients. Second generation
antihistamines are not used for pruritus because first generation antihistamines are
commonly used for sedative effect as well as for pruritus relief.
The study by Goutos (2010) demonstrated that 10 out of 22 burn units used
additional pharmacological agent. Of the 10 units, 6 units used a second antihistamine, 1
used Ondansetron (serotonin receptor antagonist), and 3 used gabapentin with alone or
combining with an antihistamine. Gabapentin has been more effective relieving pruritus
in acutely burn patients than first generation antihistamines; especially, Chlorpheniramine
Ahuja and Gupta (2012) compared the use of Pregabalin to other medicine in
managing post burn pruritus for 80 adult patients in outpatient setting. They reported that
the group using both antihistamine and Pregabalin and the group using Pregabalin only
showed higher rates of remission of itching in post burn population compared to the
group of using antihistamine only. However, in the population of mild itching, using
both antihistamine and Pregabalin had a much higher rate (77.5%) than using only
Pregabalin (23.3%) regarding reducing itching.
Akhtar & Brooks (2012) explored the effect of botulinum toxin (Botox®) as a
new agent in managing post burn pruritus and found that Botox® successfully decreased
pruritus in 8 outpatient adult burn population who were resistant to conventional
therapies. All eight post burn patients described itching as "0" out of 10 at 2weeks after
Botox® injection. The average duration of no pruritus after the treatment was 9 months.
The study of Baker et al. (2001) demonstrated the combination of histamine 1
(H1) receptor blocker and histamine 2 (H2) receptor blockers significantly reduced post
burn pruritus than using H1 receptor blocker only during the first 4 days of treatment in
17 adult and pediatric patients. After 4days of treatment, there were no differences
between two cases. Baker et al. (2001) also reported that programmed (scheduled)
medication rather than medication on demand (PRN) contributed to the reduction of
pruritus. The review by Goutos (2013) also reported that aggressive antihistamine was
effective in the early phase, but in the later stages wounds appeared to be less effective to
antihistamine therapy.
Mendham's (2004) study was done to test the action of gabapentin on itching in
healing wounds among 35 children admitted to the inpatient burn unit. The research
sample was the population who had been treated with Chlorpheniramine and
Trimeprazine, but still remained irritable and constantly itching wounds at the beginning
of the research. Gabapentin was given starting as 5mg/kg three times a day and
maximum dose increased up to 5mg/kg twice a day and 10mg/kg at night. Within 24
hours of gabapentin use, parents and nursing staff assessed the effects of the treatment
and they stated that there was a remarkable reduction in itching and they had decreased or
unused antihistamine intake.
Ahuja, Gupta, Gupta, and Shrivastava (2010), studied the effectiveness of
gabapentin in decreasing post burn pruritus comparing to using cetirizine alone and
combination of gabapentin and cetirizine for 28days in 20 burn patients with ages of 12
to 70 years. The study showed that using gabapentin alone reduced itching in 95% of
people in the group while cetirizine alone used group and combination of gabapentin and
cetirizine used group reduced itching to 52% and 94%, respectively. In addition, the
study demonstrated that the onset of action with gabapentin was significantly faster than
the cetirizine. According to Ahuja et al. (2010), 74% in gabapentin group stated the relief
of pruritus whereas 32% in the group with cetirizine alone stated pruritus relief on the
third day after the treatment. Ahuja et al. (2010) suggested the need for pruritus relief
protocol as well as the need for appropriate dosage of gabapentin treatment was needed to
reduce post burn pruritus.
Goutos, Eldardiri, Khan, Dziewulski, and Ricahrdson (2010) compared
gabapentin treatment with antihistamine treatment in relieving acute post burn pruritus
among 91 adult and pediatric burn population of inpatient setting. Gabapentin
monotherapy was four times more effective than Chlorpheniramine monotherapy in acute
burn pruritus (41.46% vs 10%). As an antipruritic polytherapy in acute burns,
combination of gabapentin, cetirizine and Cyproheptadine was more effective than the
combination of three antihistamines (Chlorpheniramine, Hydroxyzine, and
Cyproheptadine) in relief rate of pruritus in post burn population. The outcome was
95.12% and 84%, respectively. Goutos et al. (2010) also suggested polytherapy in
younger population and larger TBSA because monotherapy had higher failure rate in
younger populations.
Anand (2012) showed the effectiveness of gabapentin for pruritus in palliative
care, too. According to the literature review by Anand (2012), gabapentin is safe and
effective in uremic pruritus, cancer and hematologic causes, opioid-induced itch,
brachioradial pruritus, burns pruritus, and pruritus of unknown origin. In the study by
Goutos (2013), gabapentin had persistent therapeutic effect because of the ability to
prevent central nervous system sensitization; Ondansetron was more effective in reducing
pruritus than antihistamine; serotonin had pruritus relief effect; and TENS was more
effective in reducing post burn pruritus during the remodeling phase. Warner, Coffee,
and Yowler (2014) supported efficient outpatient burn management by using H-1
receptor blocking agent (cetirizine) during the early stage of pruritus as scheduled basis
not as needed basis combined with frequent massage of moisturizers. In addition, neuro-
inflammatory transmitter blockers (Gabapentin and Pregabalin) are effective because
they prevent neuron transmitters from stimulating itch-specific neurons (Warner et al.,
The study by Otene and Onumaegbu (2013) revealed that 88.6% of 35 plastic
surgeons had no assessment tool or method to evaluate post burn pruritus while only
11.4% believed they had a method of assessing the severity of post-burn pruritus. Otene
and Onumaegbu (2013) also stated that "57.1% would use oral medications as first-line
treatment, 22.9% would use injectables, 8.6% would use topical agents, 5.7% would only
reassure the patients and another 5.7% would use a combination of oral and topical
agents together. 85.7% of these plastic surgeons and burn care specialists did not have
any form of anti-pruritic regimen, as only 14.3% indicated having this". Otene and
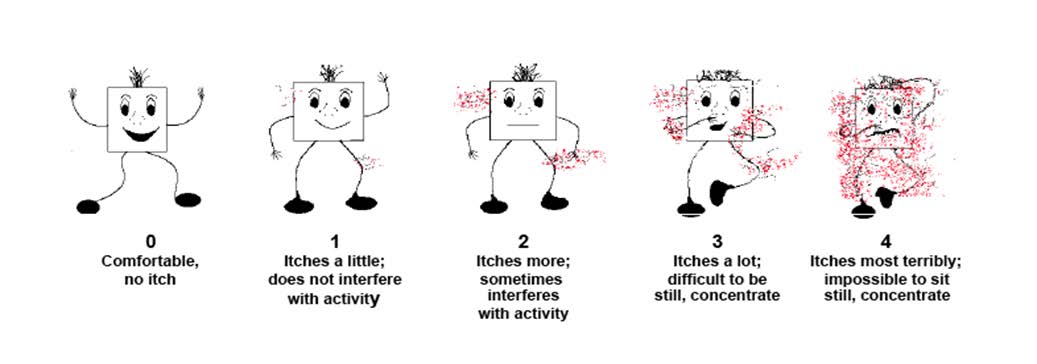
Onumaegbu (2013) recommended Itch Man Scale as an assessment tool for pruritus and
suggested rough guidelines as a pruritus relief management according to the score
measured by Itch Man Scale.
According to the review by Brooks et al. (2008), topical agents such as capsaicin
and nanocrystalline silver ointment can be used to reduce pruritus. These drugs can also
be used as part of a combination therapy. Topical steroid, Doxepin or Dothiepin cream (a
tricyclic antidepressant), and EMLA can be used as part of a combination therapy in
pharmacological interventions.
One topical agent, Provase®, is a nonprescription moisturizer with a blend of
protease enzymes. Nedelec, Rachelska, Parnell and LaSalle (2012) performed a
prospective, double-blind, randomized, controlled, and pilot study to evaluate the effect
of Provase® in reducing post burn pruritus in 18 burn patients. According to Nedelec et
al. (2012), the application of Provase® to post burn population significantly reduced the
duration and the frequency of pruritus, area of itch, and the presence of affective itch
characteristics. For instance, treatment group reported the area of itch was decreased to
half after four weeks of Provase® application.
La Salle, Rachelska, and Nedelec (2007) evaluated the effect of naltrexone in
managing post burn pruritus among 13 adult population in inpatient and outpatient
settings. They reported research participants who had failed with H1 or H2 receptor
antagonist and hydrating lotion demonstrated some satisfaction of naltrexone use in
reducing post burn pruritus. Overall, 50% of research participants improved the
frequency and duration of itching, 72% were satisfied with the itch relief provided by
naltrexone, and 62% stated that quality of life improved by using naltrexone. Jung et al.
(2009) did a study to determine the effects of naltrexone as a potential antipruritic
medication for 19 adult burn population in the inpatient setting experiencing chronic
refractory itching. All of the research subjects were population who had failed in
reducing post burn pruritus with antihistamine, gabapentin, or both antihistamine and
gabapentin before. However, researchers found out that 44.5% (9 patients) of research
subjects reported decreased scratching activity two weeks after using naltrexone.
Mugwort lotion seems to be effective in treating the itch associated with post burn
pruritus who had hypertrophic scars (Ogawa & Hyakusoku, 2008). Mugwort lotion
significantly decreased pruritus, sleep disturbance and redness after 2 months of
treatment in 14 adult post burn patients of inpatient setting suffering from hypertrophic
scars in the study by Ogawa & Hyakusoku (2008).
Lewis et al. (2012) explored the efficacy of Medilixir (mixture of coconut, palm,
castor, olive, hemp seed, wheat germ, and canola seed oil) compared to the standard
treatment of aqueous cream (mixture of paraffin, heavy liquid, phenoxyethanol, and
purified water) regarding relieving the post burn itch symptoms. Research findings
indicate that Medilixir is more effective in minimizing post burn pruritus than aqueous
cream in 52 adult burn population of inpatient setting.
Campanati et al. (2013) evaluated the clinical effect of the topical application of
Ozonated oil on second degree skin burns comparing to the treatment with hyaluronic
acid gel. Thirty adult patients were applied Ozonated oil on half of the burn lesion and
hyaluronic acid on the other half of the lesion once a day for 12weeks. Clinical features
of each lesion (erythema, tension, height, itching, and burning sensation) were assessed at
baseline, six, and twelve months after treatment. Ozonated oil had the same efficacy of
hyaluronic acid in reducing symptoms related to burns (erythema, tension, height,
itching, and burning sensation) after 12 weeks of topical application.
Non-Pharmacological Interventions
Studies that have non-pharmacological interventions in relieving pruritus for burn
population include: psychological interventions, massage therapy, silicone sheeting for
burn wounds, hypnosis, TENS (transcutaneous electrical nerve stimulation), and Unna
boot application (Brooks et al., 2008). Cold water, cold temperature, and rest also can
relieve pruritus in some burn population (Parnell et al., 2012). The study by Goutos
(2010) found that 2 out of 22 burn units utilized psychologists, 2 units used massage
therapy, and 1 unit used silicone products for pruritic wounds and these methods were
effective in reducing pruritus in burn patients.
According to Upton, Penn, Richardson, and Rippon (2014), psychological
approaches are effective in reducing wound itching. Upton et al. (2014) reviewed 12
published articles regarding psychological methods (habit reversal, suggestions,
relaxation training, massage, and itch-coping programs) are used to treat wound
associated pruritus. The study finding demonstrated psychological methods reduced
itching but this approach was supported by only one article. Psychological interventions
can be applied with consultation of a psychologist in conjunction with other therapies.
Muscle relaxation methods decrease itching in burn populations. Farahanil,
Hekmatpou, and Khani (2013) investigated the effect of muscle relaxation on pain,
pruritus, and vital signs among 110 hospitalized adult and pediatric patients suffering
from burns. They assessed pain, pruritus, and vital signs before and after the Benson
relaxation method was applied. According to the study, muscle relaxation technique was
effective in relieving the pain, pruritus, and vital signs of patients suffering from burns.
Brooks, Phang, and Moazzam (2007) performed a case study with 5 cases
including 7, 20, 40, 45, and 65% of TBSA having mixed-thickness burns from both
inpatient and outpatient clinic and reported the effect of Acticoat® (Nanocrystalline
silver) for itch relief in burn patients. Acticoat® was applied for 2 weeks and the
intervals from original injury to application were 2, 3, 3, 6, and 8 months. Before and
after 2 weeks of application, Visual Analog Scale (VAS) of itching was assessed and
compared. VAS score was 7.4 before application and it decreased to 3.1 after application
of Acticoat® (
p = 0.002) which significantly reduced post burn pruritus. However, the
study did not indicate the condition of wounds. For example, whether the burns were
healed or unhealed was not stated. It is assumed they were unhealed or in the healing
process because Acticoat® is used for unhealed wounds in current practice.
Field et al. (2000) performed a randomized controlled trial (RCT) to evaluate the
effect of massage therapy in reducing post burn itching, pain, and psychological
symptoms of 20 adult burn patients in the outpatient setting suffering from pruritus. The
research finding is massage therapy significantly decreases itching, pain, depression, and
anxiety in post burn population with severe itching. According to Gurol, Polat, and
Akcay (2010), massage therapy effectively alleviates pruritus in 63 burn adolescent
inpatients even though this application is not commonly used. Pfab et al. (2013) reported
in their review that 15 minute massage therapy twice a week over 5weeks reduced
itching, pain, and anxiety levels in burn adolescents. The study by Cho et al. (2014)
reported the effect of burn rehabilitation massage therapy on 146 adult inpatients with
hypertrophic scars after acute burn care. Their findings indicated that burn massage
therapy is effective in improving pain, pruritus, and scar characteristics in hypertrophic
scars after burn (Cho et al, 2014).
