Powerpoint presentation
Renal Care in the Community
Lynette Knuth. RN, BSc, PG cert Crit care, PGDip NS. 2014 Masters candidate Chronic Kidney Disease – Stage 4 Nurse Specialist - 0.5 fte Clinical Nurse Specialist – 0.1 fte Dialysis Nurse (PD and HD) – 0.3 fte 30 May 2014
• Past, present and future of the Anaemia protocol
• CKD stage 4: management
• Advanced care planning: end of life care
Past, present and future! Our anaemia protocol
• Anaemia protocol started around 2004
• Roche employed nurses to coordinate the protocol – move it into
• Temporary positions • To ensure primary physicians can manage renal anaemia
• These nurses were passionate and proud. • Very good at their jobs and wanted to keep their jobs*
• Taranaki was the first protocol
• Presented at many Australasian conferences.
• After having the protocol within the primary sector for 8 years,
Roche pulled funding for their positions.
• These nurses went into "Save our jobs" mode • DHBs didn't listen, they still lost their jobs…
SO……. What's happening now
• Fair enough, by rights after 10 years of having this protocol
out… we shouldn't need them
• The whole purpose of the anaemia coordinator was to get the
protocol out and usable
• Make it fully managed by GPs • Why
• Saves the patient admissions to hospital
• No blood transfusions – no antibodies when comes to Tx • Saves $1200/night/patient in hospital – tax payers money • Good revenue for GPs • Easy protocol
• Across the country, anaemia jobs have been disestablished • CKD nurse to organise
• Special authorities for all renal anaemia patients • Iron infusions for CKD patients
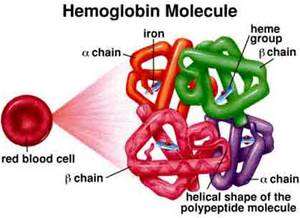
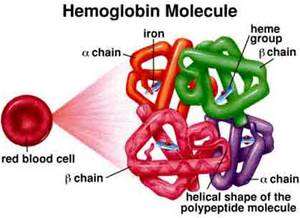
• Erythropoietin (EPO) Administration
•
• Start EPO in the dose of 4000 units subcutaneously once a week
• Monitor Hb, iron status, renal function, albumin, and BP (blood pressure) monthly
• If Ferritin > 500 microg/L then check CRP and Reticulocyte count
• Adjust EPO dose as below
•
• Hb < 110 g/l:
•
• Increase EPO dose by 1 step
•
• Hb 110 – 120 g/l:
•
• No change in EPO dose
•
• Hb > 120 g/l:
•
• Reduce EPO by one step
•
•
• • STOP EPO and restart at lower step when Hb is <120
Weekly Dose
Weekly frequency
1000 units equivalent
2,000 units x fortnightly
2000 units
2,000 units x once a week
3000 units
3,000 units x once a week
4000 units
4,000 units x once a week
5000 units
5,000 units x once a week
6000 units
6,000 units x once a week
8000iu units
4,000 units x twice a week
10000 units
10,000 units x once a week
12000 units
6,000 units x twice a week
Parts of the protocol often not read
• The general practitioner will consult with the renal physician, (Dr A
Williams), if there are any difficulties in achieving target haemoglobins, or for any other queries related to this protocol.
• Oral Iron Administration
• NB: If BP > 160/100 do not give EPO – ****refer to renal
• NB: ****Refer to Physician**** if:
• Hb increase is > 10g/L in the past month • Hb increase is < 3 g/L in the past month and is below target range • Hb < 80 g/L and patient is on EPO • Hb increase above target range despite previous dose decrease • CRP > 50
Chronic Kidney Disease (CKD)
www.kidneys.co.nz
Who should usually be referred to a nephrologist?
