Early and visible improvements after application of k101 in the appearance of nails discoloured and deformed by onychomycosis
Journal of Cosmetics, Dermatological Sciences and Applications, 2011, 1, 59-63
doi:10.4236/jcdsa.2011.13010 Published Online August 2011 (http://www.SciRP.org/journal/jcdsa)
Early and Visible Improvements after Application
of K101 in the Appearance of Nails Discoloured
and Deformed by Onychomycosis
Jan Faergemann1, Sören Gullstrand2, Kjell Rensfeldt3
1Department of Dermatology, Sahlgrenska University Hospital, Gothenburg, Sweden; 2Möllevångens Husläkargrupp, Malmö, Swe-
den; 3Moberg Derma AB, Bromma, Sweden.
Email:
[email protected] Received June 9th, 2011; revised July 14th, 2011; accepted July 19th, 2011.
ABSTRACT
Onychomycosis is a fungal infection of the nails of the fingers and toes and is difficult to cure. A previous 24
-week,
placebo-controlled study demonstrated that a solution containing propylene glycol,
urea and lactic acid (
K101)
was
well-tolerated and effective in the treatment of onychomycosis. Patients who received K101
judged that their condition
had improved from Week 2
of treatment onwards. The aim of the current study was to further evaluate and document
early visible effects on nail appearance after application of topical K101
in an 8-week baseline-controlled study in 75
patients. Patients graded the appearance of their nail compared with baseline using a four-point scale. Compared with
baseline,
91.8
% (67
/73;
95
% confidence interval (
CI):
83.0
%, 96.9
%)
of the patients experienced at least some im-
provement in their target nail after 8 weeks of treatment. At Week 2,
the proportion showing some improvement was
76.7
% (56
/73;
95
% CI:
65.4
%,
85.8
%)
with this number increasing to 87.7
% (64
/73;
95
% CI:
77.9
%,
94.2
%)
at Week 4
.
Proportions of patients reporting less thickened, less discoloured,
less brittle and softer nails increased over the course
of the study. No safety issues were identified. In conclusion,
K101
provided early visible improvements in nails affected
by onychomycosis.
Keywords: K101,
Onychomycosis,
Early Effects,
Topical
1. Introduction
can include fatal liver toxicity [8]. Topical agents are usually formulated as lacquers that adhere to the nail
Onychomycosis is a fungal infection that affects the nails
plate and include antifungal drugs such as amorolfine,
of the hand and foot. Infection rates in Western adult
tioconazole and ciclopirox 8% [5,7]. Topical application
populations range from 2% to 14%, although onycho-
allows targeted delivery to infected areas, minimising the
mycosis may affect up to 50% of people over 70 years of
risk of secondary effects related to systemic exposure.
age [1]. Prevalence of onychomycosis is also higher in the immuno-compromised, children with Down's syn-
K101, a topical treatment for onychomycosis, is a
drome and patients with diseases that affect the periph-
combination of propylene glycol, urea and lactic acid.
eral circulation, such as diabetes mellitus [2,3]. Ony-
The concept of using propylene glycol solutions of urea
chomycosis is often associated with pain and discomfort
and lactic acid to treat onychomycosis was investigated
coupled with a significant negative impact on emotional
in a study of 23 patients who applied a test solution twice
health and social image [4,5].
daily for 2 - 6 months. The solution was effective in 21
Onychomycosis can be treated pharmacologically with
of the 23 patients treated [9]. The efficacy of K101 was
both systemic and topical agents [6]. Systemic antifungal
confirmed in a placebo-controlled study that documented
drugs such as terbinafine and itraconazole are effective
the efficacy and tolerability of K101 versus placebo in
treatments; although their use must be balanced against
493 patients with onychomycosis. A greater number of
the risk of unpleasant side-effects that include gastroin-
patients who received K101 experienced mycological
testinal disorders, skin rashes and headache [5,7]. Serious
cure after 26 weeks of treatment (27% versus 10%) [10].
side-effects occur in less than 1% of patients, but these
Also, almost half the patients who received K101 con-
Copyright 2011 SciRes.
JCDSA
Early and Visible Improvements after Application of K101 in the Appearance of Nails Discoloured and
Deformed by Onychomycosis
sidered that their condition had shown at least some im-
tients. Photographs were taken at baseline and after 2, 4
provement from Week 2, and approximately 75% from
and 8 weeks of treatment. Patients were asked the fol-
Week 8 of treatment onwards. In the light of these find-
lowing question: "How do you perceive your target nail
ings, and to investigate in more detail the early clinical
appearance compared to baseline?", and then evaluated
effects of K101, we conducted an 8-week study in pa-
the efficacy of their treatment using a four-point Global
tients with nails affected by onychomycosis.