TENS is known as an ideal method of treating itching. The case study by
Whitaker (2001) exhibited the effect of TENS in decreasing post burn pruritus. Whitaker
(2001) applied TENS to a 19 year old patient at the inpatient setting who suffered from
severe itching after being healed from 70% mixed thickness flame burns. After two
weeks of using the TENS unit in the study, the patient did not need to continue the use of
the TENS unit because post burn pruritus no longer existed. Hettrick (2004) evaluated
the effect of TENS as the management of burn pruritus in a pilot study with RCT on 20
adult burn patients in the outpatient setting and reported TENS significantly reduced post
burn pruritus in the population sampled. In the study, Hettrick applied one hours of
TENS per day, 7 days a week for 3 weeks to the experimental group. It was suggested
that TENS should be considered as a treatment option for burn survivors whose quality of
life was negatively affected by itching (Hettrick, 2004).
Silicone gel sheeting is considered effective in reducing scar pigmentation, pain,
and itching as well as improving scar thickness and pliability (Li-Sang, Lau, Choi, Chan,
& Jianan, 2006). The study by Li-Sang et al. (2006) demonstrated significant efficacy of
silicone gel sheeting on severe post-traumatic hypertrophic scars among 45 Chinese adult
outpatient burn population in their RCT. In a similar study, Li-Tsang, Zheng, and Lau
(2010) investigated the effect of pressure therapy, silicone gel sheeting, and combined
therapy on management of posttraumatic hypertrophic scar among 104 adult and
pediatric burn population in the outpatient setting. All three methods significantly
reduced itching but silicone gel sheeting had better results but was not statistically
significant (Li-Sang et al., 2010).
Laser therapy is one of ways to relieve pruritus. According to pretest and posttest
designed study by Gaida et al. (2003), low level laser therapy (LLLT) was effectively
decreased pain and pruritus in 19 adult post burn population of the outpatient setting.
Likewise, Hultman, Edkins, Wu, Calvert, and Cairns (2013) reported that laser therapy
on burn scars significantly improved pain, pruritus, pliability, and paresthesia among 147
outpatients (
P < 0.0001).
Waked, Nagib, and Ashm (2013) evaluated the effectiveness of triamcinolone
acetonide phonophoresis (TAP) compared to TENS in the treatment of post burn pruritus
for 40 adult inpatients. According to the researchers, there was a significant
improvement in reducing pruritus in both group with TAP and the group with TENS
(P<0.05). However, there was no significant difference between the two groups
regarding the effect of pruritus reduction.
Richardson, Upton and Rippon (2014) suggested an algorithm for the mechanism-
based treatment of post burn pruritus based on the stages of healing. According to the
algorithm by Richardson et al. (2014), there are four stages that include: inflammatory,
inflammatory/proliferative, proliferative/remodeling, and remodeling. Each stage has
different treatment methods. However, this algorithm is the only algorithm suggested
and requires validation with further use in multiple studies.
Summary of Literature Review
Summary of the literature review shows that Oral anti-pruritic medications are the
first drug of choice and they can be given as a scheduled dose by combining with other
anti-pruritic medications to be more effective in decreasing pruritus in post burn wounds
regardless of wound healing stages. In addition, topical agents decrease post burn
pruritus in healed wounds, especially, hypertrophic scars. These topical agents can be
used with oral anti pruritic medications or after oral anti-pruritic medications have failed
to relieve post burn pruritus.
In addition, non-pharmacological interventions decreased post bun pruritus as
effectively as pharmacological interventions. Effective non-pharmacological
interventions were psychological intervention (habit reversal, suggestions, relaxation
training, and itch-coping programs), pressure therapy, laser therapy, TAP, TENS,
Massage, special dressing (silicone sheeting, Nanocrystallin [Acticoat®], and Unna
boot), hypnosis, cold water, cold temperature, and rest. However, pharmacological
interventions were suggested to augment non-pharmacological interventions to maximize
This literature review analyzed 38 articles regarding post burn pruritus. 23
articles among them used VAS as a pruritus assessment tool, two articles used Itch man
scale, two articles used both Itch man scale and VAS, and two articles used 5-D Itch
scale. On the other hand, nine articles did not clearly state which pruritus assessment tool
was used. Moreover, each treatment method was supported by less than five studies and
most studies were relatively small sample size.
Methods for this project included incorporating two models, the PRISMA model
and the Rosswurm and Larrabee model of evidence-based practice change. Consistent
with a systematic review, a table of evidence (TOE) was used for organization of the
research studies (Appendix C). Methods contain: search strategy, eligibility criteria,
study selection, data collection process, data extraction, quality assessment, and results.
PRISMA Model
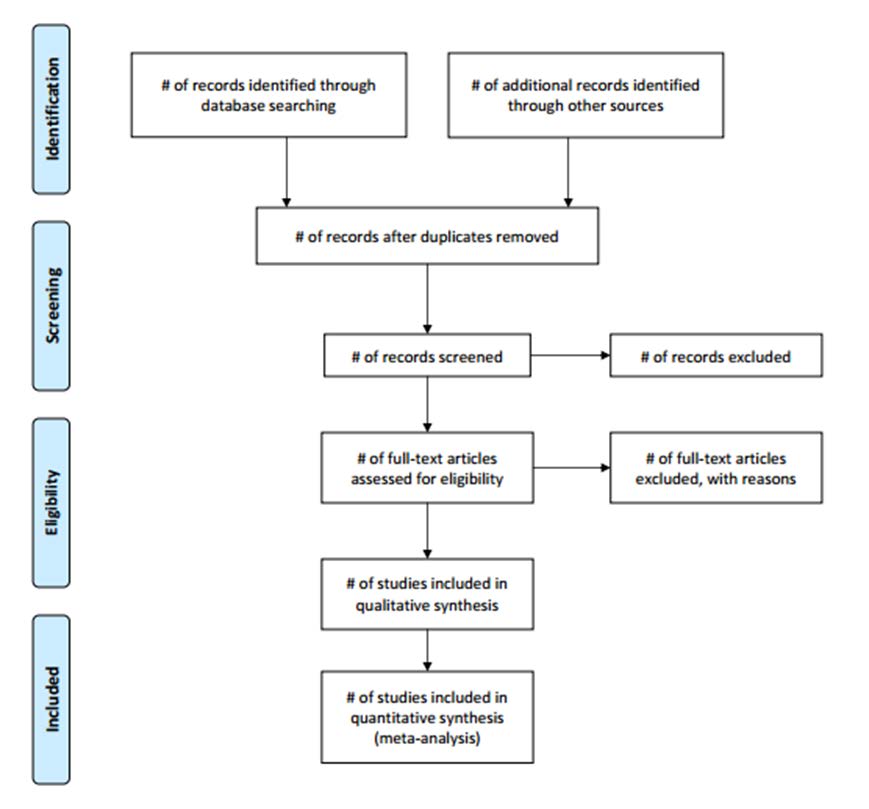
This project partly adopted the PRISMA flow diagram during the process of study
selection and data collection. By using the PRISMA flow diagram, the selecting process
of studies in this project was transparent. Steps for selecting research studies are
identified in the PRISMA flow diagram (Figure 1), and includes: identification,
screening, eligibility check, and inclusion of data.
The PRISMA model for organizing and reporting systematic reviews includes an
abstract, background, problem statement, purpose statement, methods, results, and
discussion sections. These steps will be clearly delineated as headings throughout this
paper. In the health sciences, 174 journals have used the PRISMA model for reporting
systematic reviews and meta-analysis in their collections (Moher et al., 2009).
The PRISMA model has also been considered as an assessment tool for research
dissemination within the Enhancing the Quality and Transparency of Health Care
Research (EQUATOR). The EQUATOR is an international initiative that seeks to
improve reliability and value of health related research by promoting accurate and clear
reporting of research studies (International Prospective Register of Systemic Reviews,
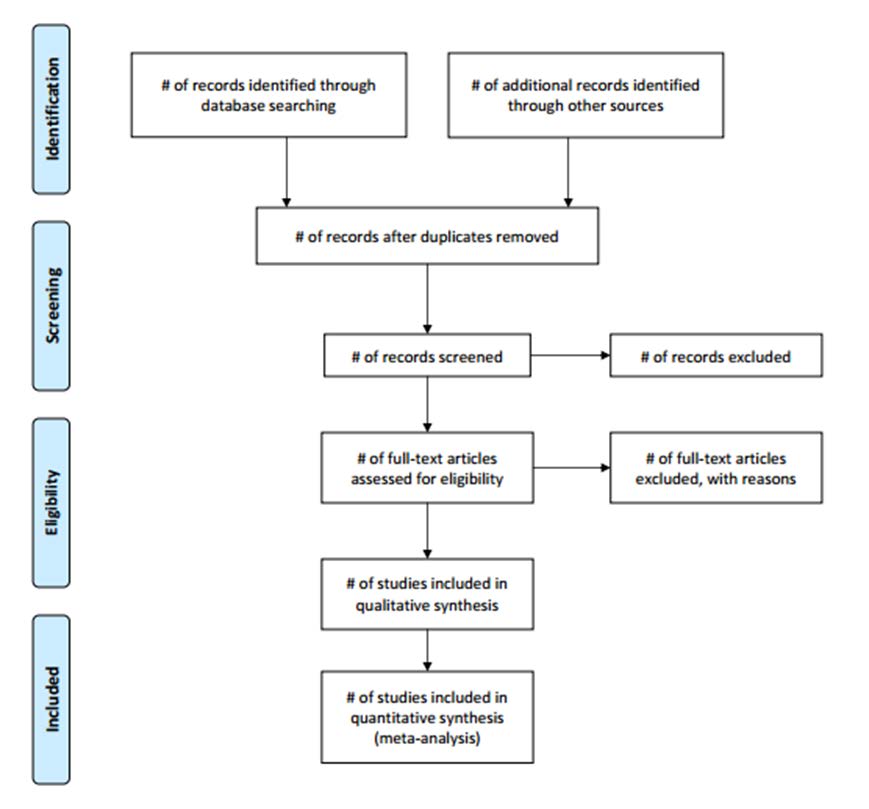
Figure 1. PRISMA 2009 flow diagram (Moher, Liberati, Tetzlaff, & Altman, 2009).
The Model for Evidence-based Practice Change
Another framework for this project is the model for evidence-based practice
change. This model, published by Rosswurm and Larrabee (1999), was a model used to
change practice in an organization (Melnyk & Fineout-Overholt, 2011) and is closely
related to the PRISMA model in that steps overlap.
The Rosswurm and Larrabee model was based on theoretical and empirical
literature related to evidence-based practice, research utilization, standardized language,
and change theory. In this model, practitioners are guided through the entire process of
developing and integrating an evidence-based practice change. The model supports
evidence-based practice changes derived from a combination of quantitative and
qualitative data, clinical expertise, and contextual evidence (Rosswurm & Larrabee,
1999). Because the purpose of this project was to develop a protocol to improve post
burn pruritus and related symptoms, the model for evidence-based practice change was
an appropriate framework for practice (Figure 2).
In this model, step one included the background, problem statement, and literature
review. In addition, step one assessed the need for change in practice by identifying the
problem, inclusion of stakeholders, data collection of current practice, and development
of a population-intervention-comparison-outcome- and time frame (PICOT). Step two
was to locate the best evidence by identifying types and sources of evidence, reviewing
research concepts, planning the search, and conducting the search (Table 1). Step three
analyzed the evidence. This step included appraisal of the evidence, syntheses of the best
evidence, and assessment of feasibility, benefits, and the risks of new practice. This
project established incorporated step three under literature review and result. Step four
was to design practice change and the development of a post burn pruritus relief protocol
was the outcome of this step, and the protocol is contained in the results section. For the
purposes of this time-limited DNP project steps five and six were not included and
developing of a post burn pruritus relief protocol was sufficient, but this protocol will be
tested in future research studies.
Figure 2. A model of evidence-based practice change (Larrabee, 2009).
Search Strategy
Four data bases: Cochrane Central Register of Controlled Trials, CINAHL the
Cumulative Index of Nursing and Allied Health Literature, EBSCO, and PubMed were
searched. In addition, The National Guideline Clearinghouse, and the following
websites: Bandolier, The National Health Service (NHS) Center for Reviews and
Dissemination, google scholar, and the American Burn Association (ABA) web site were
used for searching data. Research articles were searched from September 1, 2013 to
November 17, 2014. Key words linked with Boolean "AND" included burn(s), itch(ing),
itch(es), pruritus, and pruritic.
Data Extraction and Quality Assessment
In accordance with the PRISMA guidelines, articles were collected, studies
reviewed for validity, potential bias, and threats. This review also included reviewing the
articles for clarity of the clinical question, inclusion criteria, the relevance of the clinical
question, study design, data collection, and analysis methods.
Eligibility Criteria
According to the Iowa Model, systematic literature review was performed by
formulating a focused clinical question about post burn pruritus (Holly, 2014). The
question in the project is "In populations with burn injury, what measures are effective in
minimizing post burn pruritus?" Initially, studies published within last five to seven
years were inclusion criteria, but there were insufficient literature during the period.
Therefore, the criteria for eligibility was expanded to all published studies written in
English from 2000 to 2014 that performed on all second and third degree burn population
suffering from burn related pruritus to collect sufficient data for the project.