• eGFR <30mL/min/1.73m2* • Persistent significant albuminuria (urine ACR >30mg/mmol) • A consistent decline in eGFR from a baseline
<60mL/min/1.73m2
>5mL/min/1.73m2
(a decline over a six-month period which is confirmed on at least three
separate readings)
• Glomerular haematuria with macroalbuminuria • CKD and hypertension that is hard to get to target despite • At least three anti-hypertensives • Diabetes with eGFR <45mL/min/1.73m2**
Prognosis of CKD by GFR and albuminuria category
Albuminuria Stage
Microalbuminuria Macroalbuminuria
(Urine ACR mg/mmol)
(Urine ACR mg/mmol)
(Urine ACR mg/mmol)
Female: < 3.5
structural or pathophysiological abnormalities present
< 15 or on dialysis
Progression risk
Causes of new patients 2012
• Cease smoking • Weight management • Physical activity • Good nutrition • Alcohol intake • Blood pressure management • Proteinuria management • CVD Risk • Blood glucose management
• Up to 80% of our dialysis population could have been
• Incentre Haemodialysis patients can cost up to if not more
than $100,000/per year/patient
• Peritoneal dialysis patients can cost up to $50,000
• Big drive for community dialysis and pre-emptive
transplantation…
Continuum of development, progression and complications CKD
Management of CKD Patients
• First we need to prevent CKD… Diabetes, obesity, heart
• Main aim of management:
• Prevent Complications
• Prolong period before needing dialysis
• Positive end of life
• Anaemia – Iron stores first - then EPO • BP management • Bone health • Kidney monitoring • Symptom management • Cognitive testing • Advanced care planning
Bone health and Kidney Failure
• Phosphate - Increases • Calcium - Decreases • PTH - Increases • Alk Phos – Increases
• What does Calcium carbonate work on? • What does Calcitriol work on? • What does Aluminium work on? • What does increased alk phos indicate?
• Phosphate absorbed by food
• Dairy/Meat/Eggs
• Excreted mainly by kidneys, some by the bowel
• Calcium increased by PTH activation of vitamin D
• Excreted mainly by bowel, little by kidney, reabsorbed by kidneys.
• Released in response to low extracellular concentrations of free Ca+ • Stimulates production of inactivated vitamin D • Mobilization of Calcium from bone • Suppresses calcium loss in urine
• Inactivated Vitamin D – 25 Dihydroxylvitamin D
• Converted by liver • Mobilised to kidney convert it to useable form
• 1,25 dihydroxycalciferol – increases Ca+ absorption in intestine.
Bone health and kidney problems Simply
• Phosphate is not excreted via kidneys
• Serum phos rises
• Unable to activate Vitamin D
• Absorption of Ca+ is decreased • Serum Ca+ decreases • PTH hyper secreted, in an effort to increase intestinal absorption
Complications of poor bone health
• Alk Phos rises = Damage to bone structure. CKD-MBD • Brittle Bones • Deformation • "Chalk" vessels • Calciphylaxis
Years of poor bone health
Bone Health Medications
• Phosphate Binders – Calcium carbonate and aluminium taken
with every meal – Ca Carb - CHEWED!! – excrete phosphate through bowels
• Calcitriol – (Rocaltrol) Activated Vitamin D to increase Calcium
and suppress secretion of PTH.
New Initiatives - TDHB
Cognitive Testing
Cognitive Testing
• Up to 70% of HD patients have chronic cognitive impairment -
Moderate to Severe
• Unrecognized cognitive impairment
• Functional status of older patients that start dialysis is
maintained in only 13% of these patients
• Cognitive and functional impairment is associated with
increased risk of death amongst dialysis patients
Why do cognitive testing
• Failure to train patients onto home dialysis • Prevent early death within 6 months of starting dialysis • Gives an understanding how these patients will train
• To early to tell results
• Pre-dialysis cognitive testing
• Addenbrooke's tests
• Survival calculations at pre-dialysis modality session
• ANZdata calc • Haemodialysis calc
• On dialysis, every 12 months (Only HD patients at this point)
• Test for deterioration – 30% of our patients have deteriorated
Advance Care Planning
End of life care
• What is Advanced Care Planning?
• Process – capable (Mentally competent) adult engages in a plan
about health care decisions, in the event that they become incapable (Legally incompetent) to personally direct his/her own health care
• Kind of care the person would want or not want if he/she unable
to make a decision
• Process of exploring Qs that often go unasked
• What give life meaning • Are there circumstances
• Loss physical functioning • Loss mental awareness
ACP – Role of health worker
• Health care workers should initiate ACP conversations –
Having those difficult conversations.
• Health care worker should encourage ACP. Not just for those
people facing life threatening conditions etc.
• Health care workers can and should be a support and resource
to people doing ACP.
• Health care workers should know how to assist an adult
person who wants to complete an ACP.
