Slep.com.br

Pituitary 7: 83–87, 2004
� 2005 Springer Science + Business Media, Inc. Manufactured in The Netherlands.
Pituitary Apoplexy During Therapy with Cabergoline in an
Adolescent Male with Prolactin-Secreting Macroadenoma
Mirta Knoepfelmacher, Miriam C. Gomes, Maria E.
Melo, and Berenice B. Mendonca
Department of Endocrinology, Hospital das Cl´ınicas, University
of S ˜ao Paulo Medical School, S ˜ao Paulo, Brasil
Abstract. Pituitary adenomas are rare in young patients.
overcome these inconveniences. With duration of action
Prolactinomas are the most common type of pituitary ade-
up to 14 days after single oral dose of 0.3 to 1.0 mg, caber-
nomas in children older than 12 years, occurring more often
goline can be taken only one or twice weekly. Moreover,
in girls, at a 4.5:1 female-to-male ratio. The clinical pre-
cabergoline has been demonstrated to be more effective
sentation may vary according to the age and sex of the pa-
than bromocriptine in the treatment of macroprolacti-
tient. Pituitary apoplexy is a rare life-threatening condition
nomas in adults [10–13] and children [14] with a low
caused by a sudden infarction or hemorrhagic necrosis of the
incidence of side effects, resulting in a very good com-
pituitary containing an adenoma. A wide variety of condi-
tions can trigger apoplexy such as pituitary irradiation, gen-
pliance with dosing. To our knowledge, there has been
eral anesthesia, traumatic head injury, pituitary stimulatory
only one report of pituitary apoplexy with cabergoline
tests and a wide variety of medications including bromocrip-
use [10]. We report the case of an adolescent male with a
tine. We report a case of a 16-year-old male patient with
prolactin-secreting macroprolactinoma who presented
puberty arrest harboring a macroprolactinoma, who devel-
apoplexy 12 months after cabergoline treatment.
oped a sudden clinical picture of pituitary apoplexy during
the 12th month of treatment with cabergoline.
cabergoline, puberty arrest
A 17-year-old male patient was admitted to the En-docrine Department of the Hospital das Cl´ınicas of theUniversity of S ˜ao Paulo complaining of sexual develop-
ment retardation. Puberty had begun at 12, but he expe-rienced pubertal and growth arrest at 13. At 15, he was
Pituitary apoplexy is a rare life-threatening condition
diagnosed as having hypothyroidism, and was treated
with an unknown precise incidence [1]. The classi-
with levothyroxine for 6 months only. The patient re-
cal apoplexy is characterized by headache, visual loss,
ported having had frequent right hemicranial headache
meningismus, and altered mental status [2]. This pathol-
for the previous six months.
ogy is caused by tumoral hemorrhagic necrosis or pitu-
Physical examination revealed a normal young male
itary gland infarction [1]. Over the last 20 years, numer-
weighting 60.4 Kg and measuring 164 cm (−1.7 SD) who
ous case reports and small series have emphasized the
presented an incomplete development of secondary sex-
association of pituitary apoplexy with precipitating fac-
ual characteristics. Facial and body hair were absent,
tors such as radiotherapy, anticoagulation, dynamic en-
pubic hair was Tanner stage III, right and left testes were
docrinological testing, traumatic head injury [2,3], and a