Study Selection and Data Collection Process
Purpose, design, sample, setting, findings of each study were recorded for the
studies that were included in this review. Each paper was reviewed and analyzed
descriptively. The systemic literature search of articles indicated that 38 studies met the
inclusion criteria. A total of 79 articles were searched and 41 articles were excluded
according to the flow diagram (Figure 3). First four articles were excluded; one was
written in German, one was only response to the editor of the other article, and the other
two articles were reviewed in other articles (duplication of research findings).
Figure 3. Flow diagram for selection of studies.
Next 22 studies were removed conforming to eligibility criteria: Seventeen
articles were related only to scar, skin condition, and scar assessment; two studies were
only regarding sleep quality in burn patients; and three articles stated general burns and
their treatment only. Five articles were excluded because they were written about
pruritus assessment tool development and evaluation only. Also, another study was not
included because it stated general wound itching instead of writing specifically about post
burn associated itching. Nine articles were excluded because they described only pruritus
and did not write pruritus relief methods. Therefore, 38 articles were reviewed to
develop a post burn pruritus relief protocol and significant findings of each study were
shown in Table 1. Details of each publication was written in the Table of Evidence
(TOE) under Appendix B. The TOE was constructed according to purpose, design,
sample, setting, operational definition, findings, limitation of each study, and comments.
A synthesis of each study was reported at the end of the review of literature.
Table 1 Characteristics of Included Studies
Characteristics of
Ahuja & Outpatient
TBSA > 5%, 2nd degree
Pregabalin alone or combined antihistamine
burns, & wound either in
w/pregabalin → ↓ PBP
Addition of antihistamines does not decrease
epithelialized) or healed
PBP Massage therapy can be used as adjunctive treatment
TBSA > 5%, 2nd degree
Gabapentin alone or combination of gabapentin
burns, over 80% of wound
& cetirizine → ↓ PBP
epithelialized or healed
Certirizine only does not decrease PBP
Prospective& All healed areas after 2nd -
Botox → ↓ PBP in the population who failed in
3rd degree burns
managing PBP w/ conventional therapies/ 50%
8 pts w/ failure
had no PBP within 2wks after Botox treatment/
free of itching up to average 9 months after
Gabapentin → ↓ PBP & ↓ in morphine demand
Zofran is second method for PBP.
Other methods (cooling of wound,
antihistamines, local anesthetics, topical doxepin, colloidal oatmeal, capsaicin, laser treatment, dapsone, unna boot, compression garments, &
TENS) → ↓ PBP
Characteristics of
Baker et Setting not
Partial thickness & any %
Combination of H1 receptor antagonist
(cetirizine) & H2 receptor antagonist
Not specified in description
(cimetidine) is more effective in decreasing PBP
of wound healing stage
than H1 receptor antagonist (diphenhydramine)
during the first stage of treatment. It is more effective to treat PBP w/ scheduled medication than w/ as needed medication
Burn associated wound w/
All PBP- Moisturizing cream, massage
10% TBSA or less- antihistamine, colloidal
Not specified in the stage of
oatmeal w/ liquid paraffin, topical antihistamine,
silicone gel sheeting
More than 10% TBSA- oral non selective antihistamine, oral selective antihistamine, oral gabapentin
Not specified in the stage of Not
Algorithm consisting of 4 steps of treatment
1st- oral antihistamine, topical emollient, 2nd –
clinical psychologist, 3rd – massage, silicone
sheeting, hypnosis, TENS, unna boot, topical nanocrystalline silver, capsaicin, 4th – 8topical antihistamines, H1&H2 a9ntagonists, topical steroid, doxepin, EMLA, gabapentin, dothiepin cream
TBSA range 7-65% w/
2weeks of Acticoat (Nanocrystalline silver)
unhealed burn wound
application is effective in PBP.
Unclear setting/
2nd degree burns in healing
Ozonated oil & hyaluronic acid have the same
effect in reducing PBP 12 weeks of topical
Characteristics of
Ozonated oil is more effective than hyaluronic acid in preventing post hyperpigmentation.
All healed burn wound
Massage therapy is effective in improving pain,
hospital setting/
pruritus, & scar characteristics in hypertrophic
scars after burn.
hypertrophic scars
Inpatient setting/ Quasi-
2nd degree burn wounds
Twenty-minute Benson muscle relaxation is
110 hospitalized experimental
Stage of wound healing not
effective in relieving PBP.
clear-possibly not healed
wound considering
Healed burn wound
Massage therapy significantly decreased itching,
pain, depression & anxiety in PB population w/
severe itching (30 min x 2days per week x
Healed burn wound (scar)
LLLT demonstrated improvement in pain &
pruritus among all participants.
All stages of healing in
Aggressive antihistamine is effective in the early
phase, but less effective in the later stage of
Gabapentin is persistent in decreasing PBP. Ondansetron-more effective than antihistamine. Serotonin- antihistamine effect TENS-effective in remodeling phase
Characteristics of
Varied by methods of
Peripheral & central aspects of pathway need to
be included in decreasing PBP.
Peripheral - cooling of the wound,
antihistamines, topical Doxepin, local
anesthetics, colloidal oatmeal, Laser tx, Aloe
Vera, topical Dapsone, Unna boot, Compression
garments, Ondansteron.
Central - Gabapentin, TENS, Massage therapy, Psychological support
Inpatient setting/ Cohort,
Partial to full thickness
Monotherapy in PBP: gabapentin monotherapy
observational burn injury.
has more effective than chlorpheniramine.
Healing stages not
Polytherapy in PBP: Combination of gabapentin,
the study, 41-2nd Intervention
cetirizine, & cyproheptadine is more effective
than combination of 3 antihistamines
(chlorpheniramine, hydroxyzine, &
Inpatient setting/ Experimental 2nd to 3rd degree burn
15minute massage twice per week for 5weeks
applied to healthy skin around the wounds &
Healing stage not specified.
surface of wound decreased PBP in adolescent
2nd to 3rd degree recently
TENS significantly reduced PBP in the target
healed burn wound
All healed burn wounds
Laser therapy decreased pain, pruritus, pliability,
& paresthesia in population with hypertrophic
Characteristics of
Cairns (2013) Jung et
Healed burn wounds
With Naltrexone therapy,14 pts reported
rehabilitation /
improvement in experience of itching & 5 pts
reported no change in itching.
Experimental TBSA of 7-70% & all
Participants stated satisfaction with Naltrexone
grafted burn areas.
in decreasing PBP & improved regarding
Healing stages not specified
frequency & duration of itching.
Lewis et Inpatient setting
Mean TBSA:7.2%, mostly
Medilixir is more effective to minimize PBP
partial thickness burn
than aqueous cream.
wound & newly healed scar
Post traumatic hypertrophic VAS
SGS was effective to reduce thickness, pain,
itchiness, & pliability of the severe hypertrophic
SGS showed more effective in decreasing pain
and pruritus than the scar thickness.
CTG & PG group showed significant
improvement in scar thickness after 6 months of
intervention (CTG>PG).
Inpatient setting
Experimental Burn wounds and skin loss
Gabapentin reduced itching in healing wound &
from meningitis.
decreased antihistamine intake in pediatric
Not healed wound
Characteristics of
Nedelec, Not clear /
All healed burn wounds
Provase decreased PBP in weekly frequency,
daily episode of itch, & duration of itch episode.
& La Salle (2012) Ogawa
Inpatient setting/ Prospective,
All healed burn wounds
Mugwort lotion is effective for improving
itching & sleep disturbance. (Two months of
Mugwort treatment decreased symptoms)
scars from burns
PBP relief methods used by % of plastic
surgeons - 57.1 (oral meds), 22.9 (Injections),
8.6 (topical agents), 5.7 (reassure pts), 5.7
(combination of oral & topical agents). 85.7
without anti-pruritus protocol.
Any skin conditions that
15 minute massage therapy twice a week over
5weeks reduced itching, pain, & anxiety levels
in burn adolescents.
Inpatient setting
Itching management protocol for children;
: Various wound stages
1)Moisturizing body shampoo & lotions, topical
ointments (not hydrocortisone creams)
2)Diphenhydramine 1.25mg/kg/dose po Q 6h
3)If itch remains poorly controlled, subsequently add hydroxyzine 0.6mg/kg/dose q 6h, then cyproheptadine 0.1mg/kg/dose po q6h so that
one of the medications is given q2hrs
Characteristics of
Four different stages of
PBP management algorithm per 4 healing
Literature up to
healing in burn wounds
phases of wound suggested – inflammatory
phase, inflammatory/proliferative phase,
proliferative/remodeling phase, & remodeling
Burn scars from partial or
PBP significantly decreased by SRMT in burn
full thickness burns on
victims with scars from partial to full thickness
on the forearm or hand.
Double-blind All stages of burn wound
PBP is reduced with massage w/ emollient
cream, cool baths, pressure garments, & oral and
topical antihistamines & analgesics.
Any skin conditions
Five psychological approaches to treat wound
causing pruritus- atopic
associated itching are suggested.
dermatitis, burn wounds,
(Habit reversal, Suggestions, Relaxation
skin disorders, pruritic skin
training, Massage, & Itch-coping programs)
Inpatient setting
2nd & 3rd degree burn
Triamcinolone acetonide phonophoresis is as
wounds, 10-15% TBSA. –
useful as TENS to reduce PBP
& Ashm 40 burn pts
All Healed scars
All phases of burn wounds
Early pruritus management: H-1 receptor
blocker (cetirizine) on as scheduled basis not as
needed basis combined with frequent massage of
Neuro-inflammatory transmitter blockers (gabapentin & pregabalin) is effective because itch-specific neurons won't be stimulated by
Characteristics of
using this medicine.
Inpatient setting
Healed 70% TBSA flame
2 weeks of TENS is effective in decreasing PBP.
burn wound (scar)
Day #1: 62.5% decreased in itching within 4hrs
Day #2: 88% decreased within 4hrs of application. Day #3: No itching within 4hrs of application.
All burn wounds.
Current tx options for PBP summarized;
Healing stage not specified
Antihistamines (H1 & H2 receptor antagonists),
Topical alternatives over the healed burn
wounds (colloidal oatmeal baths, EMLA, corticosteroids, massage therapy, Doxepin cream).
Adjuncts (Biofeedback therapy, psychological support, combined w/pharmacological agents, TENS), Newer medicine: Ondansetron (5HT-3 receptor antagonist), Gabapentin (anti-epileptic drug), Pregabalin (anti-convulsant), Paroxetine (SSRI), & Naltrexone (opioid antagonist)
Notes. CTG = combined pressure therapy and silicone gel sheeting group; EMLA = eutectic mixture of local anesthetic; h = hour; hrs = hours; H1 = histamine 1; H2 = histamine 2; LLLT = low level laser therapy; PBP = post burn pruritus; PG = pressure therapy group; pts = patients; RCT = randomized clinical trial; SGS = silicone gel sheeting; SRMT = skin rehabilitation massage therapy; SSRI = selective serotonin reuptake inhibitor; TBSA = total body surface area; TENS = transcutaneous electrical nerve stimulation; VAS = visual analog scale.
PROJECT MANUSCRIPT
Thirty-eight articles were reviewed. Eighteen articles identified pharmacological
effects on post burn pruritus that included single medicine use and two or three combined
medicine. Effective pharmacological, both oral and topical, methods used in decreasing
pruritus were antihistamines, Pregabalin, analgesics, corticosteroids, Gabapentin,
Naltrexone, Botox, Provase, Capsaicin, colloidal oatmeal, Aloe Vera, topical Dapsone,
Doxepin, Mugwort lotion, EMLA, Ozonated oil, and hyaluronic acid. Fifteen of the
thirty eight articles stated positive non-pharmacological methods in relieving post burn
pruritus. Examples of effective non-pharmacological methods included: cool bath,
massage therapy, laser therapy, TENS, TAP, muscle relaxation, psychological approach,
biofeedback therapy, silicone gel sheeting, Acticoat®, and pressure garment therapy. Of
the studies, five supported combination of pharmacological and non-pharmacological
methods to reduce post burn pruritus.
The outcome of the systemic literature review regarding pruritus relief in post
burn populations was synthesized and evaluated based on best outcomes which are
pharmacological and non-pharmacological interventions. Accordingly, an advanced
practice nurse (APN) driven post burn pruritus relief protocol was developed (Figure 4).
This protocol was designed to apply to three different stages of wound healing such as:
pre-healing (no granulation tissue); healing (partly granulated tissue); and healed stages
(scar formation); and, recommended dosages per each intervention (Table2). Non-
pharmacology interventions are recommended before pharmacological interventions
based on established effectiveness.
1. Non-Pharmacological methods (Single or multiple options)
• Massage therapy to intact skin areas except wound (priority)
• Benson Muscle Relaxation therapy
2. Pharmacological methods (Single option only: same priority)
• Pregabalin alone (if not effective) Pregabalin + 2 H1 blockers
• Gabapentin alone (if not effective) Gabapentin + H1 blocker (if not
effective) Gabapentin + 2 H1 blockers
• Combination of H1 & H2 blockers
3. Supplementary pharmacological method (additional option): Naltrexone
All methods for pre-healing wound stage
Topical agents (Ozonated oil or Hyaluronic acid gel 0.2%)
1. Non-pharmacological methods (single or multiple options)
• Moisturizing body shampoo
• Benson muscle relaxation
• Massage therapy applied to healed wound
• Acticoat® (Nanocrystalline Silver)
• Silicone Gel Sheeting
• Pressure garments (Unna boot®)
2. Topical agents (Select one opti on)
• Mugwort lotion
• Ozonated oil
• Hyaluronic acid gel 0.2%
3. Supplemental Intervention (single or multiple options)
• LLLT or regular laser th erapy
Above methods failed
Oral: Zofran® (ondansetron), Serotonin, SSRI (Paroxetine), Tricyclic
antidepressant (Doxepin), Gabapentin, Naltrexone.
