Print.ispub.com
The Internet Journal of Anesthesiology
Volume 29 Number 1
A Comparative Study Of Ondansetron And Granisetron For
Prevention Of Nausea And Vomiting Following
Laparoscopic Surgeries
A Chidambaram, K Bylappa, P Somasekaram
A Chidambaram, K Bylappa, P Somasekaram.
A Comparative Study Of Ondansetron And Granisetron For Prevention OfNausea And Vomiting Following Laparoscopic Surgeries. The Internet Journal of Anesthesiology. 2010 Volume 29 Number1.
Background and objectives Laparoscopic surgeries are associated with an appreciably high rate of post operative nausea andvomiting (PONV). This study was designed to compare the effectiveness of Ondansetron with that of Granisetron for preventionof PONV after laparoscopic surgery and their effect on clinical recovery and recovery time.Methods This is a randomizedprospective study of 60 adult patients of both sexes received either Ondansetron 4mg or Granisetron 2mg intravenously at theend of surgery. Perioperative anaesthetic care was standardized in all patients. Patients were then observed 24 hours afteradministration of the study drug.Results A complete response (defined as no PONV and no need for another rescue antiemetic)was achieved in 75% of the patients given ondansetron and 86% of the patients given granisetron with (p<.05%). No significantdifference observed in the recovery time from anesthesia between the two drugs and slight differences in the adverse eventswere observed between the two groups.Conclusion This study concludes that the prophylactic intravenous administration ofGranisetron is more effective drug than ondansetron for controlling postoperative nausea and vomiting with fewer incidences ofside effects.
vomiting is considerably high3.
Despite continuing advances in anesthetic and surgical
The introduction of 5-HT receptor antagonist was a major
techniques, both the incidence and severity of post-operative
advancement in the treatment of post operative nausea and
nausea and vomiting have remained relatively unchanged.
vomiting because of less adverse effects that were observed
Post operative nausea and vomiting are the most common
than commonly used traditional antiemetic4.
distressing symptoms occurring after surgery1. These factorsprevent patients returning home at the end of the day, after
Certain procedure such as middle ear surgeries, strabismus
surgery and necessitating readmission to the hospital. The
surgeries, laparoscopies, gynecological surgeries are
etiology of postoperative nausea, vomiting is complex and
associated with higher incidence of PONV5. Ondansetron is
depends upon a variety of factors, including patient
selective 5-hydroxy tryptamine receptor antagonist possess
characteristic, type of surgery, anaesthetic technique and
property of superior antiemetic prophylaxis6. This has been
postoperative care.
now used widely for the treatment of postoperative nauseaand vomiting7,8. Granisetron is recently introduced, 5-
Postoperative nausea and vomiting are more common in
hydroxy tryptamine receptor antagonist, with stronger 5HT
female patients1. Women undergoing Laparoscopic surgeries
binding. It is more potent and longer acting antemetic agent
are particularly at risk of experiencing these problems. It
compared to Ondansetron against emesis associated with
leads to dehydration and electrolyte imbalance. These factors
chemotherapy, and have been found to be very effective for
reduce the quality of life of the patients and interfering with
preventing PONV after laparoscopic surgery9. Granisetron
continuation of curative therapy2. So an effective antiemetic
has less incidence of side effects10.
therapy is needed. In the absence of any antiemetic treatmentfollowing laparoscopic surgery the incidence of nausea and
The aim of this clinical trial is to compare, the efficacy of
A Comparative Study Of Ondansetron And Granisetron For Prevention Of Nausea And Vomiting
prophylactic administration of 4mg Ondansetron i.v. with
was reversed with inj glycopyrollate 0.005mgkg-1 and
that of 2mg Granisetron i.v. administered at the end of the
neostigmine 0.05mgkg-1 and patient was extubated.