soft and measured 3.8 × 2.0 cm and penis length was
wide variety of medications including bromocriptine [4–
8.3 cm. The neurological examination was unremark-
6], a drug largely used as primary treatment for prolacti-
able. Ophthalmic examination showed normal visual
nomas [7]. Bromocriptine, an ergot-derivative that acti-
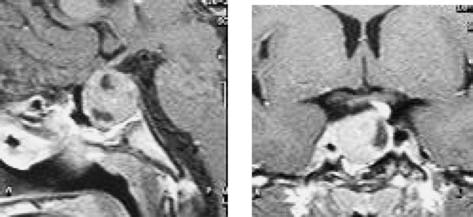
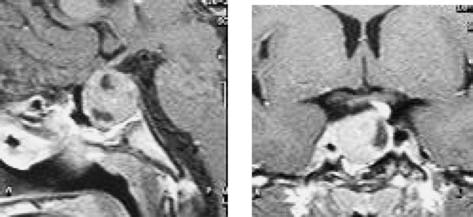
acuity and normal visual fields. T1-weighted contrast
vates D1 and D2 receptors, normalizes serum PRL levels
magnetic resonance imaging (MRI) showed an intra- and
and induces reduction in the tumor size in patients with
suprasellar mass (2.2 × 2.0 × 2.0 cm), with cystic areas,
macroprolactinomas, promoting restoration of gonadal
displacing the chiasma opticum and neurohypophisis to
function, cessation of galactorrhea and improvement in
the left (Fig. 1). Bone age was compatible with 14 years
visual defects in the majority of patients [8,9]. However,
according to the method of Greulich and Pyle. Basal
these important clinical effects are often limited by the
PRL levels were high (Table 1), suggesting the presence
occurrence of side effects such as nausea, vomiting, pos-
of a macroprolactinoma. The combined stimulatory pi-
tural hypotension, headache and dizziness. Therefore, a
tuitary test revealed, in addition to very high prolactin
significant number of patients (up to 20%) does not toler-ate the drug at therapeutic doses or is resistant. Further-more, the compliance to bromocriptine is difficult dueto the short duration of action often requiring several
Address correspondence to: Mirta Knoepfelmacher, R. Dr. En ´eas
doses per day. Cabergoline, another dopamine-agonist
C Aguiar, 255 – PAMB – 2◦ andar – Bloco 6, CEP 05403-900, S ˜ao
with specificity for D2 receptor has been developed to
Paulo, Brasil. E-mail: [email protected]
Knoepfelmacher et al.
Fig. 1. Intra- and suprasellar mass on T1 weighted MRI after
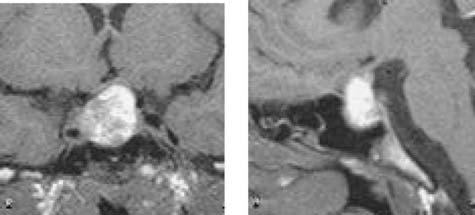
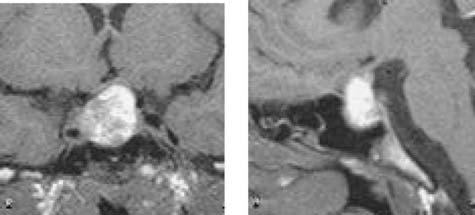
Fig. 3. Increased mass with heterogeneous enhancement,
gadolinium injection, midsagittal and coronal views, before
suggesting pituitary apoplexy.
tomography (CT), which showed an unmodified pitu-itary mass, and a cerebrospinal fluid analysis, whichwas normal. One week later, as the symptoms persisted,he returned to our hospital. The patient referred severeheadache, nausea and asthenia. He did not complain ofvisual abnormalities. Physical examination was normalexcept for postural hypotension. On neurological exam-ination, he was alert and fully oriented, with normal vi-sual fields and normal visual acuity; no papiledema wasevident, and the extra ocular movements were full. Theremaining cranial-nerve functions were also preserved.
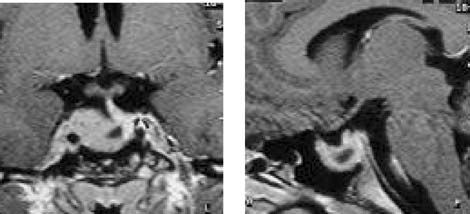
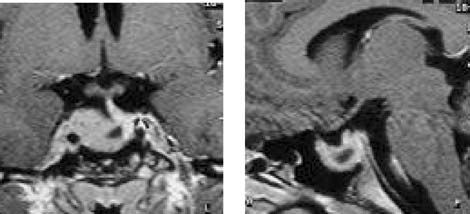
Fig. 2. Tumoral shrinkage 2 months after cabergoline
Laboratory biochemical analysis showed normal lev-
els of glucose, urea nitrogen, creatinine, sodium andpotassium. Pituitary MRI showed an increase in tumoral
levels, multiple pituitary deficiencies: GH, LH, FSH, cor-
volume, with peripheral enhancement and a central
tisol and a hypothalamic pattern of TSH response, with
hyposignal, suggesting an intra-adenoma hemorrhage
low basal levels of free thyroxine.