Topical: Antihistamines, H1 & H2 antagonists, Botox®, Topical Steroid,
EMLA® Cream (lidocaine 2.5% & prilocaine 2.5%), Dothiepin (Tricyclic agent)
Figure 4. Post Burn Pruritus Relief Protocol.
Table 2 Post Burn Pruritus Relief Protocol Guideline (Recommended Dosage)
Recommended Dosage
(refer to article No. in Table 1)
Massage therapy to intact skin
15 minutes/day, 2 days/week, 5 weeks or as needed.
Benson Muscle Relaxation therapy
20 minutes daily for 1 month or as needed (11)
Pharmacological treatment
(1, 2, 5, 6, 16, 25)
- Pregabalin alone
- 150-300mg/day (divided by 2 or 3 times)
- Pregabalin & two antihistamines
- Pregabalin (same dose),
Cetirizine 10-20mg/day (one or twice a day), &
Pheniramine 25mg/day before sleep
- Gabapentin alone
- 300-900mg/day (adult), 5-10mg/kg/day (child)
- Gabapentin & H1 blocker
- Gabapentin (same dose) & Cetirizine 10-20mg/day
- Gabapentin & Cetirizine (same doses) &
- Gabapentin & two H1 blockers
Cyproheptadine 4mg every 6hours - Cetirizine: 20mg/day (adult) & 10mg/day (pediatric
- Combination of H1 & H2
Cimetidine: 1200mg/day, divided by 4 (adult),
30mg/kg/day, divided by 4 (child)
Naltrexone (supplemental
25-50mg/day before sleep for 2weeks (20, 21)
pharmacological treatment)
All treatments for pre-healing stage
Ozonated oil 2drops/cm²once a day or
& Topical agents (Ozonated oil or
Hyaluronic acid gel ½ finger tip/cm²daily
Hyaluronic acid gel 0.2%)
For 12 weeks or as needed (9)
Benson muscle relaxation
Same dose as above (11)
Massage therapy applied to healed
15-30minutes, 1-3times/week for 5-12weeks
(10, 12, 29, 32)
Apply for 2weeks (8)
LLLT or regular Laser Therapy
LLLT: 2 times/week for 8weeks (13) Regular laser therapy: once per month for 6 month (19)
Once a day for 2-3weeks (14, 18, 37)
3 times/week for 1 month (35)
Silicone Gel Sheeting
Wear 12-24hours/day for 6 months (8, 23, 24)
Apply as needed (7, 15)
- Once a day for 2 weeks (22)
- Mugwort lotion
- 2 times/day for 2 months (27)
- 3 times/day for 4 weeks (26)
- 2drops/cm² once a day (9)
- Hyaluronic acid gel 0.2%
- ½finger tip/cm² daily (9)
Moisturizing body shampoo
Use as needed (30)
Apply as needed (7)
Each stage of wound healing can be managed by both non-pharmacological and
pharmacological interventions. Non-pharmacological methods are less invasive
interventions and are considered the primary intervention. On the other hand,
Pharmacological methods are more invasive interventions and are most times used as a
supplement to potentiate the effect of non-pharmacological interventions or to decrease
possible adverse effects of combination medications.
Non-pharmacological interventions are versatile and can be combined with any
other non-pharmacological interventions as well as pharmacological interventions.
Choice for non-pharmacological interventions will be considered by the facility's
resources and patients' preferences. However, only one option from pharmacological
interventions should be used with any non-pharmacological interventions only when non-
pharmacological methods are not effective. Also, single medicine can be started when
adding pharmacological methods. For example, in pre-healing stage, they can use all of
non-pharmacological methods (both massage and Benson muscle relaxation therapy) and
only one of pharmacological methods (either Pregabalin alone, Pregabalin & two
antihistamines, Gabapentin alone, Gabapentin & H1 blocker, or Gabapentin & two H1
blockers, or Combination of H1 & H2 blockers). In this case, only Pregabalin needs to
be initiated, but if Pregabalin alone does not effectively relieve pruritus two
antihistamines can be added (Figure 4). Moreover, if pruritus persists regardless of
interventions used, the following medications can be added to reduce symptoms:
Zofran® (ondansetron), Serotonin, SSRI (selective serotonin reuptake inhibitor:
Paroxetine), Doxepin® (tricyclic antidepressant), Gabapentin, Naltrexone, Topical
Antihistamines, Topical Steroid, EMLA® Cream (lidocaine 2.5% & prilocaine 2.5%),
Dothiepin (Tricyclic agent) cream, and Botox® (botulinum toxin). This post burn
pruritus relief protocol was developed after a comprehensive systematic review of the
literature with best practices identified. APNs can also use this evidence based protocol
as standardized procedure for prescriptive authority.
DISCUSSION
This protocol, the second of any post burn pruritus protocols is the first APN
driven evidence based protocol that uses non-pharmacological interventions as a primary
method of choice to reduce post burn pruritus. This protocol can be implemented in
practice by APNs or RNs depending on the choice of interventions used. In addition, this
protocol has recommended dosage and period for each intervention to clearly guide
APNs and RNs. Using the Rosswurm and Larrabee model the nurse in clinical practice
can assess the efficacy of this post burn pruritus protocol to ascertain if the protocol: 1)
relieved discomfort from pruritus; 2) lessened disturbances on daily life that can include
low concentration, agitation, anxiety, and a flat affect; 3) and increased quality of life.
The 5-D Itch Scale (Appendix A) and/or the Visual Analogue Scale (Appendix B) are
both valid and reliable and can be used before and then after the treatment method to
quantify patient outcomes. The results from this systematic literature review and the
model for implementing practice change, significantly contribute to the treatment of post
burn pruritus. Non-pharmacological and Pharmacological interventions for post burn
pruritus have been identified and presented in an easily identified protocol to improve
patient outcomes and clinical practice.
The findings of this systematic literature review and proposed protocol will help
to advance the DNP role in research and translational inquiry. This protocol will be
utilized in the future to develop interventional studies to enhance post burn pruritus
management as well as to relieve patient suffering.
REFERENCES
Ahuja, R. B., & Gupta, G. K. (2012). A four arm, double blind, randomized and placebo
controlled study of pregabalin in the management of post-burn pruritus. Burns,
39, 24-29. doi:10.1016/j.burns.2012.09.016
Ahuja, R. B., Gupta, R., Gupta, G, & Shrivastava, P. (2010). A comparative analysis of
cetirizine, gabapentin and their combination in the relief of post-burn pruritus.
Burns, 37, 203-207. doi:10.1016/j.burns.2010.06.004
Akhtar, N., & Brooks, P. (2012). The use of botulinum toxin in the management of burns
itching: Preliminary results. Burns, 38, 1119-1123.
Anand, S. (2012). Gabapentin for pruritus in palliative care. American Journal of Hospice
& Palliative Medicine, 30(2), 192-196. doi:10.1177/1049909112445464
Baker, R. A. U., Zeller, R. A., Klein, R. L., Thornton, R. J., Shuber, J. H., Marshall, R.
E., . . Latko, J. A. (2001). Burn wound itch control using H1 and H2 antagonists.
Journal of Burn Care & Rehabilitation, 22, 263-268.
Bauer, C. (2010). Evidence based practice: Demystifying the Iowa Model. Oncology
Nursing Society, 25(2), 1-8.
Bell, P. L., & Gabriel, V. (2009). Evidence based review for the treatment of post-burn
pruritus. Journal of Burn Care & Research, 30(1), 55-61.
Brooks, J. P., Malic, C. C., & Judkins, K. C. (2008). Scratching the surface: Managing
the itch associated with burns: A review of current knowledge. Burns, 34(6), 751-
760. doi:10.1016/j.burns.2007.11.015
Brooks, P., Phang, K. L., & Moazzam, A. (2007). Nanocrystalline silver (Acticoat) for
itch relief in the burns patient. Australian & New Zealand Journal of Surgery,
77(9), 797-804. doi:10.1111/j.1445-2197.2007.04233.x
Campanati, A., De Blasio, S., Giuliano, A., Ganzetti, G., Giuliodori, K., Pecora, T., . .
Offidani, A. (2013). Topical ozonated oil versus hyaluronic gel for the treatment
of partial- to full-thickness second-degree burns: A prospective, comparative,
single-blind, non-randomized, controlled clinical trial. Burns, 39, 1178-1183.
Carrougher, G. J., Martinez, E. M., McMullen, K. S., Fauerbach, J. A., Holavanahalli, R.
K., Herndon, D. N., . . Gibran, N. S. (2013). Pruritus in adult burn survivors:
Postburn prevalence and risk factors associated with increased intensity. Journal
of Burn Care & Research, 34(1), 94-101. doi:10.1097/BCR.0b013e3182644c25
Casaer, M., Kums, V., Wouters, P. J., Van den kerckhove, E., & Van den Berghe, G.
(2008). Pruritus in patients with small burn injuries. Burns, 34(2), 185-191.
Cho, Y. S., Jeon, J. H., Hong, A., Yang, H. T., Yim, H., Cho, Y. S., . . Seo, C. H.
(2014). The effect of burn rehabilitation massage therapy on hypertrophic scar
after burn: A randomized controlled trial. Burns, 40(8), 1513-1520.
Elman, S., Hynan, L. S., Gabriel, V., & Mayo, M. J. (2010). The 5-D itch scale: a new
measure of pruritus. British Journal of Dermatology, 162(3), 587-593.
Farahani, P. V., Hekmatpou, D., & Khani, S. S. (2013). Effectiveness of muscle
relaxation on pain, pruritus and vital signs of patients with burns. Iran Journal of
Critical Care Nursing, 6(2), 87-94.
Field, T., Peck, M., Hernandez-Reif, M., Krugman, S., Burman, I., & Ozment-Schenck,
L. (2000). Postburn itching, pain, and psychological symptoms are reduced with
massage therapy. Journal of Burn Care Rehabilitation, 21, 189-193.
Gaida, K., Koller, R., Isler, C., Aytekin, O., Al-Awami, M., Meissl, G., & Frey, M.
(2004). Low level laser therapy-a conservative approach to the burn scar? Burns,
30, 362-367. doi:10.1016/j.burns.2013.12.012
Goutos, I. (2010). Burns pruritus - A study of current practices in the UK. Burn, 36(1),
42-48. doi:10.1016/j.burns.2009.06.196
Goutos, I. (2013). Neuropathic mechanisms in the pathophysiology of burns pruritus:
Redefining directions for therapy and research. Journal of Burn Care & Research,
34, 82-93. doi:10.1097/BCR.0b013e3182644c44
Goutos, I., Clarke, M., Upson, C., Richardson, P. M., & Ghosh, S. J. (2010). Review of
therapeutic agents for burns pruritus and protocols for management in adult and
pediatric patients using the GRADE classification. Indian Journal of Plastic
Surgery, 43(3), 51-62. doi:10.4103/0970-0358.70721
Goutos, I., Dziewulski, P., & Richardson, P. M. (2009). Pruritus in burns: Review
article. Journal of Burn Care & Research, 30, 221–228.
Goutos, I., Eldardiri, M., Khan, A. A., Dziewulski, P., & Richardson, P. M. (2010).
Comparative evaluation of antipruritic protocols in acute burns: The emerging
value of Gabapentin in the treatment of burns pruritus. Journal of Burn Care &
Research, 31, 57-63. doi:10.1097/BCR.0b013e3181cb8ecf
Gurol, A. P., Polat, S., & Akcay, M. N. (2010). Itching, pain, and anxiety levels are
reduced with massage therapy in burned adolescents. Journal of Burn Care &
Research, 31, 429-432. doi:10.1097/BCR.0b013e3181db522c
Hettrick, H., O'Brien, K., Laznick, H., Sanchez, J., Gorga, D., Nagler, W., & Yurt, R.
(2004). Effect of transcutaneous electrical nerve stimulation for the management
of burn pruritus: a pilot study. Journal of Burn Care, 25(3), 236-240.
Holly, C. (2014). Scholarly inquiry and the DNP capstone. New York, NY: Springer.
Hultman, C. S., Edkins, R. E., Wu, C., Calvert, C. T., & Cairns, B. A. (2013).
Prospective, before-after cohort study to assess the efficacy of laser therapy on
hypertrophic burn scars. Annals of Plastic Surgery, 70(5), 521-526.
International Prospective Register of Systemic Reviews. (2009). The PRISMA statement.
University of York, the Centre for Reviews and Dissemination. Retrieved from
Jung, S. I., Seo, C. H., Jang, K., Ham, B. J., Choi, I., Kim, J., & Lee, B. C. (2009).
Efficacy of Naltrexone in the treatment of chronic refractory itching in burn
patients: Preliminary report of an open trial. Journal of Burn Care & Research,
30, 257-260. doi:10.1097/BCR.0b013e318198a282
Larrabee, J. H. (2009). Nurse to nurse: Evidence-based practice. New York: McGraw-
LaSalle, L., Rachelska, G., & Nedelec, B. (2007). Naltrexone for the management of
post-burn pruritus: A preliminary report. Burns, 34, 797-802.
