Matrix-associated stem cell transplantation (mast) in chondral defects of the 1st metatarsophalangeal joint is safe and effective—2-year-follow-up in 20 patients

FAS-937; No. of Pages 6
Contents lists available at
Foot and Ankle Surgery
Matrix-associated stem cell transplantation (MAST) in chondral
defects of the 1st metatarsophalangeal joint is safe and
effective—2-year-follow-up in 20 patients
Martinus Richter MD, PhDStefan Zech MD, Stefan Andreas Meissner MD
Department for Foot and Ankle Surgery Rummelsberg and Nuremberg, Germany
The aim of the study was to assess the 2-year-follow-up of matrix-associated stem cell transplantation
Received 3 October 2015
(MAST) in chondral defects of the 1st metatarsophalangeal joint (MTPJ).
Received in revised form 9 May 2016
In a prospective consecutive non-controlled clinical follow-up study, 20 patients with 25 chondral
Accepted 11 May 2016
defect at the 1st MTPJ that were treated with MAST from October 1st, 2011 to March, 30th, 2013 were
analysed. The size and location of the chondral defects range of motion (ROM), and the Visual-Analogue-
Scale Foot and Ankle (VAS FA) before treatment and at follow-up were registered.
Stem cell-rich blood was harvested from the ipsilateral pelvic bone marrow and centrifuged (10 min,
1500 RPM). The supernatant was used to impregnate a collagen I/III matrix (Chondro-Guide). The matrix
Matrix-associated stem cell transplantation
was fixed into the chondral defect with fibrin glue.
1st metatarsophalangeal joint
The age of the patients was 42 years on average (range, 35–62 years). The VAS FA before surgery was
50.5 (range, 18.3–78.4). The defects were located as follows, dorsal metatarsal head, n = 12, plantar
metatarsal head, n = 5, dorsal & plantar, n = 8 (two defects, n = 5). The defect size was 0.7 cm2 (range, .5–
2.5 cm2). ROM was 10.3/0/18.88 (dorsal extension/plantar flexion). All patients completed 2-year-
follow-up. VAS FA improved to 91.5 (range, 74.2–100; t-test, p < .01). ROM improved to 34.5/0/25.5
The surgical treatment including MAST led to improved clinical scores and ROM. Even though a
control group is missing, we conclude that MAST is a safe and effective method for the treatment of
chondral defects of the 1st MTPJ.
! 2016 European Foot and Ankle Society. Published by Elsevier Ltd. All rights reserved.
a modification of AMIC with a potentially higher concentration of
stem cells in the implanted matrix, and also as a completely new
The optimal treatment for chondral defects at foot and ankle is
method Most of these methods have been used for chondral
debatable. The current options are distraction, debridement,
defects at the ankle MAST was also used for the 1st
abrasion, microfracture, antegrade or retrograde drilling, mosaic-
metatarsophalangeal joint (MTPJ) with encouraging initial results
plasty or osteochondral autograft transfer system (OATS), autolo-
The aim of the study was to assess the 2-year-follow-up of
gous chondrocyte implantation (ACI), matrix-induced autologous
MAST in chondral defects of the 1st MTPJ.
chondrocyte implantation (MACI), autologous matrix-induced
chondrogenesis (AMIC), allologous stem cell transplantation,
allograft bone/cartilage transplantation, or matrix-associated
stem cell transplantation (MAST) . MAST was described as
MAST was performed as single open procedure associated with
* Corresponding author at: Department for Foot and Ankle Surgery Rummelsberg
other procedures. The other procedures included the standard joint
and Nuremberg, Location Hospital Rummelsberg, Rummelsberg 71, 90592 Schwar-
preserving surgical management for hallux rigidus like cheilect-
zenbruck, Germany. Tel.: +49 9128 50 43450; fax: +49 9128 50 43260. Homepage:
omy, synovectomy, arthrolysis and tenolysis . Stem cell-
www foot surgery eu.
rich blood was harvested during the procedure from the ipsilateral
E-mail addresses:
(M. Richter).
pelvic bone marrow with a Jamshidi needle (10 ! 3 mm, Cardinal,
1268-7731/! 2016 European Foot and Ankle Society. Published by Elsevier Ltd. All rights reserved.