Assessment Scale. The scores used were: 1) no im- provement; 2) some improvement; 3) clear improvement;
2. Methods
and 4) very good improvement. Patients were also asked
2.1. Study Population
whether the target nail had become less thickened, dis- coloured or brittle and whether it had softened.
The study population comprised men and women aged at least 18 years with clinically diagnosed onychomycosis
2.4. Safety Assessments
affecting between 25% and 75% of at least one big toe-
Adverse events were recorded from the start of the first
nail or thumbnail. Patients were excluded if they had
treatment period to the end of the study. At each study
proximal subungual onychomycosis or other conditions
visit, investigators asked patients the following question:
known to cause abnormal nail appearance. Patients who
"Have you had any health problems since your last
had participated in another study with K101 or in any
visit?". The Investigator rated any reported events for
study with an investigational drug or device within 4
intensity and relationship to study treatment.
weeks of screening were ineligible, as were patients who had used topical antifungal nail treatment within 1 month
2.5. Statistical Analysis
or systemic antifungal treatment within 3 months of
Seventy patients were to be enrolled to provide 65
screening. Patients with a known allergy to any of the
evaluable patients. With a sample size of 65, a two-sided
study treatment components were excluded from the
95% confidence interval (CI) for the proportion of
study. The study was conducted at Sahlgrenska Univer-
patients who experienced at least some improvement in
sity Hospital (Gothenburg, Sweden) and Möllevångens
target nail appearance (who scored 2 or more according
Husläkar-grupp (Malmö, Sweden) after approval by the
to the Global Assessment Scale) after 8 weeks' treatment,
Regional Ethics Committee (Gothenburg, Sweden). All
was to extend 0.12 from the observed proportion for an
patients provided signed and dated informed consent
expected proportion of 0.50.
prior to screening.
The primary efficacy endpoint was an improvement in
2.2. Study Design
target nail appearance at 8 weeks compared with baseline, which was defined as the proportion of patients scoring
This was an 8-week baseline-controlled study to assess
at least 2 on the Global Assessment Scale. Other end-
the efficacy of K101 in improving nail appearance. At
points included the proportion of patients scoring at least
the baseline visit at the study site, patients were taught
2 on the Global Assessment Scale at Week 2 and Week 4
how to apply K101 by study staff. K101 is a clear, col-
and individual nail attributes at Week 2, Week 4 and
ourless liquid supplied in a 10 mL plastic tube with a
Week 8. All efficacy endpoints were presented as point
silicon drop tip to ensure accurate application to the af-
estimates with two-sided 95% CIs computed using the
fected nail. A thin layer of the K101 solution was applied
Clopper-Pearson (exact) method. Adherence was calcu-
to all affected fingers and/or toenails at bedtime every day. An affected big toenail or thumbnail was selected as
lated as the percentage of maximum use of K101.
The safety analysis set comprised all randomised pa-
the target nail for all subsequent assessments. After their
tients who applied study medication at least once. The
visit at baseline, patients returned 2, 4 and 8 weeks after
per protocol set was a subset of the full analysis set and
starting treatment to undergo efficacy and safety evalua-
consisted of patients with 80% adherence who had not
tions. At each study visit after starting treatment, patients
experienced major protocol violations and who had a
were asked "On average, how many days per week have
measure of the primary endpoint. SAS® software (ver-
you applied the test product since last visit?".
sion 9.2, SAS Institute Inc., Cary, NC, USA) was used
2.3. Efficacy Assessments
for the statistical analysis.
The target nail was photographed in a standardised way
3. Results
using a digital camera and camera stand; the stand was
3.1. Patient Disposition
equipped with lighting to create consistent light condi- tions. Care was taken to ensure that the distance between
Seventy-five patients were enrolled and 72 completed the
the camera and the nail was exactly the same for all pa-
study. The mean age of the patients was 60 years. Most
Copyright 2011 SciRes.
JCDSA

Early and Visible Improvements after Application of K101 in the Appearance of Nails Discoloured and
Deformed by Onychomycosis
patients were male (63.5%) and Caucasian (97.3%).
Table 3. Patient assessment of individual nail attributes (full
Three patients were discontinued from the study: one due
analysis set; N = 73).
to protocol non-compliance and two due to non-atten- dance at follow-up visits. All patients had abnormal fin-
ger and/or toenails and 22 (29.7%) had abnormal skin on
hands and feet as a result of fungal infection. Overall,
mean (standard deviation) adherence was 99.45 (2.3) %
(full analysis set).