Lewis, P. A., Wright, K., Webster, A., Steer, M., Rudd, M., Doubrovsky, A., & Gardner,
G. (2012). A randomized controlled pilot study comparing aqueous cream with a
beeswax and herbal oil cream in the provision of relief from postburn pruritus.
Journal of Burn Care & Research, 33, 195-200.
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P. A.,
. . Moher, D. (2009). The PRISMA statement for reporting systematic reviews
and meta-analyses of studies that evaluate healthcare interventions: explanation
and elaboration. British Medical Journal. Advance online publication.
doi:10.1136/bmj.b2700
Li-Tsang, C. W. P., Lau, J. C. M., Choi, J, Chan, C. C. C., & Jianan, L. (2006). A
prospective randomized clinical trial to investigate the effect of silicone gel
sheeting (Cica-Care) on post-traumatic hypertrophic scar among the Chinese
population. Burns, 32, 678-683. doi:10.1016/j.burns.2006.01.016
Li-Tsang, C. W. P., Zheng, Y. P., & Lau, J. C. M. (2010). A randomized clinical trial to
study the effect of silicone gel dressing and pressure therapy on posttraumatic
hypertrophic scars. Journal of Burn Care & Research, 31(3), 448-457.
Melnyk, B. M., & Fineout-Overholt, E. (2011). Evidence-based practice in nursing &
healthcare: A guide to best practice (2nd ed.). Philadelphia, PA: Lippincott
Williams & Wilkins.
Mendham, J. E. (2004). Gabapentin for the treatment of itching produced by burns and
wound healing in children: a pilot study. Burns, 30, 851-853.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items
for systemic reviews and meta-analyses: The PRISMA statement. Annals of
Internal Medicine, 151(4), 264-269. doi:10.7326/0003-4819-151-4-200908180-
Morris, V. E., Murphy, L. M., Rosenberg, M., Rosenberg, L., Holzer, C. E., & Meyer, W.
(2012). Itch assessment scale for the pediatric burn survivor. Journal of Burn
Care Research, 33, 419-24. doi:10.1097/BCR.0b013e3182372bfa
Nedelec, B., Rachelska, G., Parnell, L. K. S., & LaSalle, L. (2012). Double-Blind,
randomized, pilot study assessing the resolution of postburn pruritus. Journal of
Burn Care & Research, 33, 398-406. doi:10.1097/BCR.0b013e318233592e
Ogawa, R., Hyakusoku, H., Ogawa, K., & Nakao, C. (2007). Effectiveness of mugwort
lotion for the treatment of post-burn hypertrophic scars. Journal of Plastic,
Reconstructive & Aesthetic Surgery, 61, 210-236. doi:10.1016/j.bjps.2007.10.032
Otene C. I., & Onumaegbu, O. O. (2013). Post-burn pruritus: need for standardization of
care in Nigeria. Annals of Burns & Fire Disasters, 26(2), 63-67.
Parnell, L. K., Nedelec, B., Rachelska, G., & LaSalle, L. (2012). Assessment of pruritus
characteristics and impact on burn survivors. Journal of Burn Care & Research,
33(3), 407-418. doi:10.1097/BCR.0b013e318239d206
Pfab, F., Schalocks, P. C., Napadow, V., Athanasiadis, G. I., Yosipovitch, G., & Ring, J.
(2013). Complementary integrative approach for treating pruritus. Dermatologic
Therapy, 26, 149-156. doi:10.1111/dth.12031
Ratcliff, S. L., Brown, A., Rosenberg, L., Rosenberg, M., Robert, R. S., Cuervo, L. J., . .
Meyer III, W. J (2005). The effectiveness of a pain and anxiety protocol to treat
the acute pediatric burn patients. Burns, 32, 554-562.
Richardson, C., Upton, D., & Rippon, M. (2014). Treatment for wound pruritus following
burns. Journal of Wound Care, 23(5), 227-233. doi:10.12968/jowc.2014.23.5.227
Roh, Y. S., Cho, H., Oh, J. O., & Yoon, C. J. (2007). Effects of skin rehabilitation
massage therapy on pruritus, skin status, and depression in burn survivors.
Journal of Korean Academy of Nursing, 37(2), 221-226.
Rosswurm, M. A., & Larrabee, J. H. (1999). A model for change to evidence-based
practice [Abstract]. Image – The Journal of Nursing Scholarship Abstracts, 31(4),
Rowley-Conwy, G. (2014). Management of major burns: rehabilitation and recovery.
Nursing Standard, 28(25), 65-70. doi:10.7748/ns2014.02.28.25.65.e7723
Upton, D., Penn, F., Richardson, C., & Rippon, M. (2014). Psychological management of
wound pruritus. Journal of Wound Care, 23(6), 291-299.
Waked, I. S., Nagib, S. H., & Ashm, H. N. (2013). Triamcinolone acetonide
phonophoresis versus transcutaneous electrical nerve stimulation in the treatment
of post-burn pruritus – a randomized controlled study. Indian Journal of
Physiotherapy & Occupational therapy, 7(2), 87-92. doi:10.5958/j.0973-
Warner, P. M., Coffee, T. L., & Yowler, C. J. (2014). Outpatient burn management.
Surgical Clinics of North America, 94, 879-892. doi:10.1016/j.suc.2014.05.009
Whitaker, C. (2001). The use of TENS for pruritus relief in the burns patient: An
individual case report. Journal of Burn Care & Rehabilitation, 22, 274-276.
Zachariah, J. R., Rao, A. L., Prabha, R., Gupta, A. K., Paul, M. K., & Lamba, S. (2011).
Post burn pruritus-A review of current treatment options. Burns, 38, 621-629.
APPENDIX A
5 –D ITCH SCALE
(Adapted from Elman, Hyman, Gabriel, & Mayo, 2010)
APPENDIX B
VISUAL ANALOGUE SCALE
(Adapted from Elman et al., 2010)
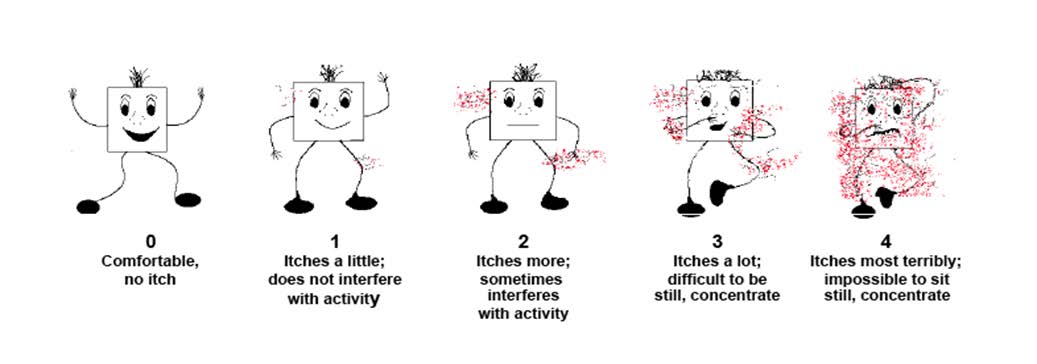
APPENDIX C
ITCH MAN SCALE
(Adapted from Morris et al., 2012)
APPENDIX D
TABLE OF EVIDENCE FOR PROPOSAL
Summary of Studies Including Pruritus in Burn Patients
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
4 groups divided from A to
For mild itching pts (VAS 2-5):
Pregabalin alone &
outpatients from
D. They were asked at 3, 7,
combined antihistamine
the department of 14, 21, 28 days after tx
B & D group showed 77.5% & 23.3%
w/pregabalin showed
To compare the Key variables: Burns & Plastic
regarding VAS scores
of remission of itching, respectively on
significant effect in
decreasing itching
All groups received
B & D group showed 100% & 96.7% of
remission of itching, respectively on
A: Antihistamine (cetirizine 28days after tx
antihistamines does not
+ pheniramine) use
seem to be beneficial to
B: Combination of
For moderate itching pts (VAS 6-8):
decrease pruritus
antihistamine & pregabalin
60yrs, TBSA >
C: Placebo (Vitamin B) use
B & D group showed 64.8% & 61.4%
Also, massage therapy
D: Pregabalin use
of remission of itching, respectively on
effectiveness within 2-
2nd degree burns,
B & D group showed 92.6% & 92.8%
4wks after tx that
of remission of itching, respectively on
showed it can be used
10mg QD or bid + 25mg
as adjunctive tx
epithelialized) or
healed < 3month
B: Pregabalin + Cetirizine
For severe itching pts (VAS: 9-10):
Limits: the study did
not define end point of
75 mg bid, tid, or 150mg
B & D group showed 56.9% & 52.7%
anti-pruritic therapy
of remission of itching, respectively on
C: Vitamin B 1 capsule
Both B & D group showed 78.9% of
QD, bid or 2 capsules bid remission of itching on 28days after tx.
D: Pregabalin 75mg bid,
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
tid, or 150mg bid
GA – cetirizine tx only
GA: pruritus reduction in 52%
GB – gabapentin tx only
GB: pruritus reduction in 95%
centrally acting drugs &
patients per each
GC – gabapentin &
GC: pruritus reduction in 94%
peripherally acting
drugs did not show
Onset of action with gabapentin
better effect in reducing
cetirizine tx, &
VAS used for antipruritic
significantly faster than the cetirizine:
PB pruritus compared
effect at baseline, 3, 7, 14,
32% in GA vs 74% in GB on the 3rd
to using centrally acting
21, & 28days after tx for
day of the treatment
drugs (gabapentin)
Different drug dose used
Need for larger sample
based on the VAS (2-5, 6-8,
size to generalize,
> 1% graft were
cetirizine tx in
IC:12–70yrs old,
Limited period of data
burn area > 5%
Single site study
suggested PB pruritus
relief protocol and the
epithelialized or
gabapentin in the future
completely < 1 month back
10 pts who failed
During the study, only 8 pts All 8pts stated severe itching before tx – Botox can successfully
included due to 2 pts
2pts10/10, 1 pt-9/10, 4 pts-8/10, 1pt-
be used to treat PB
excluded for language
pruritus that is resistant
barrier & not a burn scar.
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
Key variables: therapies
All 8 pts described symptoms as "0" out therapies
(silicone gel tx,
F/u done before tx, 1wk,
of 10 at 2wks after tx
2wks after tx and b/w3-
23months after tx.
Three pts labeled the score as 1, 2, & 3
at 6, 4, & 3 months after tx
VAS used to assess itching
5 others had no itching since 2wks after
:11.3 months f/u
period. 2-3rd degree burns All scarred areas
Reviewed studies Classification of pruritus:
Gabapentin is safe & effective in uremic Well-designed placebo-
regarding use of
pruritus, cancer/hematologic causes,
controlled randomized
(prurioreceptive), central
opioid-induced itch, brachioradial
trials are needed to
effectiveness of Key variables: pruritus (cause,
(neuropathic, neurogenic,
pruritus, burns pruritus, & pruritus of
show the effectiveness
of gabapentin in
& classification
pruritus not responsive
Causes of pruritus: uremic,
Recommended doses:
to other modalities of tx
cancer (solid tumors or
Uremic pruritus-100mg after each HD,
hematologic), opioid-
Opioid-induced itch-1200mg before
induced, cholestasis,
spinal anesthesia w/morphine use
brachioradial, burns r/t itch
Started w/32 pts,
A1: Cetirizine + Cimetidine During days 1-16, no significant
Use as scheduled meds
differences b/w A1 (A1B1, A1B2) &
instead of prn meds to
A2 (A2B1, A2B2) even with some
Key variables: study
B1: Revive lotion
improvement in both tx
B2: Corrective concepts
Each group had 4tx options
During days 1-4, A1 had significant
(A1B1, A1B2, A2B1,
improvement compared to A2
A2B2) in different time
different period
frame of 1-4, 5-8, 9-12, &
During days 5-16, no significant
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
differences b/w A1 &A2 possibly from
the residual effect of previously used tx
Pts completed itch score
(VAS) before tx, at 1, 6, &
Also, no difference b/w B1 & B2 noted.
12hr intervals after tx
Class II: studies where
Pharmacologic methods (w/ specific
The study suggested tx
certainly reliable data are
dose) below decreased PB pruritus
plan according to TBSA
collected (observational
studies, cohort studies,
Selective antihistamine antagonists
To all PB pruritus;
prevalence studies & case-
(cetirizine/cimetidine) in adult &
Moisturizing cream,
control studies)
pediatric population,
Atarax in adult population,
Specified b/w TBSA
Class III: evidence
Gabapentin in pediatric population,
<10% & >10%
provided by clinical series,
Colloidal Oatmeal (topical) in adults,
comparative studies, case
& EMLA (topical) in pediatric
reviews, case reports, &
Non-pharmacologic methods decreased
The classified literature was PB pruritus significantly; determined to support
Pulsed dye laser in adult & pediatric pts,
guideline status as outlined
Silicone gel sheeting in adult &
by the Practice Guideline
for Burn care 2006
Massage in adult population,
& TENS in adult population
VAS used for itching
(Brooks, Malic, Literature
Current standard tx: oral antihistamines
Literature evidence on PB pruritus tx:
1.Combination of colloidal oatmeal &
paraffin bath emollient + antihistamines
2.Combination of different
antihistamines 3.Combination of H1
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
&H2 antagonists 4.Gabapentin use
5.TENS, massage tx, Laser tx, Unna
boot, Doxepin cream, EMLA cream,
silicone gel sheets, Acticoat dressing.