Please cite this article in press as: Richter M, et al. Matrix-associated stem cell transplantation (MAST) in chondral defects of the 1st
metatarsophalangeal joint is safe and effective—2-year-follow-up in 20patients. Foot Ankle Surg (2016),

FAS-937; No. of Pages 6
M. Richter et al. / Foot and Ankle Surgery xxx (2016) xxx–xxx
Dublin, OH, USA) and a special syringe (Arthrex-ACP1, Arthrex,
Analogue Scale Foot and Ankle (VAS FA) was registered . The
Naples, FL, USA) through a stab incision. The syringe was
defect size and location was assessed intraoperatively. The
centrifuged (10 min, 1500 rotations per minute). The supernatant
defects were classified as dorsal when located above a virtual
was used to impregnate a collagen I/III matrix (Chondro-Guide1,
horizontal line at 50% of the metatarsal head height or diameter;
Geistlich, Baden-Baden, Germany) that was cut to the size of the
plantar when located below that line, or both when crossing
cartilage defect before. The cartilage defect was debrided until
the line. The following parameters were registered at 2-year-
stable surrounding cartilage was present. Microfracturing with a
follow-up: VAS FA, ROM, radiographic hallux rigidus stage and
1.6 mm Kirschner wire was performed. The matrix with stem cells
was fixed into the chondral defect with fibrin glue (Tissucoll,
Deerfield, IL, USA). An 8Ch drainage was inserted without suction.
Closure was performed following the local standard with layer
wise closure (joint capsule, subcutaneous, skin). The postoperative
Standard dynamic pedography (three trials, walking, third
treatment included full weight bearing without orthosis or splint.
step, mid stance force pattern) was performed as described before
Motion of the joint with MAST was restricted for two days, and
. A standard platform (Emed AT1, Novel Inc., Munich,
physiotherapy with motion of this joint was started at day three
Germany & St. Paul, MN, USA) and software (Emed ST1, version
after surgery. The patients were instructed to perform motion of
12.3.18, Novel Inc., Munich, Germany & St. Paul, MN, USA) was
the joints with MAST 10 times a day for 10 min. Postoperative
used. Both sides were measured. Computerised mapping to create
consultations were performed at 6 weeks, 3, 12 and 24 months.
a distribution into the following foot regions was performed with
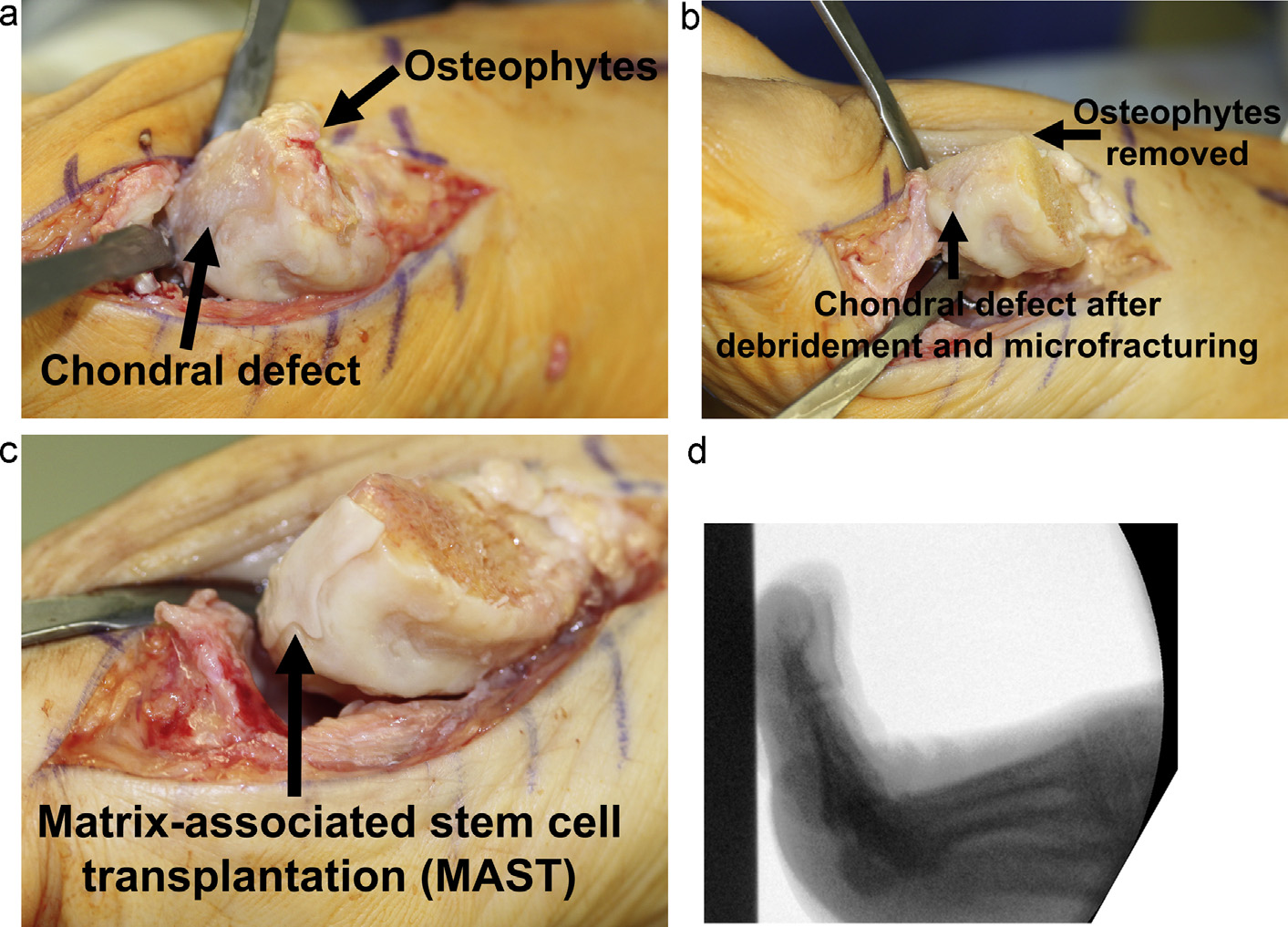
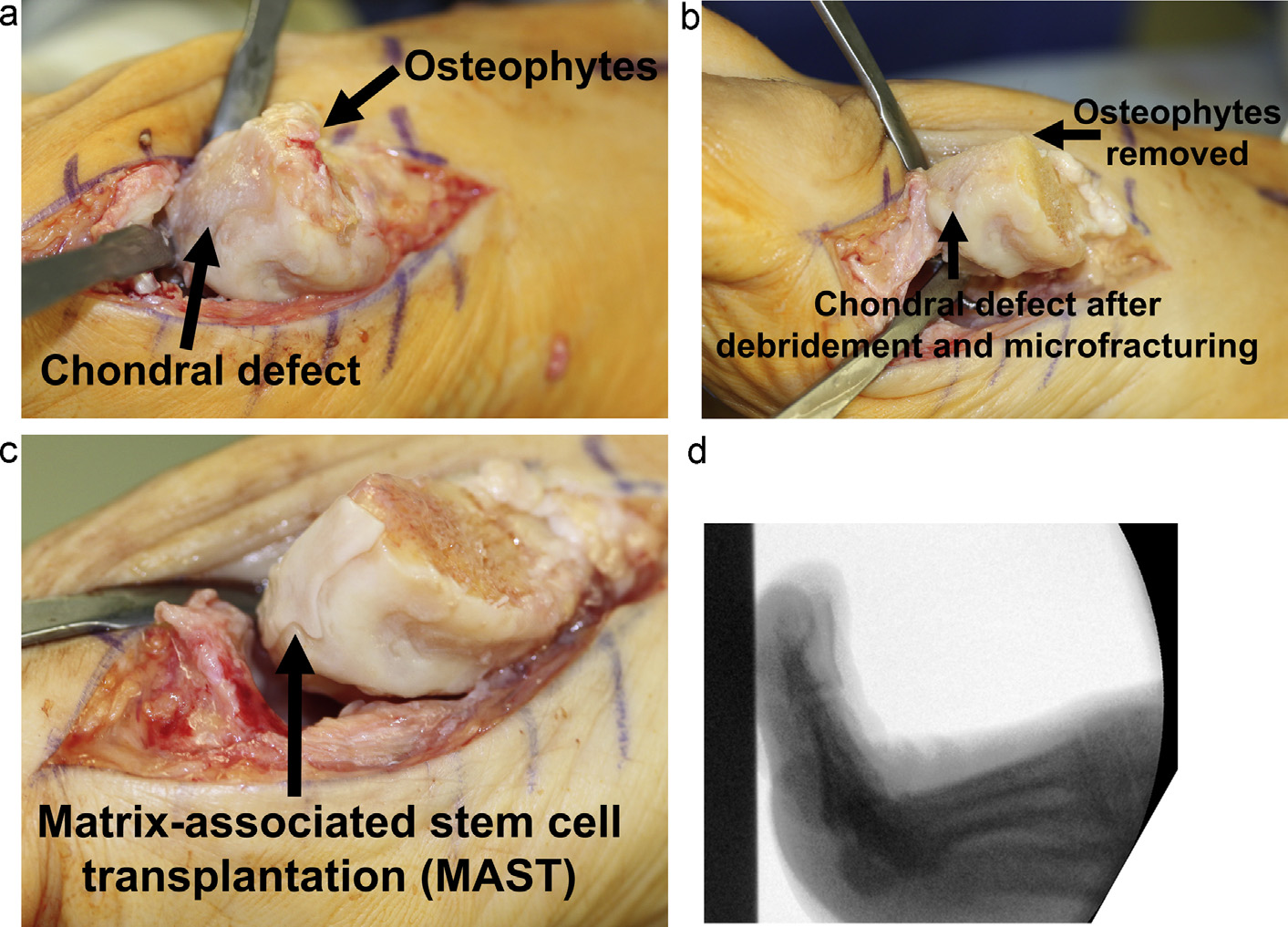
show a typical case.