(Fig. 3), which confirmed our suspicion of pituitary
The patient started replacement treatment with
apoplexy. He was treated with saline and high doses of
levothyroxine and cortisone acetate. The initial treat-
corticosteroids (dexamethasone 16 mg/day) with symp-
ment with bromocriptine (BRC dosed up to 5 mg/day)
tom relief within 24 hours. He was discharged on corti-
was substituted by cabergoline (CAB) 2 weeks later, due
sone acetate, thyroxine and cabergoline (1.5 mg/week).
to the patient's intolerance to BRC. We observed a reduc-
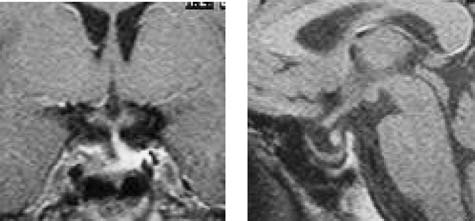
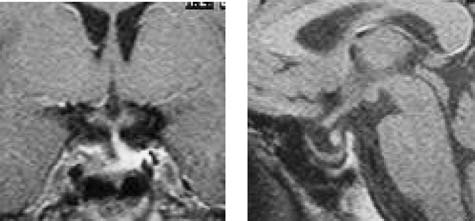
Four months after the apoplexy, an MRI revealed a
tion in tumor volume in the second month of treatment
great reduction in tumor volume, with a partially empty
with cabergoline (Fig. 2). There was a progressive re-
sella (Fig. 4). Six months later, a new MRI showed no
duction of prolactin levels and a normalization of the
alterations. Prolactin levels remained low during treat-
gonadotropin axis (Table 2).
ment with cabergoline (1 mg/week), testosterone levels
After twelve months of cabergoline treatment, the
normalized (Table 2) and the patient presented progres-
patient suddenly presented headache, nausea and vom-
sively normal pubertal development (Tanner IV). One
iting and sought another hospital. He was discharged
year after the apoplexy he was submitted to another
48 hours later, after being submitted to a computed
combined pituitary stimulatory test, which revealed
Table 1. Combined stimulatory pituitary test (TRH 200 µg, GnRH 100 µg and Insulin 0.1 IU/Kg)
Apoplexy 12 m after
GH (µg/L)∗∗
Prolactin (µg/L)
∗Glucose nadir; ∗∗GH: µg/L = 2.6 mU/L; m = month.
Pituitary Apoplexy with Cabergoline
Table 2. Evolution of hormonal levels during treatment with cabergoline
Prolactin (µg/L)
∗After 15 days with bromocriptin; ∗∗Pituitary apoplexy; d = day; m= month.
PCNA, that the predominance of large prolactinomas inmen may be related to a high frequency of rapidly grow-ing tumors, which are often invasive and bromocriptine-resistant [21].
The diagnosis of prolactinoma in our patient was
based on the prolactin level, which was 1.340 µg/L. Nor-mally, such a high prolactin level suggests the presenceof a prolactinoma. Many tumors in the pituitary and inthe suprasellar region can cause an elevation in pro-lactin levels as a result of the stalk disruption, which
Fig. 4. Great tumor reduction causing a partially empty sella
interrupts the normal dopamine inhibition of prolactin
four months after apoplexy and on cabergoline 1 mg/week.
secretion. With the stalk effect, serum prolactin levelsare usually no higher than 150 µg/L but they have beenoccasionally reported to be as high as 600 µg/L [22].
persistence of the previous diagnosed pituitary deficien-
Pituitary apoplexy is a rare but life-threatening condi-
cies (Table 1).
tion caused by sudden infarction or hemorrhagic necro-sis of a pituitary containing an adenoma [1]. According
to Randeva et al. [2] the classical pituitary apoplexy isa clinical syndrome characterized by sudden headache,
We report the case of a male adolescent with a prolactin-
vomiting, visual impairment and meningismus. Subclin-
secreting macroadenoma who presented apoplexy after
ical apoplexy was described in 16% (22/136) of the pi-
12 months of cabergoline therapy. The onset of the pro-
tuitary adenomas of patients younger than 20 years at
lactinoma probably occurred around 13 yrs of age when
surgery [16], but it was symptomatic in only one pa-
arrest of puberty was noticed, but it was diagnosed and
tient (left sixth cranial nerve palsy 5 days after com-
treated only 4 years after the onset of the disease.