Algorithm for PB pruritus management
suggested w/ 4 steps
(Brooks,
5 subjects w/ 7,
Acticoat applied for 2 wks
VAS score: 7.4 before tx decreased to
and the intervals from
3.1 after tx (p = 0.0022).
This report did not
Key variables: 65% of TBSA
original injury to
indicate the condition of
application were 2, 3, 3, 6,
Ex) Pt w/ excoriation of the skin due to
wounds whether they
itching showed absence of excoriation
following acticoat tx
unhealed. However, it is
Before & after 2 wks of
assumed they were
outpatient clinic
application, VAS assessed
unhealed or in the
healing process because
acticoat is used for
unhealed wounds in
current practice
patients
(Campanati et
30 pts w/partial
Pts applied ozonated oil on
Ozonated oil had the same efficacy of
Limit: lack of a
to full thickness
half of the burn lesion and
hyaluronic acid in reducing symptoms
histological comparison
2nd degree burns
hyaluronic acid on the other r/t burns (erythema, tension, height,
half of the lesion once a
itching & burning sensation) after 12
wks of topical application
and controlled 01/2012
Ozonated oil was more effective than
Clinical features of each
hyaluronic acid in preventing post-
Key variables: stage of re-
lesion (erythema, tension,
lesional hyperpigmentation
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
height, itching & burning
comparing with hyaluronic
sensation) assessed w/
IVCP at baseline, 6monthes
& 12 months after tx.
scars, photo type
> III, allergy or
Pts completed survey
intolerance to the
focusing on "what part of
the treated lesion had
improves more?", which
thyroid diseases,
topical tx is more
comfortable?", & "what tx
corticosteroid or
Burn patient age
G1(w/in 24months PB
More than 73% of adult burn survivors
suffered from pruritus episodes during
Questionnaire for burn r/t
the first 2 yrs following injury;
responses regarding
study (N = 930).
pruritus provided at D/C, 6,
wound condition d/t
12 & 24 months PB
In 75.7% of long-term burn survivors,
self-report based data &
Key variables: patients injured
pruritus existed <6hrs/ day from mild to
no P/E information;
G2 (over 2yrs PB injury):
moderate for the intensity;
Limited control ability
2010. –no more
2-yr f/u & long-term f/u in
for question variability
5yrs (172subjects) & in
In more than ½ of long-term burn
& question confusion
10yrs (164subjects) PB
survivor, pruritus still impacted their
d/t various data
leisure, household, vocational activities
collection methods;
No current tx method
43 out of 930subjects in
for PB attained;
provided 5 or 10
common to both G1 & G2
Predictors of PB pruritus include female
Future study needed to
gender, younger age, %TBSA-burn,
assess tx methods for
Group 2 (LTF) – f/u at 5
depth of injury, %TBSA grafted, dry
&10 yrs after burn injury &
skin, & thick or raised scars;
43 subjects completed from
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
care facility at
No differences in PB pruritus noted
Note: Since the data
D/C & thereafter
regarding ethnicity/race, scar
collection method was
discoloration, & open/closed wounds
self-report only,
experts' objective data,
especially for wounds are needed
Questionnaire was made in
No difference in time b/w injury &
First study on pruritus
patients treated in Dutch w/ collaboration of a
interview in patients reporting pruritus
in a large population
Retrospective, the university of
burn surgeon, a child
& no pruritus (P = 0.3);
w/small burns (TBSA
psychiatrist, a registered
Similar pruritus incidence obtained
nurse, a specialized
from patients or a relative (P = 0.2)
Injury Clinic in
physiotherapist & an
intensive care physician (no Pruritus incidence 50%;
High P values for the
detail info on the
¼ of the moderate pruritus group had
info obtained methods
%TBSA-burn, A relative who
questionnaire noted)
negative impact on daily life (P =
& the time b/w injury &
lived in the same
.0002) & sleep pattern (P = .002)
factors in small
Questionnaire is not
Patients had less pruritus when the age
psychometrically
at burn injury was < than 2yrs, %TBSA-
validated, not age
burn was < 2%, & wound healing was <
3 weeks, but more pruritus when the
specified in races,
burn areas were trunk or lower limbs
opioid intake & burn
(P<0.001)
Age < 50yrs & %TBSA-burn had
Notes: Further studies
expectation for severe pruritus in
needed for impact on
QoL, development of
pathologic scarring,
Half of patient having pruritus received
early consultation in the
treatment & 25% of them reported
plastic surgery clinic, a
distinct effect; No association b/w
formal referral to
wearing of garments & application of
general practitioner f/u,
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
& a preventive tx
Before & after massage
No significant differences b/w EG &
Burn massage therapy
therapy, EG & CG assessed CG for gender, age, TBSA, interval b/w
burn injury & rehabilitation therapy,
Key variables: scars after acute
pain(VAS), Pruritus, &
period of rehabilitation therapy, VAS,
pruritus, & scar
Scar characteristics
pruritus, & scar characteristics before
characteristics in
(thickness, melanin,
hypertrophic scars after
erythema, TEWL, sebum,
elasticity) b/w 2 groups
Results after burn rehabilitation
massage therapy;
standard therapy
Measurement tools:
EG showed significant improvement in
Massage given only for
Thickness, melanin &
pain, itching, scar thickness
short period (average:
erythema, TEWL, sebum,
(↓thickness), melanin (↓melanin),
34.7days), so long-term
& elasticity assessed by
erythema (↓erythema), scar TEWL
effects not identified.
(↓TEWL), & sebum (↑sebum)
in addition to the
Tewameter, Sebumeter, &
hypertrophic scar not
Cutometer, respectively
However, for scar elasticity, EG showed considered
significant improvement only in
Future study
Burn rehabilitation massage immediate distension & gross skin
therapy given 30min a day
for 3times a week, average
12.5 times by specialized
burn rehabilitation massage
Demographic info obtained. Muscle relaxation technique is effective
Pain VAS, Pruritus
in relieving the pain, pruritus & v/s of
No explanation for
hospitalized 2nd
assessment scale, & v/s
pts suffering from burns. Its use as a
other methods to reduce
degree burn pts,
assessed before & after 20
therapeutic & alleviative method to be
pain or pruritus used or
min Benson relaxation
suggested for patients suffering from
allocated to case
method to control group. A
No explanation of
& control groups. month later, these 4
frequency of relaxation
assessments performed
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
group: control &
before & after 20 min
Benson verbal & muscle
relaxation technique to case
hospital in Iran
Chi-square, independent t-
test, paired t-test & Mann-Whitney test were used
CG received standard
There was significant reduction in
itching, pain, depression & anxiety in
significantly decreased
Key variables: (EG:10, CG:10)
EG received standard
medical care & massage
depression & anxiety in
Inclusion criteria: therapy on the wound for
PB population w/
A closed, oderate 30min, twice a week for
c/o severe itching After massage therapy,
Limits: needs larger
Itching, pain, depression &
sample & long term use
anxiety compared b/w two
of massage therapy
VAS used for itching
VSS (for ht, pliability,
17 out of 19 lesions showed
Selecting other side of
pigmentation & vascularity
macroscopic improvement while 2
skin in the same pt is
of scar), VAS (for pruritus
lesions did not improve.
possible weakness of
All pts suffered
& pain), digital
:Scar < 12months improved better than
Key variables: from burn scars
scar > 12months
before the study
macroscopic evaluation
Need more studies that
and none of them
were performed before &
LLLT demonstrated improvement in
have higher number of
pain & pruritus among 19 PB
sample and control site
from different people
corticosteroids,
rather than the same
group w/ different sites
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
excision before LLLT In each pt, 1 burn scar was given by LLLT & 1 similar burn scar was defined as a control area(no tx)
Phone questionnaire
The median of postburn pruritus is 80%
The first study to
specialists from
distributed to inquire burn
explore the knowledge
22 burn units in
relevant pruritus
on burn pruritus among
Key variables: the UK
(12 questions in
21 burn units (95.45%) have no daily
physicians, reporting a
assessment on pruritus in a quantitative
lack of consensus on
manner; 1unit uses Itch Man Scale on a
Protocols for burn
1. % of burn patients
12 units (54.55%) reported more intense pruritus needed;
affected by pruritus,
pruritus in the evening;
The reasons for lack of
2. differences in adult &
34.36%, 34.09% & 20.45% felt more
protocols include low
pediatric burn patients for
pruritus during the wound healing,
remodeling & acute phase, respectively;
3. assessment tool
40.91% felt more pruritus in superficial
consideration of pt
availability for pruritus in
partial thickness burns;
preferences, & poor
pt daily care plans,
40.91% & 31.82% felt more pruritus in
resource allocation
4. diurnal variation of
wounds treated w/ dressings & w/grafts,
January, 2008 –
5. effect stage of healing &
90.91% used antihistamines as a 1st line
Low Sample size.
for pruritus:1unit used ondansetron, &
6. effect of burn depth &
3units used gabapentin alone or with an
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
pruritus, healing method &
5 units used additional pruritic relief
The study showed
methods: 2 units utilized psychologists,
relevant research
pharmacological agents,
other 2 units used massage therapy, & 1
according to question
other supplement in
used silicone products for pruritic
contents & suggested
pruritus management,
more research on each
8. protocols in postburn
Only one unit has a specified protocol
content to relieve
pruritus in the unit
for pruritus management
PB Pruritus lasts longer than wound
Neuropathic element is
healing period (inflammatory,
cause of PB Pruritus
proliferative, & remodeling phase)
and neuropeptide-
mediated selective
Pruritus classification (by Twycross et
hyper innervation
Pruritoceptive, Neuropathic,
excitement to develop
Neurogenic, & Psychogenic pruritus)
longstanding symptoms
Aggressive antihistamine is effective in
the early phase, but in the later stages
Needs more study
wounds appear to be less effective to
antihistamine therapy
Evidence from the effectiveness of
therapeutic approaches acting on the
Gabapentin-persistent therapeutic effect
of gabapentin is due to the ability of
preventing CNS sensitization
Ondansetron-more effective than antihistamine. Serotonin- antihistamine effect
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
TENS-effective in remodeling phase
Multidisciplinary approach is needed in
The study advocates the
successful assessment & treatment.
early employment of
centrally acting agents
Key variables: agents in the
Employment of a tool to assess severity
& peripherally acting
Pruritus, burn, burns literature
of pruritus is critical because sever
agents as well as non-
pruritus needs a combination of agents-
Itch man scale is recommended for burn
interventions for the tx
Use of topical emollients & cooling
agents is included in the protocol due to
positive clinical experience even w/o
supportive studies
classification to
Agents acting on the central part of the
pruritic pathway-gabapentin, ondasetron
Agents acting on the peripheral part of
the pruritic pathway-H1 partial agonist
& H2 receptor antagonist Non-pharmacological adjunct-TENS, laser, pressure garment, massage therapy
Therapeutic strategies are classified by
interventions on peripheral & central
aspects of the pruritic pathway
Peripheral aspects: cooling of the
wound, antihistamines, topical Doxepin,
local anesthetics, colloidal oatmeal,
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
Capsaicin, Laser tx, Aloe Vera, topical
Dapsone, Unna boot, Compression
garments, Ondansteron
Central aspects: Gabapentin, TENS, Massage therapy, Psychological support
Study #1 & #2 pts assessed
Antipruritic monotherapy in acute
Gabapentin is more
50 PB pts applied for pruritic symptoms using burns: gabapentin monotherapy had 4
"itch man scale" & VAS
times more effective than
monotherapy by acting
chlorpheniramine tx (41.46% vs 10%)
directly on the central
Antipruritic Polytherapy in acute burns:
Combination of gabapentin, cetirizine,
It is important to use
41 PB pts applied 1: little itch not interfering
& cyproheptadine was more effective
Key variables: to revised St.
than combination of 3 antihistamines
peripheral aspects of the
2: more itch sometimes
(chlorpheniramine, hydroxyzine, &
pruritic pathway in
interfering w/activity
cyproheptadine) in symptomatic relief
managing burns itching
3: a lot of itch, which
of pruritus in PB population
antihistamines EC: burn
makes lying still &
concentration difficulty
Needs further studies
4: most terrible itch making
Factors for failure in monotherapy are
incorporating long term
hypersensitivity
it impossible to sit still &
younger age and larger TBSA
f/u of comparing
peripherally & centrally
Pts w/ higher initial itch scores needed
acting agents in late
more pharmacologic escalation
hepatic impairment
(Gu¨rol, Polat,
EG showed significant improvement in
Limits: small sample
admitted for burn Demographically & burn
reducing itching, pain, & anxiety
characteristically no
compared to CG (p < 0.001)
The study did not
Key variables: university
differences b/w EG & CG
specify the condition of
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
wound whether it is
2/2008 to 6/2009
EG got 15minute massage
healed or not. – it is
tx 2x/wk for 5wks as well
assumed that not all
as standard care
wound are healed
2nd or 3rd degree
according to the fact
pain, itching, &
Massage tx done by trained
some pts were getting
massage therapists, applied
standard tx including
to healthy skin around the
pain & they were
wounds & surface of
enrolled in the study
right after admission
Itching rating, VAS for pain, & STAI assessed on the 1st day & last day of 5-wk study period
VAS used by sample before TENS significantly reduced PB pruritus
& after tx and data were
in the population sampled
generalized to children
standard of care.
compared b/w 2 groups
<18 or pts> 75yrs of
Therefore, TENS should be considered
received standard
as a tx option for burn survivors whose
The mode of TENS was
quality of life is negatively affected by
high frequency & low-
7days per wk for
Additional parameters
for TENS need to be
IC: age of 18-75
w/ partial or full-
thickness burns,
proliferative stage of
>5, remodeling
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
phase of wd healing w/ recent re-epithelialization. EC: pregnancy, hx of epilepsy, pacemaker
Sample: mean age-26.9,
Within the 12months of the study
mean TBSA-16.1%,
period, VSS & UNC4P (pain, pruritus,
1.unaware of long-term
average 2.8sessions/pt,
pliability, & paresthesia) decreased (P <
including pulsed dye laser
2.not specified in scar
& CO2 laser at 16months
Key variables: treated at the
(median) & 48months
3.evaluator bias not
effects of laser
(mean) after burn injury.