surgery in preventing PONV in patients undergoinglaparoscopic surgeries, their effect on clinical recovery and
The recovery time (in minutes) was measured from the time
recovery time and the side effects of Inj Ondansetron and Inj
nitrous oxide was switched off until the patient respond to
simple verbal commands. The patients were then assessedwith the help of a clinical recovery score, to compare effects
MATERIAL AND METHODS
on clinical recovery. The score consisted of simple questions
A randomized prospective study was conducted in 60 adult
to evaluate vigilance, cognition and orientation (Kumar et al
patients of class ASA I and ASA II, of either sex in age
group of 18-50yrs, weighing 45 to 70kgs, posted for
Laparoscopic surgery. The patients were randomly dividedinto two groups of 30 each: Group ‘A' – Ondansetron group
Unconscious, not arousable — 0
(n = 30), Group ‘B' – Granisetron group (n = 30). Patients
Unconscious, arousable by nociceptive stimuli — 1
belonging to ASA III and ASA IV, history of drug allergy,
Unconscious, arousable by verbal stimuli — 2
extremes of ages, obesity, history of motion sickness,
emergency surgeries, full stomach, respiratory diseases,
Awake, not attentive — 4
uraemia and Diabetes Mellitus where excluded .
Awake, attentive — 5
Ethical clearance and written informed consent was taken
from patients in both groups. The patients werepremedicated with 0.2mgkg -1 diazepam orally 12 hr before
No understanding of simple orders — 0
giving general anaesthesia. Patients were kept NPO for 12
Good understanding of simple orders — 1
hours before surgery. In the preoperative room, iv line was
secured. In the operation theatre routine monitoring devices,like pulse oximetry, NIBP, ECG monitors were attached;
and baseline blood pressure, heart rate and O saturation
values were recorded. Later capnography was attached after
Well oriented — 2
the intubation. The anaesthetic regimen and surgical
Evaluation by patient of his/her condition
procedures were standardized for all patients.
Uncomfortable — 1
Anaesthesia was induced with glycopyrollate 5µgkg-1 and
Comfortable — 2
intravenous thiopentone 5mgkg-1. For tracheal intubation
suxamethonium 2mgkg-1 was used. Anaesthesia wasmaintained with N20 66%, O 33%, halothane 0.5-2%;
Clinical Recovery Score
neuromuscular blockade with intermittent doses ofvecuronium bromide and analgesia with fentanyl 1.5µgkg-1.
11 : Excellent recovery
Ventilation was controlled mechanically and adjusted so as
9-10 : Good Recovery
to keep the end tidal carbon dioxide 35-40 mm of Hg.
8 : Fair recovery<8 : Poor recovery
Laparoscopic surgeries were performed under videoguidance. During surgery the patients were placed in
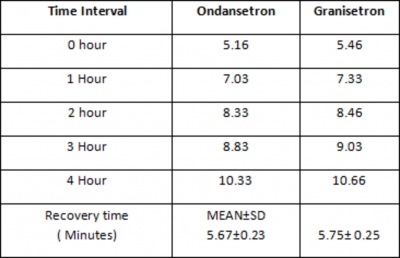
The clinical recovery score was assessed at 0, 1, 2, 3 and 4
trendlenburg position wherever required and the abdomen
hours after patient's arrival in recovery room and
was insufflated with carbon dioxide with an intra abdominal
assessments were made and appropriate recording was done.
pressure of 12-15 mm of Hg. At the end of the surgery
In post anaesthesia care unit blood pressure and heart rate
Group I patients received 4mg Inj ondansetron and Group II
was recorded every 10 min for 30 min. Episodes of nausea
patients received 2mg Inj. granisetron administered slow iv
and vomiting experienced by each patient were recorded by
over period of 30 seconds. At the cessation of surgery
direct questioning. The number of patients who suffered
patients were made supine and residual neuromuscular block
A Comparative Study Of Ondansetron And Granisetron For Prevention Of Nausea And Vomiting
nausea/vomiting was noted during the period's 0-4hrs,
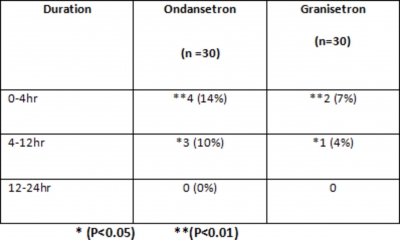
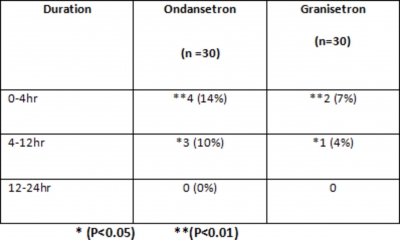
cases (14%) as compared to 2 cases (7%) in granisetron
4-12hrs, 12-24hrs. Rescue Antiemetic (inj. metaclopramide
group in 0-4 hours(P<0.01). In 4-12 hours ondansetron
10mg) was used if patient had vomiting.