3.2. Efficacy Results
The proportion of patients experiencing at least some
improvement of the target nail at 8 weeks, compared
with baseline, was 91.8% (67/73 patients; 95% CI; 83.0,
96.9) (Table 1. full analysis set). After 2 weeks of treat-
ment, 76.7% (56/73) of patients experienced at least some improvement of the target nail; this proportion in-
CI: confidence interval.
creased to 87.7% (64/73) after 4 weeks. Similar results
were obtained for the per protocol data set. During the
treatment period, the number (%) of patients reporting
clear/very good improvement of the target nail increased
from nine (12.4%) at Week 2 to 38 (52.0%) at Week 8
(Table 2).
Over the 8 weeks of the study, increasing proportions
of patients reported that, compared with baseline, their
target nails were less thickened (from 32.9% at Week 2
to 75.3% at Week 8), less discoloured (from 60.3% to
67.1%), less brittle (from 15.1% to 45.2%) and softened
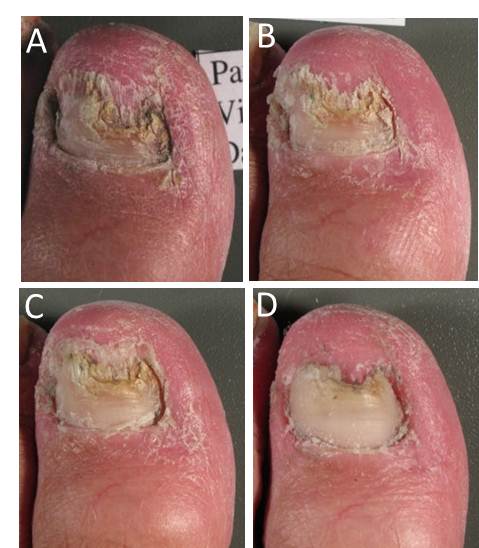
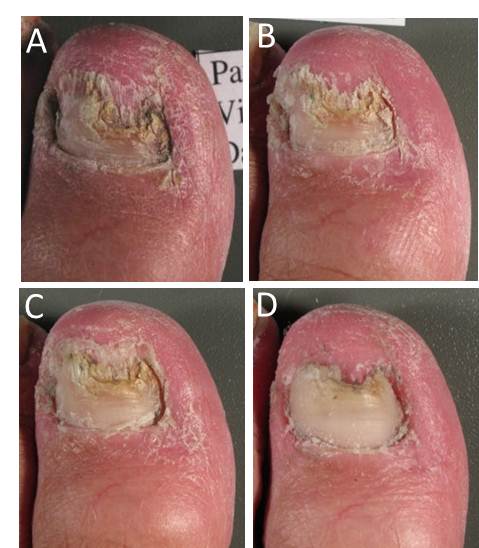
(from 35.6% to 71.2%) (Table 3). Visible improvements
in the condition of the target nails from baseline to Week
8 are presented in Figure 1 for a patient with infection of
moderate baseline intensity and in Figure 2 for a patient
Figure 1. Photographic sequence showing target nail ap-
with infection of severe baseline intensity. In the course
pearance at baseline (Panel A), at Week 2 (Panel B), Week 4
(Panel C) and Week 8 (Panel D) for a patient with onycho-
of treatment, visible signs of fungal infection regressed
mycosis of moderate intensity at baseline.
Table 1. Improvement in target nail (defined as a score ≥ 2
on the Global Assessment Scale).
Full analysis set (N = 73)
Per protocol set (N = 71)
CI: confidence interval
Table 2. Patient experience of target nail appearance com-
pared with baseline (full analysis set; N = 73)
Figure 2. Photographic sequence showing target nail ap-
Some improvement
pearance at baseline (Panel A), at Week 2 (Panel B), Week 4
Clear improvement
(Panel C) and Week 8 (Panel D) for a patient with onycho-
Very good improvement
mycosis of severe intensity at baseline.