pleting irradiation). If the term apoplexy is reserved for
Pituitary adenomas are rare in young patients, rep-
instances where symptomatic hemorrhagic infarction
resenting 3.5–6% of all surgically treated pediatric pitu-
acutely occurs, and for those cases that result in the
itary tumors [15–17]. In a large surgical series, only 6%
clinical syndrome described above, the incidence of pi-
(136/2,230) of the reported patients were younger than
tuitary apoplexy is found to be very low, around 0.6–9.1%
20 years and most of them were at pubertal age [16]. Pro-
of surgically-treated pituitary adenomas [23,24].
lactinomas are the most common type of pituitary ade-
Many authors have emphasized the association of pi-
noma in children older than 12 and are more frequent
tuitary apoplexy with a variety of precipitating events
in girls, at a 4.5:1 female to male ratio [17]. The presen-
such as pituitary irradiation, general anesthesia, trau-
tation of these tumors may vary, depending on the age
matic head injury, dynamic testing using gonadotropin-
and sex of the patient [18–20]. Prepubertal children typ-
or thyrotropin-releasing hormones [1–3,25,26] and a
ically present with a combination of headache, visual
variety of medications including bromocriptine [4–6].
disturbance, and growth failure, whereas pubertal fe-
However, in many cases the association of these events
males frequently present with puberty arrest and hypog-
and apoplexy does not imply necessarily in causa-
onadism, with or without galactorrhea. Pubertal males
tion. A causal relationship between bromocriptine and
may present with headaches and visual impairment, as
apoplexy has been suggested because adenomas have
well as pubertal arrest or growth failure. Gynecomastia
sometimes shown necrosis at surgery after bromocrip-
is not a common sign. Males are more likely than females
tine treatment [23]. Although various factors have been
to present a macroadenoma [18–21] and most authors
proposed to be predisposing events leading to pituitary
explain this feature based on the fact that males, more
apoplexy, most cases are not associated with any pre-
often than females, postpone seeking medical attention
disposing factor [2,3,27]. However, Randeva et al. [2]
because their clinical presentation is less conspicuous.
noted arterial hypertension (conservatively defined as
It has been suggested, however, based upon analysis of
SBP > 160 mmHG or DBP > 90 mmHg) to be the most
the cell proliferation-related nuclear antigens Ki-67 and
common predisposing condition, present in one-fourth
Knoepfelmacher et al.
of their series before the apopletic event. In another
adolescent with pubertal arrest harboring a macropro-
retrospective study, potential precipitating factors were
identified in only nine (30%) of 30 consecutive patientswith pituitary apoplexy [3]. In this series there was no
sex preponderance and no population that seemed tohave more predisposition for pituitary apoplexy, which
1. Rolih CA, Ober KP. Pituitary apoplexy. Endocrinology and
occurred along a broad age range, from the 1st to the
Metabolism Clin N Am 1993;22:291–302.
9th decade, and in tumors of almost any size. The au-
2. Randeva HS, Schoebel J, Byrne J, Esiri M, Adams CBT, Wass
thors concluded that pituitary apoplexy is unpredictable
JAH. Classical pituitary apoplexy: Clinical features, manage-
and should be considered in any patient with abrupt
ment and outcome. Clin Endocrinol 1999;51:181–188.
neuro-ophthalmologic deterioration associated with se-
3. Biousse V, Newman NJ, Oyesiku NM. Precipitating factors in
vere headache.
pituitary apoplexy. J Neurol Neuros and Psych 2001;71:542–
Similarly to our case, pituitary apoplexy was reported
4. Yamaji J, Ishibashi M, Kosaka K, Hori T, Manaka S. Pituitary
late in the course of bromocriptine treatment, in a girl
apoplexy in acromegaly during bromocriptine therapy. Acta
of 14 years with a history of arrested puberty asso-
ciated to a macroprolactinoma [17]. After 6 months
5. Shirataki K, Chihara K, Shibata Y, Tamaki N, Matsumoto S,
of bromocriptine treatment, she suddenly developed
Fujita T. Pituitary apoplexy manifested during a bromocriptine
headaches without impaired vision, followed 2 days
test in a patient with growth hormone and prolactin producing
later by vomiting and fever. Pituitary apoplexy during
pituitary adenoma. Neurosurgery 1988;23:395–398.