group had 3 cases(10%) of incidence of vomiting ascompared to 1 case (4%) in granisetron group(P<0.05).
Any adverse reactions of the drug like headache, dizziness,
Again the incidence of vomiting was maximum during first
hypersensitivity, constipation if any was noted in the 24 hr
four hours and no patient in any group vomited from 12
study period. Statistical analysis was done using student‘t'
hours onwards. (table: 5).
test. A ‘P' value of less then 0.05 will be considered to besignificant
Need for rescue antiemetic is more in Ondansetron groupthat is 7 (23 %) compared to Granisetron group 3 (10 %).
RESULTS AND ANALYSIS
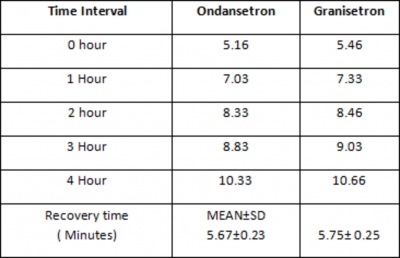
There was no significant difference in CRS and RT between
Total 60 patients were included in this study. Patient
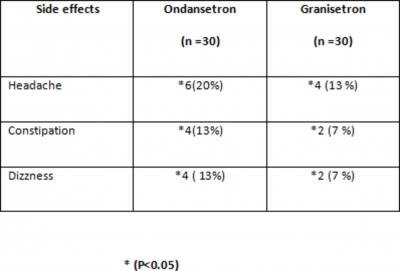
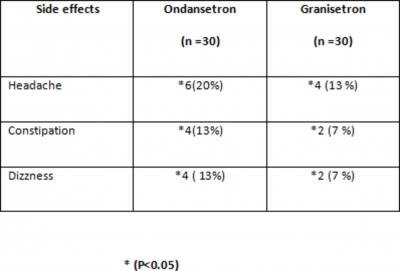
the two groups as shown in (table: 6). Occurrence of side
populations were comparable across the two groups with
effects like headache, constipation and dizziness in
respect to Age, Weight, Systolic BP, Diastolic BP, Heart
Ondansetron group are 6(20%),4(13%),4(13%) respectively
rate. Statistical analysis was done by using student ‘t'test
compared to 4 (13%), 2(7%),2 (7 %) in Granisetron group.
and rest of the study data have been categorically analyzed.
The number of patients who suffered side effects was morein Ondansetron group. As shown in (table: 7).
In our study most of the patients in both groups belonged toage group 18-30. In both the groups females predominated
males : in Ondasetron group male were 7 (23%) and females
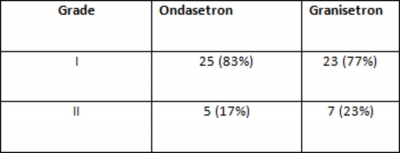
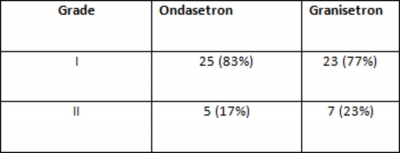
Table: 1 asa grade wise
23 (77%) and in Granisetron group male were 5 (17%) andfemales 25 (83%).
There was no significant weight difference between the twogroups: in Ondasetron group 45-60 kg - 20 (67%), 61-70kg -10 (33%); in Granisetron group 45-60 kg - 23 (77%), 61-70kg 7(23%). Mean weight ±SD of Group A was 56.93±10.62and in Group B 50.86±10.85. Both groups had almostsimilar numbers of ASAI and ASAII as shown in (table: 1).