Copyright 2011 SciRes. JCDSA
Early and Visible Improvements after Application of K101 in the Appearance of Nails Discoloured and
Deformed by Onychomycosis
and in general, a more uniform and smooth appearance
study; no adverse events were judged to be treat-
was observed throughout the nail.
ment-related by the Investigator. In a 24-week long, dou-
3.3. Safety and Tolerability
ble-blind, placebo-controlled study with K101, irrita- tion/pain was observed in the periungual skin in 22
Eight patients (10.8%) experienced nine adverse event
(6.4%) patients who received K101. In that study, K101
episodes; none of these was judged to be related to K101
was applied to the nail drop-wise, which presumably
by the Investigator. Seven of the events were considered
increased the likelihood that the solution would contact
to be mild and two were moderate in intensity. The most
and leach into the skin surrounding the infected nail.
frequently reported adverse event was rhinorrhoea (n =
Also, the target nail was occluded with surgical tape for
the first 4 weeks of treatment, which may have amplified
4. Discussion
skin irritation. In the current study, the applicator con- sisted of a tube with a silicon tip so that the K101 solu-
This 8-week, open-label study was designed to evaluate
tion could be spread more precisely over the nail surface,
the early clinical effects of treatment with K101 in pa-
thus minimising the risk for irritation or pain in the peri-
tients with onychomycosis. Efficacy was assessed in
ungual skin. Photographs from the current study showed
terms of improvement from baseline in nail appearance.
that, in some cases, the treated nails became more opaque.
Standardised photographic techniques were used to
However, this was not reflected in the adverse event re-
document at regular intervals any changes in appearance
porting indicating that patients did not consider this to be
from baseline. With just 2 weeks of treatment the propor-
tion of patients with visible improvements in the target
In conclusion, data from the current study support ear-
nail was of 76.7% and this number increased to 91.8% by
lier findings that clearly demonstrate rapid improvements
Week 8 (primary endpoint). As the study progressed,
in nail condition after application of K101; early, visible,
treatment was associated with the retreat of typical signs
positive effects compared with baseline were observed
of fungal nail infection such as the development of a less
from 2 weeks onwards. This topically applied solution
discoloured and smoother nail surface.
also appears to demonstrate characteristics conducive to
When rating the condition of their nails for thickness,
good adherence such as an excellent tolerability profile
discolouration, brittleness and softness, patients generally
and once daily application.
reported improvements from baseline at Week 2, Week 4
5. Acknowledgements
and Week 8. These data support the findings of a previ-ous study in which half the patients enrolled (152/304
The authors would like to thank the patients and staff who participated
patients) perceived at least some improvement in their
in the study. This study was funded by Moberg Derma AB.
condition after only 2 weeks of treatment [10].
There are limited data within the scientific literature
REFERENCES
on adherence to treatment in patients with onychomyco-
[1] B. E. Elewski and M. A. Charif, "Prevalence of Onycho-
sis, with the available data generally determined in stud-
mycosis in Patients Attending a Dermatology Clinic in
ies of oral treatments rather than topical applications.
Northeastern Ohio for Other Conditions," Archives of
One study reported that the key determinants in patient
Dermatology, Vol. 133, No. 9, 1997, pp. 1172-1173.
preferences for an oral onychomycosis treatment were
duration of therapy, frequency of treatment and number
[2] A. K. Gupta, N. Konnikov, P. MacDonald, P. Rich, N. W.
of drugs [11]. Another study concluded that the main
Rodger, M. W. Edmonds, et al., "Prevalence and Epide-
reasons for patient non-adherence were adverse events,
miology of Toenail Onychomycosis in Diabetic Subjects:
financial restraints and the premature perception by pa-
A Multicentre Survey," British Journal of Dermatology, Vol. 139, No. 4, 1998, pp. 665-671.
tients that the improvement in their condition was asso-
ciated with cure [12]. In terms of factors known to affect
[3] E. L. Svejgaard and J. Nilsson, "Onychomycosis in Den-
patient adherence in the current study, treatment with
mark: Prevalence of Fungal Nail Infection in General
K101 was associated with a very low incidence of ad-
Practice," Mycoses, Vol. 47, No. 3-4, 2004, pp. 131-135.
verse effects and only once daily application was re-
[4] B. Elewski, "Onychomycosis: Pathogenesis, Diagnosis,
quired. Results from the present study clearly indicate
and Management," Clinical Microbiology Reviews, Vol.
that the majority of patients were very happy with early
11, No. 3, 1998, pp. 415-429.
positive results and this encouraged them to achieve the
[5] D. de Berker, "Clinical Practice. Fungal Nail Disease,"
very high levels of adherence that were observed (99%).