VSS & UNC scar scale
4.no control group
assessed right before the
5.order of different
first session, 4-6wks later,
lasers not examined
& at the time of the next
Recommendation: RCT w/ long-term period & objective data (elasticity, hardness, & redness) & subjective data (QoL)
Retrospective, 19 pts treated for
Total 19pts (9-treated
14 pts reported improvement in
Not sure of naltrexone
w/antihistamine only, 9-
experience of itching & 5 pts reported
as the first line of PB
w/antihistamine &
no change in itching
pruritus, but the study
gabapentin, 1-w/gabapentin
suggests naltrexone
Key variables: Hangyang Sacred only) who are dissatisfied
44.5% (9pts) reported ↓ scratching
warrants further studies
Heart Hospital in
w/ current tx received
using RCT to examine
naltrexone for 2wks.
its potential role as a tx
After 2wks, participants
However, 7 pts reported side effects
for chronic itching in
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
answered for itching on
(headaches, nausea, vomiting, &
abdominal cramps).
w/retrospective rating of
the severity of itching.
No laboratory tests after tx noted
(Tx: began w/25mg, then ↑
to 50mg the following day)
15 pts who traditionally
Participants demonstrated some
treated w/antihistamines
satisfaction of Naltrexone use in
Need a larger sample,
traditional tx for
(H1 or H2 receptor
reducing PB pruritus;
Key variables: PB pruritus.
antagonist) & hydrating
measurement of itch
lotion, but still w/ pruritus
Overall, 50% (4pts) improved regarding
recruited for naltrexone tx-
frequency & duration of itching
qualification of
1pt dropped for allergic
according to Frech-Canadian VAS
scratching activity,
reaction, 1pt dropped for
recruitment of a broader
intolerable dizziness
range of burn pts, long
Regarding additional 6 questions,
term f/u, & a placebo
8 pts completed French-
72% (9pts) satisfied with the itch relief
controlled tx group
Canadian version of the
provided by naltrexone
itch VAS before tx & 2wks
62% (8pts) stated that QoL improved
after naltrexone tx, then compared the result. 5pts completed only after tx All pts answered 6 additional questions regarding naltrexone, too
Components of Medilixir-
1.Medilixir reduced itch after
Medilixir is more
coconut, palm, castor,
application more frequently than
effective to minimize
olive, hemp seed, wheat
PB pruritus than
germ, & canola seed oil
2.By using Medilixir, pts felt itch
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
Key variables: Mean
recurrence later than CG w/tx of
Components of aqueous
Limits: small sample
cream- paraffin, heavy
3.EG required less antipruritic
liquid, phenoxyethanol, &
medications than CG did
direct admission,
Meaning: a larger size
study can be warranted
No significant difference in
any demographics
Mean time in seconds
required for cream
application & mean days
before the 1st cream
application b/w two groups
not significantly different.
VAS used for itching
Spectrocolorimeter &
EG showed significant improvement
The study indicated that
w/ post-traumatic TUPS used for
regarding scar thickness & scar
silicone gel sheeting
pigmentation measurement
was effective to reduce
thickness, pain,
Vancouver Scar Scale for
For scar pigmentation, pain & itching,
itchiness, & pliability of
Post traumatic EG (24pts) wore
the scar thickness
EG showed better outcomes but not
the severe hypertrophic
scar among the Chinese
day and received
15minute lanolin
VAS used for pain &
Moisturization effect of
the scar twice a
the tough & hard scar
day for 6months.
Digital image of each scar
may contribute to the
was recorded by using a
reduction of the skin
thickness after 6 months
only massage for
‘s intervention
Two-way repeated
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
ANOVA used to analyze
Limit: population is
above 4 measures &
limited to Chinese
Turkey test for post hoc
people- generalization
to long traveling
comparison analysis used
for difference over time(2
Small size of sample
& 6months after beginning)
Study had only 16 burn scars out of 45 scars – can be applied to specifically to burn scar pts?
4 groups of PG (n=30),
Scar Thickness: CTG showed
SGS (n=24), combined w/
significant improvement at 2, 4, 6
showed significant
PG & SGS (CTG, n=29), & months after tx. PG showed significant
improvement in scar
Jiangsu People's
control group (CG, n=21)
improvement 6 months after tx.
thickness after 6months
First Affiliated
Drip-out: 20 pts
Scar Pigmentation: CTG showed more
4 groups assessed before, 2, improvement than other groups & all
4, & 6months after
other groups showed significant
SGS showed more
improvement regarding pigmentation
effective in decreasing
pain and pruritus than
Assessment tools:
the scar thickness
Subjective feedback from
Scar Pliability: significant improvement
pts regarding their
in all groups showed at each
Limits: high drop-rate
perception on the scar
assessment. CTG had the most
injuries, & scar <
condition (cosmesis, pain,
improvement in softness of scar among
& pruritus) by VAS.
all groups at 2 & 4 months after tx
Objective tools for scar-
spectrocolorimeter (for
Pain: 3 EG showed significantly less
color), TUPS (for
pain over time & CTG & PG had
thickness), & VSS (for
significant effect on pain
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
Pruritus: all groups reported
VSS > 5 & each
significantly less itchy but SGS seemed
better result (no significance)
Questionnaires were
Itching complaints at 3months, 1yr &
The study shows the
completed by PB pts at
2yrs PB show 87%, 70% & 67%,
necessity to approach
3months, 1yr, & 2yrs after
itching from multiple
perspectives, such as
The frequency of moderate to severe
psychological state of
Key variables: Netherlands &
The questionnaire has a 7-
itching is 34% & 23% at 1 & 2 yrs PB,
pts, because chronic
point Likert scale for
itching occurs in a
itching & the Impact of
group of different
Event Scale (IES) for
Risk factors for itching are surgical
operations, PTS, gender (F>M) &
symptoms of PTSD
Limit: the questionnaire
of the study is based on
However, TBSA is not a factor at 1 &
a single question.
2yrs PB & gender is not a factor at 2yrs
Answers were scored
differently from VAS/
The study excluded pts
In conclusion, PTS symptoms &
surgical operations (more grafted skin)
psychiatric problems.
are risk factors for itching at 2yrs PB
The study may underestimate the prevalence rate of itching
Gabapentin given starting
Nurses and parents reported a
Total 35 children
as 5mg/kg tid. & maximum
remarkable reduction in itching &
behavioral difficulties,
dose up to 5mg/kg bid &
antihistamine intake was decreased or
the tx needs to be
Key variables: 23≤3yrs).
10mg/kg at night.
3 out of 23 kids
having skin loss
from meningitis.
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
-maximum dose for
One child w/ ADHD showed disruptive
RCTs are necessary
epilepsy:40mg/kg/day
behavior as a side effect-only one case
chlorpheniramine Parents & nursing staff
assessed the effects of the
tx (gabapentin use)
remained irritable & constantly rubbing wounds
A total of 23 post Duration, frequency, &
Duration of itch episodes in minutes at
numbers of itch episode per
baseline & wks 1, 2, 3, & 4. Tx group
significantly reduced
who were itching
day, itch TBSA & affective
has shown significantly reduced
burn associated pruritus
from burn injury
itch characteristics
duration of pruritus compared to the
compared to using other
treated in Villa
measured at baseline, 1,2,3,
& 4th wk after tx b/t control
Frequency of itch was described as the
number of days a wk at baseline, wks 1,
Small pilot study, single
- 12 for tx group,
4 Measurement used:
2, 3, & 4 showed that tx group had
center & convenience
Description of Pruritus
significantly low frequency at wks 2,3,
population, short period
Experienced During
& 4 compared to the control group
of data collection
Previous Week for
Duration of episode –
Number of daily itch episodes was
classification b/w acute
<5, ≥5 & <30, ≥30 & <60,
significantly lower in the tx group
& chronic pruritus in
compared to the control group at wk 2
post burn population
IC: experiencing
Daily frequency –
after the treatment
postburn pruritus
Wkly frequency –
Itch TBSA measurement over time for
tx & control groups: Tx group had
Questionnaire for Pruritus
significantly smaller itch TBSA
compared to the control group at wks 1,
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
Modified Vancouver Scar
lasting more than
Scale; Mexameter
Presence or absence of affective itch
characteristics: Tx group significantly
Descriptive statistics & a
felt less bothersome from burn
epithelialized test Wilcoxon rank-sum test
associated pruritus at wks 1, 2, 3, & 4,
area, &18 yrs or
less annoyed at wks 4, & less
unbearable from pruritus at wks 2, 3, & 4 compared to the control group
15 pts (M5, F10;
15pts received mugwort
No significant improvement after 1 wk
Mugwort lotion is
24-74yrs old) w/
lotion twice a day, then 1
effective for improving
wk later survey completed.
subjective symptoms
Key variables: scars who
; one pt was dropped for a
Significant improvement in pruritus,
suffered from 2nd
cold sensation to the site of
sleep disturbance & redness noted
2months after tx (P = 0.027)
Need to continue to
treating the itch scars
2 months after the same tx,
evaluate effects &
14 pts completed survey
mechanism of mugwort.
regarding improvement of
Need to conduct more
studies to evaluate this
Study subjects answered
Q1: 54.3%(night), 28.6% (afternoon),
Itch man scale (0-4)
attended for 5day for: Q1. Time of the day
2.9% (no difference), 14.3% (no
when itching is most
assessment tool for
Q2: 34.3% (kids), 25.7% (adults),
pruritus & anti-pruritus
Q2. Ages of experiencing
25.7%(no difference), 14.3% (no
regimen to be applied
more itch (adults or kids),
according to the scale
Q3. Itch assessment tools
Q3: 88.6% (no assessment tool to use),
Q4. Types of burns resulted 11.4% (vague methods used)
joint scientific
in the greatest levels of
Q4: 37.1% (deep dermal burns), 20%
The recommendation
burn specialists
(partial thickness burns), 17.1% (full
needs to be supported
Q5. Treatment methods,
thickness burns), 11.4% (full thickness
by evidence based
Goutos (2010) general meetings
usage of any form of anti-
& deep dermal burns), 2.9% (partial
research. Sample size
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
pruritic regimen
thickness & deep dermal burns), 11.4%
too small & limited to a
(no answer). 85.7% (conservative tx >
country (Nigeria) to
generalize to the world
Q5: 57.1% (oral meds), 22.9% (
Injections), 8.6% (topical agents),
5.7% (reassure pts), 5.7% (combination
Surgeons and the
of oral & topical agents). 85.7% (no any
form of anti-pruritic regimen).
23 subjects aged
Demographic findings:
Frequency if pruritus:
daily (87%) & 2-3x/wk (96%). Duration characterize nonstop PB
PB pruritus with
of pruritus per incidence: 5-30 minutes
Mean years postburn
(52%)-No significant difference b/w
Pruritus reported as
(0.95), Range (0.1-3.21),
acute & chronic pruritus groups
unbearable, bothersome
Mean burn % TBSA
Description of accompanying Sensation: & annoying;
(35.35), Mean pruritus
Stinging (74%), pinching (48%),
Acute group reported
%TBSA (6.22)-1 subject
more severe pruritus &
Crawling & burning pruritus sensation
it possibly expects that
were perceived as more severe in spite
patients recover,
Scales & questionnaires in
of low frequencies
improve coping skills &
English & French; pain,
Affective aspects of pruritus:
experience w/pruritus &
pruritus, & QoL scales
Unbearable (91%), bothersome (91%),
scar maturation over
Parameter for acute pruritus Acute group has less pruritus episodes
Acute pruritus group
& chronic pruritus d/f as
but more influence from the pruritus
persistent pruritus in PB
than chronic group
pruritoceptive pruritus
subjects: PB 6months
Mean VAS Scores for Itch: 2.65. Worst
whereas chronic group
pruritus score: 7 (acute group) & 9.07
Primary variable analyzed
neuropathic pruritus.
as a single category
Best score for pruritus: 1.38
Therefore pruritic
There was a significant difference
treatment can be more
between the pruritus & pain sensations
effective when pruritus
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
A severity index for
(general pain, P = .0003; local pain, P =
characteristics are
sensation was calculated by
Sleep problems associated with pruritus
Pruritus triggering &
were not significantly reported
relieving QoL activities
Pruritus caused low concentration (N =
reported, which can be
8), agitation (8), anxiety (4) & no
applied to teach burn
change in the mood (6)
survivors to reduce
Pruritus triggering QoL activities were
pruritus episodes
dryness(83%), heat(70%),
Limitations: ↓ power
fatigue(57%), physical effort(52%), &
analysis d/t ↓sample
special fabric(48%)
Cold temperature (30%), cold water
Acute pruritus period is
(26%) & rest (22%) were pruritus
relieving activities
The age of burn scars
Sleep, lying down, sitting, eating & hot
water did not affect pruritus.