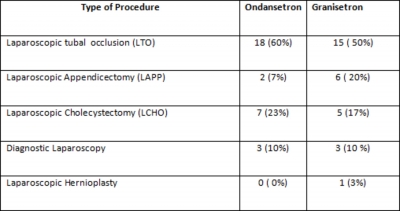
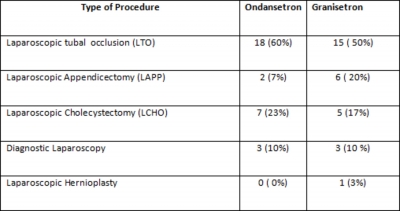
In our study Laparoscopic tubal occlusion (LTO)
Table: 3, comparision of systolic bp, diastolic bp, hr and
predominated in both groups than any other surgery as
shown in (table: 2). Systolic, Diastolic BP , Heart rate andoxygen saturation showed no statistically significantdifference recorded in PACU between the study groups asshown in (table:3)
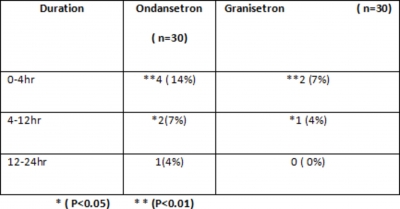
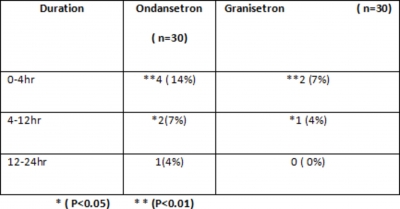
Occurrence of nausea in Ondanstron group and Granisetrongroup showed that incidence of nausea in 0-4 hours were 4cases (14%)in Ondansetron group as compared to 2 cases(7%) in Granisetron group(P<0.01). Incidence of nausea in4-12 hours were 2 cases (7%)in Ondansetron group ascompared to 1 cases (4%) in Granisetron group(P<0.05).
Incidence of nausea in 12-24, hours was only 1 case (4%) inOndansetron group as compared to 0 cases (0%) inGranisetron group. The incidence of nausea was greatestduring the first four hours and it was more in theOndansetron group. (Table: 4)
Incidence of vomiting episodes in Ondansetron group were 4
A Comparative Study Of Ondansetron And Granisetron For Prevention Of Nausea And Vomiting
Table: 4, incidence of nausea
Table: 7 , comparison of side effects
Figure 5
Table:5, incidence of vomiting
DISCUSSION
Postoperative nausea and vomiting (PONV) is of
multifactorial origin. The incidence of PONV after
anaesthesia, despite the advances in antiemetic therapy in the
last decades is still found to be relatively high. The three
most common causes for admission following day care
surgery are pain, bleeding and intractable vomiting1. Factors
affecting PONV include patient related factors (age, sex,
phase of the menstrual cycle), anaesthesia related factors
(use of volatile anesthetic agents, N O, Opioid) and surgery
related factors1. Female gender has been associated with
Table: 6, clinical recovery score (CRS) and recovery time
higher incidence of PONV compared to male patients.1, 2 On
an average, female patients suffer three times more oftenfrom PONV than men2.
Our study was aimed at comparing the antiemetic efficacy ofOndansetron and Granisetron in preventing PONV inlaparoscopic surgery. In our study the factors that wouldhave contributed to nausea and vomiting may belaparoscopic surgery, use of Halothane, use of Fentanyl etc.
Use of facemask, use of Nitrous Oxide may or may not havecontributed to nausea and vomiting. Avoidance of Pethidinetowards the end of surgery must have helped in preventingPONV3.