New England Journal of Medicine, Vol. 360, No. 20,
K101 was very well-tolerated in patients in the current
Copyright 2011 SciRes. JCDSA
Early and Visible Improvements after Application of K101 in the Appearance of Nails Discoloured and
Deformed by Onychomycosis
[6] A. K. Gupta, M. Uro and E. A. Cooper, "Onychomycosis
[10] L. Emtestam, T. Kaaman and K. Rensfeldt, "Treatment of
Therapy: Past, Present, Future," Journal of Drugs in
Distal Subungual Onychomycosis with a Topical Prepa-
Dermatology, Vol. 9, No. 9, 2010, pp. 1109-1113.
ration of Urea, Propylene Glycol and Lactic Acid: Results
[7] O. Welsh, L. Vera-Cabrera and E. Welsh, "Onychomyco-
of a 24-Week, Double-Blind, Placebo-Controlled Study,"
sis," Clinics in Dermatology, Vol. 28, No. 2, 2010, pp.
[11] S. Nolting, J. Carazo, K. Boulle and J. R. Lambert, "Oral
[8] D. P. O'Sullivan, C. A. Needham, A. Bangs, K. Atkin and
Treatment Schedules for Onychomycosis: A Study of Pa-
F. D. Kendall, "Postmarketing Surveillance of Oral Ter-
tient Preference," International Journal of Dermatology,
binafine in the UK: Report of a Large Cohort Study,"
Vol. 37, No. 6, 1998, pp. 454-456.
British Journal of Clinical Pharmacology, Vol. 42, No. 5,
1996, pp. 559-565.
[12] Y. Hu, L. Yang, L. Wei, X. Y. Dai, H. K. Hua, J. Qi, et
[9] J. Faergemann and G. Swanbeck, "Treatment of Ony-
al., "Study on the Compliance and Safety of the Oral An-
chomycosis with a Propylene Glycol-Urea-Lactic Acid
tifungal Agents for the Treatment of Onychomycosis,"
Solution," Mycoses, Vol. 32, No. 10, 1989, pp. 536-540.
Zhonghua Liu Xing Bing Xue Za Zhi, Vol. 26, No. 12,
2005, pp. 988-991.
Copyright 2011 SciRes. JCDSA
Source: http://www.nalox.no/fileadmin/sites/nalox_no/10.2_J._Faergemann_et_al._Early_and_Visible_Improvements.pdf
Bio/Pharma Quarterly Journal Volume 10, Issue 4 December, 2004 Division of Bio/Pharmaceutical Sciences Society of Chinese Bioscientists in America (SCBA) Princeton, NJ 08643 Chief Editor Lu-Hai Wang, Ph.D. Mount Sinai School of Medicine E-mail:[email protected] TEL: (212) 241-3795 FAX: (212) 534-1684 Editors Flora W. Feng, Esq.
REV ARGENT NEUROC VOL. 28, Nº 3 : 78-98 2014 REVISIÓN DE LA LITERATURA Cirugía de los trastornos del comportamiento: el estado del arte Claudio Yampolsky, Damián Bendersky Servicio de Neurocirugía, Hospital Italiano de Buenos Aires, Ciudad Autónoma de Buenos Aires, Argentina RESUmENIntroducción: la cirugía de los trastornos del comportamiento (CTC) se está convirtiendo en un tratamiento más común desde el desarrollo de la neuromodulación. Podemos dividir su historia en 3 etapas: la primera comienza en los inicios de la psicocirugía y termina con el desarrollo de las técnicas estereotácticas, cuando comienza la segunda etapa. Ésta se caracteriza por la realización de lesiones estereotácticas. Nos encontramos transitando la tercera etapa, que comienza cuando la estimulación cerebral profunda (ECP) empieza a ser usada en CTC.Objetivo: el propósito de este artículo es realizar una revisión no sistemática de la historia, indicaciones actuales, técnicas y blancos quirúrgicos de la CTC. Resultados: a pesar de los errores graves cometidos en el pasado, hoy en día, la CTC está renaciendo. Los trastornos psiquiátricos que más frecuentemente se tratan con cirugía y los blancos estereotácticos preferidos para cada uno de ellos son: cápsula interna/estriado ventral para trastorno obsesivo-compulsivo, cíngulo subgenual para depresión y complejo centromediano/parafascicular del tálamo para síndrome de Tourette. Conclusión: los resultados de la ECP en estos trastornos parecen alentadores. Sin embargo, se necesitan más estudios randomizados para establecer la efectividad de la CTC. Debe tenerse en cuenta que una apropiada selección de pacientes nos ayudará a realizar un procedimiento más seguro así como también a lograr mejores resultados quirúrgicos, conduciendo a la CTC a ser más aceptada por psiquiatras, pacientes y sus familias. Se necesita mayor investigación en varios temas como: fisiopatología de los trastornos del comportamiento, indicaciones de CTC y nuevos blancos quirúrgicos.