Ethical and Legal obligations
• Appropriate training to communicate effectively during ACP
discussions and to understand the legal and ethic issues involved.
• Basic level one training is free on line – easy ? 1.5 hours of
professional development
• www.advancedcareplanning.org.nz
• No one should be pressured – adults right to refuse • Consent to treatment must be obtained from a capable adult
• The fact that a person has an ACP and/or advanced directive –
NOT relevant as long as the person is capable of making his or her own decisions about care.
• The person: Fosters personal resolution, help to reduce
anxiety about what lies ahead.
• Confidence that wishes are known and will be followed
• Patients loved ones: Benefit of knowing what choices the
patient would have made
• Look back with the knowledge that they were able to honour
their family members wishes
• The health care worker: integrating ACP into routine clinical
encounters enables them to help pts families etc to prepare for the kinds of decisions they may face in future.
• Pre – course work
• Level one basic online training – print out certificates, bring with
you to the course
• When registered – ACP people send out pre-course workbook • Complete your own ACP
• Full course – 10 participants only
• 2.5 day course – full on!
• To complete the course, its compulsory to be there the whole time. • Compulsory to participate – ROLE PLAY • Role-play – You – 1 actor – one video player and the facilitator
• 4 others watching
Post course expectations
• Post course expectations
• Structure support group • Identify patients who would benefit from ACP • Initiate discussion and provide resources • Help patients to document their preferences • Keep a reflective log of the conversations • At ONE MONTH – need to have completed 10 conversations and
let the facilitators know.
• I sent in my reflective log to prove I had at least 10
• They send a certificate
• No anaemia nurse coordinators
• Physician to physician contact
• 1st prevent CKD • 2nd prevent complications of CKD • 3rd Management of CKD • Cognitive assessment of patients • Importance of advance care planning
• Alosco, M. L., Spitznagel, M. B., Raz, N., Cohen, R., Sweet, L. H., Colbert,
L. H., . . Gunstad, J. (2013). Executive dysfunction is independently
associated with reduced functional independence in heart failure. J Clin
Nurs. doi: 10.1111/jocn.12214
• Hayes, T. L., Larimer, N., Adami, A., & Kaye, J. A. (2009). Medication
adherence in healthy elders: small cognitive changes make a big
difference. J Aging Health, 21(4), 567-580. doi:
• Johnson DW, Atai E, Chan M, Phoon KS, Scott C, Toussaint ND, et al. KHA-
CARI Guideline: Early chronic kidney disease: detection, prevention and
management. Nephrology 2013; 18: 340-350
• KHA-CARI Guidelines www.cari.org.au and the New Zealand Primary
Care Handbook 2012 Revised October 2013
• Kidney health NZ. (2013) Chronic Kidney disease (CKD) Management in
general practice. Summary guide
• Thiruchselvam, T., Naglie, G., Moineddin, R., Charles, J., Orlando, L.,
Jaglal, S., . . Tierney, M. C. (2012). Risk factors for medication
nonadherence in older adults with cognitive impairment who live alone.
Int J Geriatr Psychiatry, 27(12), 1275-1282. doi: 10.1002/gps.3778
Source: http://www.nzirh.org.nz/wp-content/uploads/2013/03/GPs.pdf
SYRIAN ARAB REPUBLIC - MINISTRY OF ELECTRICITY PUBLIC ESTABLISHMENT FOR DISTRIBUTION OF ELECTRICITY SYRIAN ARAB REPUBLIC MINISTRY OF ELECTRICITY PUBLIC ESTABLISHMENT FOR DISTRIBUTION OF ELECTRICITY TENDER DOCUMENTS TECHNICAL SPECIFICATIONS Three Phase ACTIVE AND REACTIVE ENERGY MULTI-FUNCTION, MULTI-TARIFF STATIC METERS
ARTICLE IN PRESS Medical Engineering & Physics xxx (2006) xxx–xxx Photoacoustic monitoring of the absorption of isotonic saline solution by human mucus F.L. Dumas , F.R. Marciano , L.V.F. Oliveira , P.R. Barja , D. Acosta-Avalos a Instituto de Pesquisa e Desenvolvimento (IP&D), Universidade do Vale do Paraiba, Av. Shishima Hifumi 2911, CEP 12244-000, S˜ao Jos´e dos Campos, SP, Brazil