Laparoscopic surgery was chosen because of high incidenceof PONV associated with it. Naguib et al demonstrated thatthe incidence of PONV after laparoscopic surgeries in theirplacebo group was remarkably high (72%).11
We have conducted studies on 60 patients of ASA I and II
A Comparative Study Of Ondansetron And Granisetron For Prevention Of Nausea And Vomiting
with demographic data in terms of age, weight, which were
According to Gigilla20 it shows that some haemodynamic
similar in the two groups. There was no significant
variation in SBP, DBP and HR. Ondansetron mediated
difference in Ondansetron and Granisetron (P< 0.05) in
bradycardia and hypotension was reported in that study
terms of Age and Weight. Study done by Pearman12 shows
group. Kumar et al21 in their clinical trial on recovery score
that postoperative nausea and vomiting is more common in
and recovery time showed slightly lower clinical recovery
young age group and obese patients.
scores with metoclopramide group compared to ondansetronwhich may be attributed to its established unpleasant
Incidence of nausea in our study group was 25% in
sedative pharmacological activity. They did not notice any
Ondansetron group, 11% in Granisetron group. Present study
significant difference in the overall incidence of drowsiness
shows highly significant difference in first 0-4hr (P < 0.05).
or sedation in both the groups. They further stated that
While in 4-12hrs incidence of nausea shows marginally
ondansetron does not affect patients vigilance, cognition or
significant difference. After 12-24hrs, there was no
orientation and concluded that ondansetron (4 mg) and
significant difference in nauseating episodes. Study done by
metoclopramide (10 mg) do not affect the cognitive aspects
Pueyo13 observed that nausea and vomiting is more common
following major gynaecological surgery.
in first 6 hours post operatively. Same results are seen in thestudy done by Fujii 14.
In our study on the clinical recovery score and the recoverytime we observed slightly lower clinical recovery score in
According to Raphael15, optimal dose of Ondansetron for
the Ondansetron group compared to Granisetron and there
preventing post operative nausea vomiting is 4 mg and half
was not much of significant difference in the recovery time.
life is 3 hours. While optimal dose of Granisetron is 2 mg
Incidence of side effects was significant in our study groups.
and half life is 8-9 hours. So it is observed that after 6 hours
Incidence of headache was 20% in Ondansetron group while
Granisetron is more effective than Ondansetron for
it was 12% in Granisetron group shows statistically
preventing PONV. Vomiting in the present study group was
significant difference (P < 0.05).
24% in Ondansetron and 11% in the Granisetron group. Inour study group incidence of vomiting was highly significant
According to study by Mitra 22, incidence of headache and
in first 4hrs (P<0.01). Present study showed that Granisetron
constipation is more in Ondansetron group as compared to
is better than Ondansetron for preventing PONV.
Granisetron group which matches with our results. Incidence
Bhattacharya16 in his study observed same results.
of constipation and dizziness also shows significantdifference in Ondansetron and Granisetron groups (P <0.05).
During 0-4hr and 4-12hrs postoperatively results aresignificant in nature (P< 0.05). After 12hrs, result of
The use of rescue antiemetic in ondansetron group which
vomiting was insignificant (P>0.05). Janknegt studied that if
was about 7(23%) whereas in Granisetron group about
Ondansetron is given at the induction time, it is ineffective
3(10%) of the patients received rescue antiemetic. Stewart23
in preventing PONV17, so we administered study drug half
in his study also has same result. Updated guidelines for
an hour before end of the surgery. This makes the drugs to
managing postoperative nausea and vomiting were recently
be effective postoperatively for longer time. Sinha18
announced at the 2006 Annual Meeting of American Society
concluded the same results in his study.
of Anaesthesiologists in Chicago, Illinois, USA. Evaluatingthe current medical literature, they recommended the use of
Our study shows no statistically significant difference in the
antiemetics, with an emphasis on the use of the 5HT3
baseline values of haemodynamic variables between the two
groups before, during or after giving study drug. Study drugsOndansertron and Granisetron was given approximately half
The guidelines also suggest a potential benefit of
an hour before the end of the surgery. In PACU we have
combination prophylaxis. Overall the panel recommended,
recorded the SBP, DBP and HR over a period of 30min at
"prophylactic therapy with combination, three or more
regular interval. According to our study there was no
interventions, in patients at high risk for PONV.24 So we
haemodynamic alteration between these results. Study
have studied the effect of Granisetron 2mg i.v. versus
conducted by Dev19 also shows the same results. There is no
Ondansetron 4mg i.v, administered to the patients, who had
haemodynamic alteration seen in PR, SBP and DBP during
undergone laparoscopic surgery under general anaesthesia.
study period.