Regulating the central
The severity scores of pruritus b/w scars sensitivity of pruritus were similar
explored incompletely-
The natural lubrication of the skin b/w
pruritus mechanisms &
acute & chronic group was similar, but
tx to be more studied
acute pruritus scars have more rough
skin texture & higher mean level of
Needs more pts from
erythema despite no significant
various areas, races,
differences b/w groups
TBSA, & time after burn & research period
to ↑ for generalizability
The article addressed CAM
Regarding pruritus in burns, 15 minute
This result is written
application and its
massage therapy twice a week over
just per two other
effectiveness for atopic
5weeks reduced itching, pain, & anxiety
articles that are
dermatitis, chronic
levels in burn adolescents
included in the project
urticaria, uremic itch,
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
postoperative itch, pruritus
in burns, & intractable
neuropathic itch
mechanisms, & acupuncture, clinical
treating pruritus w/ CAM techniques (Ratcliff et al.,
The review done in terms
Findings only Relevant to itching
Itching in children
of pain medication &
TBSA, pain scales & age,
considerable problem
medication given for
Performed per itching management as
and involves both
effectiveness of pain, burn,
PTSD, anxiety, itch &
grafted & non-grafted
procedural pain, anxiety
For itching > 2 of 4, give
skin at a prevalence of
medication & TBSA, and
1) Moisturizing body shampoo &
up to 100% for the
itch medication & TBSA
lotions, topical ointments (not
hydrocortisone creams)
The review divided into 3
2) Diphenhydramine
Diphenhydramine was
groups according to ages:
1.25mg/kg/dose po Q 6h
effective as a primary
<3, ≥3 to <10, & ≥10
3) If itch remains poorly
protocol medication for
controlled, subsequently add
Itch Man Scale used for
hydroxyzine 0.6mg/kg/dose q
6h, then cyproheptadine
Other studies showed
average hospital
0.1mg/g/dose po q6h so that
shower & bath oil
stay days 11.1 +
one of the medications is given
containing liquid
paraffin with 5%
colloidal oatmeal,
39.2% received medication to control
topically applied
itching at the beginning, but eventually
doxepin cream, &
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
all the children took some type of itch
medication because their burn wounds
combination with
got more itching as the course
Objectives of the
Literature review regarding
Below as effective txs for PB pruritus
Good study due to the
PB pruritus relief mgt &
1.Topical txs (cooling agents, colloidal
approach according to
synthesized findings
oatmeal, topical emollients, mixture of
the phase of healing
beeswax & herbal oil, silicone gel
sheeting, & EMLA). No significant
evidence base for
difference for Capsaicin use
algorithm needs to be
2.Oral txs (oral histamnes, gabapentin,
tried & evaluated
naltrexone, some antidepressants, &
effects of tx to
doxepin). Oral chemotherapy & topical
generalize to all burn
on best available
immunosuppressants used for tx-
resistant pruritus
3.Other txs (TENS, botulinum toxin,
Unna's boot dressing, & nanocrystalline silver) 4.Psychological therapies Algorithm shown based on the stage of healing along with the algorithm by Brooks et al. (2008)
Pretest-posttest 2 skin
18 pts– SRMT group,
SRMT significantly affected on burn scar
The study is meaningful
17 pts- control group
healing positively
because massage therapy
clinics in Seoul,
SRMT significantly decreased depression
can have positive effects
Before SRMT & 3months
among burn patients
on pruritus, scar status,
11/2004 & 2/2005
after SRMT, survey for
SRMT significantly decreased pruritus in
and depression among
on pruritus, skin
itching was completed. Burn
Inclusion criteria:
scar & depression assessed
There is a significant positive relationship
18yrs and older,
among depression, objective skin status,
Limit: small sample size,
and pruritus, too
needs more reliable &
thickness burn on
objective burn-scar
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
forearm or hand,
Certified rehabilitation
assessment tools
nurses applied SRMT 30
min/wk for 3months & primary caregivers gave it 10min per day for 3 months
For wound management: massage &
Limited exploration on
latest evidence in
emollients, topical silicone therapy,
post-burn pruritus
Key variables: burn care by
pressure garment therapy, low pulsed
management.-showing
ultrasound, serial intralesional
corticosteroid injections, laser therapy
pruritus management
recent evidence management,
w/o specific doses or
rehabilitation &
For chronic pain: analgesia
For psychosocial care: long-term
psychosocial follow up needed for
For nutrition support: high calorie &
protein with vitamins & minerals
Burn pruritus: massage w/ emollient
cream, cool baths, pressure garments,
& oral and topical antihistamines &
analgesics
Χ 2 analysis was used.
Native American/Alaskan Native race,
facial burns, & ≥ 20% TBSA burns are
Relatively small cohort
HTS is considered of VSS
associated w/ ↑ risk of HTS
No differences b/w VSS
& itch scores in the
Key variables: from pts & Pts
VSS: Pigmentation(0-2),
However, risk for itching is only
subgroup while there is
seen 2 times (one
Vascularity (0-3), Pliability
associated with burn size ≥ 20% TBSA.
differences for the
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
(0-5), Height (0-3)
There is no significant differences
entire population,
after burn, one at
among ages and genders for both HTS
There is no consensus
6-12months after
in the literature as to
constitute hypertrophic
scarring even if a VSS
score of >7 was
itch scores were
determined as a way of
identifying HTS.
Five psychological
Habit reversal: itching is replaced by
approaches to treat wound
alternative behaviors using assessment,
psychological tx can be
associated itching (Habit
education & behavior analysis, and
used for pts w/ pruritus
reversal, Suggestions,
stimulation awareness training
–Habit reversal,
Relaxation training,
Suggestions, Relaxation
11/2013, written
Massage, & Itch-coping
Suggestion: placebo effects have been
training, Massage, &
programs) reviewed from
effective in reducing itching & pain
Itch-coping programs
contains itching
published literature
Relaxation training: many relaxation
Limit: researches are
Key variables: w/wounds or
techniques have been effective to reduce relatively weak from
mgt/tx of itching,
itching (progressive muscle,
low sample sizes, lack
biofeedback-assisted relaxation & heart
of control groups &
rate variability biofeedback)
Massage: massage techniques significantly decreased itching, pain, anxiety, skin status, remaining, depression, skin pigmentation, pliability, vascularity, & height
5-D Itch scale used to
There is a significant difference b/w pre
assess five domains of
and post tx in both group1 & group2
Key variables: Group2:20pts
degree, duration, direction,
regarding pruritus (P<0.05)
phonophoresis is as
disability, and distribution
useful as TENS to
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
There is no significant differences b/w
reduce PB pruritus
2groups regarding effect of pruritus
effectiveness of s, TENS, PB
Mann-Whiney U test used
Limits: No control
to assess b/w 2 groups
group in the study &
small sample noted
Wilcoxon test used to
IC:age:18-50yrs,
assess parameters within
Suggestion: further
2nd & 3rd degree
studies to compare
control group with both
Student t-test used to assess
tx (Triamcinolone
itching>5min &
the difference in the
origin pruritus,
All P values < 0.05
liver, thyroid, & kidney disease, DM, pregnancy, open wound, sensitivity to cortisone, pacemakers, skin malignancy, taking glucocorticoids, phototoxic or immunosuppressive medicine
Early pruritus management: histamine
Not mentioned specific
burn wound, pain
H-1 receptor blocking agent
dosages or frequency of
Key variables: management,
(cetirizine) on as scheduled basis not as tx for PB pruritus, but
pruritus, burn, home car
needed basis combined with frequent
scheduled use of
massage of moisturizers
antihistamine is notable
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
outpatient clinic
In addition, neuro-inflammatory
transmitter blockers (gabapentin &
pregabalin) is effective because itch-
specific neurons won't be stimulated by
these transmitters by using this
(pain, pruritus,
Pt received TENS 9hrs a
Day#1: 62.5% reduction in itching
A larger case study or
within 4hrs of application
full-scale study needed
Key variables: thickness flame
Day#2: 88% reduction within 4hrs of
Assessment for itching
done daily for 5days, at 9th
Day#3 – the end of study (DAY#16):
severe itching &
day, & 16th day after tx
No itching within 4hrs of application
relieve pruritus
Pt did not receive TENS
after 2wks d/t no itching
Group A: 33pts w/pruritus,
Histopathological analysis result:
Patient with post burn
Group B: 18pts w/o
Group A has less elastic fibers (density)
pruritus had broader
burned areas & more
Key variables: ages ranging 8 -
burn, pruritus, 60yrs
Differences b/w groups:
Immunoreactivity of TRP channels in
Group A has thicker burn
burn scar & normal skin result:
They also had elevated
scars, more TBSA, more
TRPV3, TRPV4, & TRPA1 elevated in
male population, & higher
Group A's scar tissue
TPRA1 in the skin
numbers in scar assessment
TRPV4 becomes more
active at temperature >
25°C & by arachidonic
Treatment w/ antagonist
of TRPA1 & TRPV4
Measurements, Operational
Conclusions, Study
Sample & Setting
Definitions of Variables
Results or Findings
Limitations, & Notes
for this population will
be meaningful in the
Current tx options for PB pruritus:
Use of gabapentin
Antihistamines (H1 & H2 receptor
showed excellent relief
antagonists), Topical alternatives over
the healed burn wounds (colloidal
especially tolerated well
oatmeal baths, EMLA, corticosteroids,
massage therapy, Doxepin cream),
significant side effects,
Adjuncts (Biofeedback therapy,
which can be the 2nd
psychological support, combined
choice for the case of
w/pharmacological agents, TENS),
antihistamine resistant
Newer medicine: Ondansetron (5HT-3
receptor antagonist), Gabapentin (anti-
epileptic drug), Pregabalin (anti-convulsant), Paroxetine (SSRI), & Naltrexone (opioid antagonist)
ABSHS = Abbreviated Burn Specific Health Scale; ACD = allergic contact dermatitis; AD = atopic dermatitis; ADHD = attention deficit hyperactivity disorder; BDISF = Beck Depression Inventory-Short Form; bid = twice a day; b/w = between; CAM = complementary and alternative medicine; CG = control group; CLD = cholestatic liver diseases; c/o = complain of; CTD = connetive tissue disease; CU = chronic urticaria; CV = confounding variable; CVD = cardiovascular disease; D/C = Discharge; d/f = defined; DFS = Dutch Fatigue Scale; DM = diabetes mellitus; d/t = due to; DV(s) = dependent variable(s); EC = exclusion criteria; EG = experimental group; EMLA = eutectic mixture of local anesthetic; F = female; f/u = follow up; G = group; GRADE = Grading of Recommendations, Assessment, Development and Evaluation; HD = hemodialysis; HS = hypertrophic scar; ht = height; HTP = hypertrophic scar; hx = history; IC = inclusion criteria; IF = itch frequency; II = itch intensity; info = information; IV(s) = independent variable(s); LAS = Linear Analog Scale; LIS = Leuven Itch Scale; LTF = Long-Term Follow up; M = male; meds = medications; Mexameter = a tristimulus colorimeter device used to measure scar; mgt = management; MRI = magnetic resonance image; MVLR = multivariate logistic regression analysis; mVSS = modified Vancouver Scar Scale; N = Number; NIDRR BMS = National Institute on Disability & Rehabilitation Research Burn Model System; NRS = Numeric Rating Scale; P1 = initial version; P2 = second version; P3 = third version; P4 = fourth version; PB = postburn; PBD = post burn days; P/E = physical examination; PET = positron emission tomography; PG = pressure therapy; PS = plastic surgeon; PSS = Perceived Stress Scale; pt = patient; PTS = post-traumatic stress; PTSD = post-traumatic stress disorder; QD = daily; QoL = quality of life; RCT = randomized clinical trial; r/t = related to; SC = skin condition; SGS = silicone gel sheeting; SLS = Satisfaction with Life Scale; SSRI = selective serotonin reuptake inhibitor; STAI = State Trait Anxiety
Inventory; SWL = satisfaction with life; TBSA = total body surface area; TENS = transcutaneous electrical nerve stimulation; TEWL = transepidermal
water loss; tid = three times a day; TRP = transient receptor potential; TRPA = transient receptor potential ankyrin; TRPV = transient receptor potential vanilloid; TUPS = tissue ultrasound palpation system; tx = treatment; UNC = University of North Carolina; USG = ultrasonography; VAS = visual analog scale; vs = versus; v/s = vital signs; VSS = Vancouver Scar Scale; Wd = wound; wks = weeks; w/ = with; w/o = without; yrs = years.
• Articles are organized by the last name of the first author of each article.
Source: http://nursing.fullerton.edu/programs/pdf/dnp/finalprojects/2015/Kim_YeonSook_DNP_Final_Project_2015.pdf
LEVETIRACETAM - levetiracetam tablet, film coated Solco Healthecare US, LLC DESCRIPTIONLevetiracetam is an antiepileptic drug available as 250 mg (pink), 500 mg (pink), 750 mg (pink), and 1000 mg (white) tablets for oraladministration.The chemical name of Levetiracetam, a single enantiomer, is (-)-(S)-α-ethyl-2-oxo-1-pyrrolidine acetamide, its molecular formula isC8H14N2O2 and its molecular weight is 170.21. Levetiracetam is chemically unrelated to existing antiepileptic drugs (AEDs). It hasthe following structural formula:
Preparation of mouth for removable partial dentures MOUTH PREPARATIONS One of the greatest challenges facing the dentist is the provision of the partially edentulous arch with a successful removable partial denture. To ensure this success, the hard and soft tissues of the particular arch being restored and the associated tissues must be in an acceptable biologic state.