cabergoline treatment has been reported previously in
6. Pinto G, Zerah M, Trivin C, Brauner R. Pituitary apoplexy in an
a 26-year-old female patient harboring a macroprolacti-
adolescent with prolactin-secreting adenoma. Hormone Re-
noma [10]. She complained of severe headaches associ-
ated with an increase in tumor size at 12 weeks, need-
7. Vance ML, Evans W, Thorner M. Bromocriptine Ann Intern
ing transsphenoidal surgery. In our case, the patient
8. Liuzzi A, Dallabonzana D, Oppizzi G, Verde GG, Cozzi R,
presented decrease of tumoral volume 2 months after
Chiodini P, Luccarelli G. Low dose of dopamine agonists in
starting treatment with cabergoline, which is in accor-
the long-term treatment of macroprolactinomas. N Engl J Med
dance with the literature [10,28]. This therapy led to
normalization of prolactin levels and tumor size reduc-
9. Molitch ME, Elton RL, Blackwell RE, Caldwell B, Chang RJ,
tion with a low dose of the drug and in a short time,
Jaffe R, Joplin G, Robbins RJ, Tyson J, Thorner MO. Bromocrip-
demonstrating that this prolactinoma was quite respon-
tine as primary therapy for prolactin-secreting macroprolacti-
sive to this dopaminergic agonist. Colao et al. [14] re-
nomas: Result of a prospective multicenter study. J Clin En-
ported a normalization of prolactin in only 10 of 26
docrinol Metab 1985;60:698–705.
young patients with bromocriptine treatment, suggest-
10. Biller BMK, Molitch ME, Vance ML,Cannistraro KB, Davis
KR, Simons JA, Schoenfelder JR, Kklibanski A. Treatment
ing a high incidence of resistance to this drug. How-
of prolactin-secreting macroadenomas with once-weekly
ever, most of them did not meet the criteria for being
dopamine agonist cabergoline. J Clin Endocrinol Metab
considered truly resistant, and there was a suspicion
that many of them were indeed not taking bromocrip-
11. Ferrari CI, Abs R, Bevan JS, Brabant G,Ciccarelli E, Motta T,
tine appropriately, since poor compliance to any chronic
Mucci M, Muratori M, Musatti L, Verbessem G, Scanlon MF.
treatment is quite often in children and adolescents.
Treatment of macroprolactinomas with cabergoline: A study
In addition, many of these patients presented intoler-
of 85 patients. Clin Endocrinol (Oxf.) 1997;46:409–415.
able gastrointestinal side effects, requiring drug discon-
12. Colao A, Di Sarno A, Landi ML, Crillo S, Sarnacchiaro F,
tinuation. When these patients were treated with an
Facciolli G, Annunziato L, Lombardi G. Long-term and low-
average dose of cabergoline almost all of them pre-
dose treatment with cabergoline induces macroprolactinomashrinkage. J Clin Endocrinol Metab 1997;82:3574–3579.
sented reduction of prolactin levels and tumor size, as
13. Verhelst J, Abs R, Maiter D, Van Den Bruel A, Vandeweghe M,
occurred with our patient who also was intolerant to
Velkeniers B, Mockel J, Lamberigts, Perossians P, Coremans P,
Mahler C, Stevenaert A, Verlooy J, Raftopoulos C, Beckers A.
In this report, the patient presented apoplexy 12
Cabergoline in the tretment of hyperprolactinemia: A study in
months after cabergoline treatment, which is a rare late
455 patients. J Clin Endocrinol Metab 1999;84:2518–2522.
manifestation after tumor reduction, although pituitary
14. Colao A, Loche S, Cappa M, Di Sarno A, Landi ML, Sarnacchiao
hemorrhage, with or without clinical apoplexy, may de-
F, Faccioli G, Lombardi, G. Prolactinomas in children and ado-
velop in small adenomas [23,24]. Although the described
lescents. Clinical presentation and long-term follow-up. J Clin
apoplexy may not be causally related to cabergoline use,
Endocrinol Metab 1998;83:2777–2780.
it suggests that any patient harboring a macroprolacti-
15. Partington MD, Davis DH, Laws ER Jr, Scheithauer BW. Pi-
tuitary adenomas in childhood and adolescence: Results of
noma is at risk of undergoing a pituitary apoplexy even
transsphenoidal surgery. J Neuros 1994;80:209–216.
when tumor reduction has taken place, and at any time
16. Mindermann T, Wilson CB. Pituitary adenomas in childhood
during treatment with a dopaminergic analog. However,
and adolescence. Journal of Pediatric Endocrinology and
this risk is quite small overall.