A Comparative Study Of Ondansetron And Granisetron For Prevention Of Nausea And Vomiting
emetogenic chemotherapy : A multicentre double blind
randomized parallel study. J Clin Oncol 1981; 6: 754-60.
Our study concludes that the prophylactic intravenous
10. Toyooka H, Tanaka H: Oral granisetron prevents
administration of Granisetron is more effective drug than
postoperative vomiting in children. BJA 1998; 81: 390-99.
11. Naguib M, EI Bakry AK, Khoshim MHB et al.
Ondansetron for controlling postoperative nausea and
Prophylactic antimetic therapy with Ondansetron,
vomiting with fewer incidences of side effects.
Tropisetron, Granisetron and metoclopramide in patients
undergoing laparoscopic cholecystectomy. Can J Anaesth
Safety profile is more with Granisetron and it is more potent
1996; 43: 226-31.
12. Pearman M.H. Single dose intravenous ondanestron in
than Ondansetron. So we observed minimal emetic and
the prevention of postoperative nausea and vomiting.
nausea episodes in postoperative period in patients who had
Anaesthesia 1994; 49: 11-15.
13. Paxton DL, McKay CA. Prevention of nausea and
received i.v. Granisetron in comparison to i.v. Ondansetron,
vomiting after day care gynaecological laproscopy.
undergoing laparoscopic surgery under general anaesthesia.
Anaesthesia 1995; 50: 403-46.
14. Fujii Y, Tanaka H, Toyooka H. Granisetron reduces
Even though there was slightly higher clinical recovery score
vomiting after strabismus surgery and tonsillectomy in
children. Can J Anaesth 1996; 43: 35-38.
in the patients who had received intravenous Granisetron
15. Raphael JH, Norton AC. Anitemetic efficacy of
compared to patients who had received intravenous
prophylactic Ondansetron in laproscopic surgery.
Ondansetron, there was no significant difference in the
Randomized double blind comparison with metoclopramide.
BJA 1993; 71: 845-48.
recovery time from anaesthesia between the two drugs.
16. Bhattcharya D, Banerjee A. Comparison of Ondansetron
and Granisetron for prevention of nausea and vomiting
following day care gynecological laproscopy. Ind J Anesth
2003; 47: 279-82.
1. Gold BS, Kitz PS, Lecky JA. Unanticipated admission to
17. Janknegt R. Clinical efficacy of antiemetic following
the hospital following ambulatory surgery. JAMA 1989;
surgery. Anaesthesia 1999; 54: 1054-68.
262: 3008-10.
18. Sinha PK, Sushil P. Ondansetron in prophylaxis of
2. Bondner M, Honkovaara P. Nausea and vomiting after
postoperative nausea and vomiting in patients undergoing
gynaecological laparoscopy depends upon the phase of the
breast surgery: A placebo-controlled double blind study. J
menstrual cycle. Can J Anaesthesia 1991; 38: 876-87.
Ind Med. Assoc 2004; 102.
3. Kortillo K. The study of PONV. BJA 1992; 69(Suppl-1):
19. Dev N, Mehrotra S, Tyagi S K. A comparative study of
metoclopramide and ondansetron. Ind J Anaesth 1998; 42:
4. Bunce K.T, Tyers MB. The role of 5-HT in post operative
nausea and vomiting. BJA 1992; 69(S): 60-62.
20. Gigilla CA, Soares H. Granisetron is equivalent to
5. Lerman J. Surgical and patient factors involved in post
Ondansetron for prophylaxis of chemotherapy induced
operative nausea and vomiting. BJA 1992; 69: 245-325.
nausea and vomiting. Cancer 2000; 89: 2301-08.