In conclusion, we present a case of pituitary
17. Knwar S, Wilson CB. Pediatric pituitary adenomas. J Clin En-
apoplexy associated to cabergoline treatment in a male
docrinol Metab 1999;84:4385–4389.
Pituitary Apoplexy with Cabergoline
18. Calle-Rodrigue RD, Gianni C, Scherthauer BW, Lloyd RV,
24. Mohr G, Hardy J. Haemorrhage, necrosis and apoplexy in pi-
Wollan PC, Kovacs KT, Stefaneanu L, Ebright AB, Abboud
tuitary adenomas. Surg Neurol 1982;18:181–189.
CF, Davis DH. Prolactinomas in male and female patients:
25. Miranda M, Barros L, Knoepfelmacher M, Augusto E,
A comparative clinical pathologic study. Mayo Clinic Proc
Jacomosi A, Cukiert A, Salgado LR, Goldman J, Liberman
B. Pituitary apoplexy followed by endocrine remission.
19. Delgrange E, Maiter D, Donckier J, Tourniare J. Influence of
Report of two cases. Arqu Neuro-Psiq 1998;56(3):449–
age on the clinical presentations of prolactinomas in male. Min
26. Knoepfelmacher M, Ursich M, Barros LM, Duarte A, Salgado
20. Tyson D, Reggiardo D, David R. Prolactin-secreting macroade-
LR, Pimentel-Filho FB, Liberman B. Insulin resistance associ-
nomas in adolescents. Response to bromocriptine therapy. Am
ated to high levels of TNF during pituitary apoplexy induced
J Dis Child 1993;147:1057–1061.
by a pituitary stimulating test in an acromegalic patient. The
21. Delgrange E, Trouillas J, Maiter D, Donckier J, Tourniaire J.
Sex-related difference in the growth of prolactinomas: A clin-
27. Cardoso ER, Peterson EW. Pituitary apoplexy: A review. Neu-
ical and proliferation marker study. J Clin Endocrinol Metab
28. Colao A, Di Sarno A, Landi ML, Scavuzzo F, Cappabianca
22. Albuquerque PC, Hinton DR, Weiss MH. Excessively high pro-
P, Pivonello R, Volpe R, Di Salle F, Cirillo S, Annunziato
lactin level in a patient with a nonprolactin-secreting adenoma:
L, Lombardi G. Macroprolactinoma Shrinkage during caber-
Case report. J Neuros 1998;89:1043–1046.
goline treatment is greater in naive patients than in pa-
23. Wakai S, Fukushima T, Teramoto A, Sano K. Pituitary apoplexy:
tients pretreated with other dopamine agonists: A prospective
Its incidence and clinical significance. J Neuros 1981;55:187–
study in 110 patients. J Clin Endocrinol Metab 2000;87:2247–
Source: http://www.slep.com.br/archivos/contenidos_docs/Cabergoline.pdf
ARE YOU READY TO BE MORE THAN LIKED? FIND YOUR BRAND ADVOCATES – THE TRUE MAVENS OF YOUR BRAND By Mary Kate Scott SO, YOU'VE HIRED A SOCIAL MEDIA enough, that they want to be a "maven" and LIAISON. YOU HAVE A FACEBOOK PAGE, know all about your product. Brand YOU TWEET, AND MAYBE YOU'VE EVEN
5990 • The Journal of Neuroscience, April 15, 2015 • 35(15):5990 –5997 Striatal D1- and D2-type Dopamine Receptors Are Linked to Motor Response Inhibition in Human Subjects Chelsea L. Robertson,1,5 Kenji Ishibashi,3,4 Mark A. Mandelkern,5,6 Amira K. Brown,3 Dara G. Ghahremani,3 Fred Sabb,3