6. Helmy.S.A.K, Abdul W. Prophylactic antiemetic efficacy
21. Kumar A. Effect of ondansetron and metocloparmide on
of ondansetron in laparoscopic cholecystectomy under total
vigilance, cognition and recovery time following major
intravenous anaesthesia. Anaesthesia 1995; 54: 266-69.
gynacecological surgery. J Anaesth Clin Pharmacol 1996;
7. Mckenzie R, Tantisira B, Deepa. Comparision of
ondanestron in the prevention of postoperative nausea and
22. Mitra S, Sharma S, Tak V. Prophylatic antiemetic for
vomiting. Anesth Analg 1994: 79: 961-64.
laparoscopic cholecystectomy; Ondansetron versus
8. Richard A, Steinbrook, Janes L, David . Prophylatic
metoclopramide. Ind J Anaesth 1999; 35: 43-45.
antiemetics for Laparoscopic cholecystectomy: Ondansetron
23. Stewart L, Crawford S.M. The comparative effectiveness
versus Droperidol plus Metoclopramide. Anesth Analg
of ondansetron and granisetron on once daily dosage in
1996; 83: 1081-83.
prevention of nausea and vomiting caused by cisplatin. The
9. Peyez EA, Hasketh P, Sandback J, Chawla S.Comparison
Pharmaceut J 2001; 265(104): 59-62.
of single dose oral Granisetron Vs IV Ondansetron in the
24. New guidelines issued for PONV: http://www.
prevention of nausea and vomiting induced by moderately
anesthesianow.com/news. cited on November 22, 2006.
A Comparative Study Of Ondansetron And Granisetron For Prevention Of Nausea And Vomiting
Author Information
Ananth Chidambaram, MBBS., MD
Department of Anaesthesiology, Chennai Medical College Hospital and Research Center
Kiran Bylappa, MBBS., MS
Department of Otorhinolaryngology, Sapthagiri Institute of Medical Sciences & Research Center
P. Somasekaram, MBBS., MD
Professor and HOD, Department of Anaesthesiology, Sri Devaraj Urs Medical College
Source: http://print.ispub.com/api/0/ispub-article/3679
SPEAKING FOR THE SALMON SUMMIT OF SCIENTISTS ON AQUACULTUREAND THE PROTECTION OF WILD SALMON JANUARY 25-27, 2007 INNER COAST NATURAL RESOURCE CENTRE and LAWRENCE AMBERS RECREATION CENTRE ALERT BAY, BC Rick Routledge, Patricia Gallaugher, and Craig Orr The conveners wish to thank the ‘Namgis First Nation, the Village of Alert Bay and the Inner Coast Natural Resource Centre for their support in making the workshop possible, and to the ‘Namgis First Nation for welcoming us into their territory and sharing their culture.
Cutaneous and renal glomerular vasculopathyas a cause of acute kidney injury in dogsin the UK L. P. Holm, I. Hawkins, C. Robin, R. J. Newton, R. Jepson, G. Stanzani, L. A. McMahon,P. Pesavento, T. Carr, T. Cogan, C. G. Couto, R. Cianciolo, D. J. Walker To describe the signalment, clinicopathological findings and outcome in dogs presenting withacute kidney injury (AKI) and skin lesions between November 2012 and March 2014, in whomcutaneous and renal glomerular vasculopathy (CRGV) was suspected and renal thromboticmicroangiopathy (TMA) was histopathologically confirmed. The medical records of dogs withskin lesions and AKI, with histopathologically confirmed renal TMA, were retrospectivelyreviewed. Thirty dogs from across the UK were identified with clinicopathological findingscompatible with CRGV. These findings included the following: skin lesions, predominantlyaffecting the distal extremities; AKI; and variably, anaemia, thrombocytopaenia andhyperbilirubinaemia. Known causes of AKI were excluded. The major renal histopathogicalfinding was TMA. All thirty dogs died or were euthanised. Shiga toxin was not identified in thekidneys of affected dogs. Escherichia coli genes encoding shiga toxin were not identified infaeces from affected dogs. CRGV has previously been reported in greyhounds in the USA,a greyhound in the UK, without renal involvement, and a Great Dane in Germany. This is thefirst report of a series of non-greyhound dogs with CRGV and AKI in the UK. CRGV is a disease ofunknown aetiology carrying a poor prognosis when azotaemia develops.