the standard software (Automask, version 12.3.18, Novel Inc.,
Munich, Germany & St. Paul, MN, USA): hindfoot, midfoot, 1st
2.2. Study design
metatarsal head, 2nd metatarsal head, 3rd metatarsal head, 4th
metatarsal head, 5th metatarsal head, 1st toe, 2nd toe, 3rd–5th toe.
In a prospective consecutive non-controlled clinical follow-up
This mapping process does not include manual determination of
study, 20 patients with 25 chondral defect at the 1st MTPJ that
landmarks Parameters of 1st metatarsal head and 1st toe
were treated with MAST from October 1st, 2011 to March, 30th,
were compared preoperative versus follow-up
2013 were analysed. The single inclusion criteria for the study was
A paired t-test was used for statistical comparison of VAS FA and
the described procedure. Patients with bilateral treatment (n = 15)
maximum pedographic pressures preoperatively and at follow-up,
or with corrective osteotomies for hallux valgus correction or
and a Chi2-test for all other parameters. Before using the paired t-
others (n = 57) were excluded. No other exclusion criteria were
test, the data were investigated regarding the distribution and the
defined. Range of motion (ROM) was measured clinically with a
data were proven to be normally distributed.
goniometer. All patients had radiographs (bilateral views (dorso-
plantar and lateral) full weight bearing). The degenerative changes
were classified in four degrees . Pedography was performed as
described below. There were no limitations in terms of patient's
Twenty patients with 25 defects were included in the study.
age and defect size. There was no clear and objective definition
The age at the time of surgery was 42 years on average (range,
regarding the combination of defect size, location and age. The
35–62 years), 14 (70%) were male. The VAS FA before surgery was
indication for the procedure was based on patient history, clinical
50.5 on average (range, 18.3–78.4). In 12 cases (60%), the right
investigation and radiographic findings (Stage 1–3) . Stage
foot was affected. shows the radiographic hallux rigidus
4 was considered as contraindication for the procedure. Visual
stage. The most common stage was 2 (n = 9, 45%). Mean ROM was
Fig. 1. (a and b) Case with hallux rigidus stage 2. 45-year-old female; VAS FA 56.2; ROM dorsal extension/plantar flexion 10/0/208.
Please cite this article in press as: Richter M, et al. Matrix-associated stem cell transplantation (MAST) in chondral defects of the 1st
metatarsophalangeal joint is safe and effective—2-year-follow-up in 20patients. Foot Ankle Surg (2016),

FAS-937; No. of Pages 6
M. Richter et al. / Foot and Ankle Surgery xxx (2016) xxx–xxx
Fig. 2. (a–d) Hallux rigidus stage 2 (same case as with typical dorsal osteophytes and dorsally located chondral defect (1 ! 2 cm = 2 cm2; (a)). Subpart b shows the situs
after removal of the osteophytes (medial and cheilectomy), debridement of the chondral defect and microfracturing. Subpart c shows the implanted MAST. Subpart d shows a
lateral intraoperative fluoroscopic image with possible 908 dorsal extension in the MTPJ.
10.3/0/18.88 for dorsal extension/plantar flexion. shows
replacement. All patients completed 2-year-follow-up. VAS FA
the pedographic parameters. The maximum pressure was
improved to 91.5 (range, 74.2–100; t-test, p < .01). ROM
237.7 kPA at the MTPJ and 807.1 kPa at the 1st toe on average.
improved to 34.5/0/25.5 (dorsal extension & plantar flexion,
The defects were located as follows, dorsal metatarsal head,
p < .01). The radiographic hallux rigidus stage decreased
n = 12, plantar metatarsal head, n = 5, dorsal & plantar, n = 8 (two
(Chi2-test, p < .01) Stage 2 was the most common preoperative-
defects, n = 5). The defect size was 0.7 cm2 (range, .5–2.5 cm2).
ly, and stage 1 at 2-year-follow-up (The maximum
No complications or consecutive surgeries were registered until
pressure and the percentage of maximum force of the maximum
follow-up, i.e. no patient was converted to fusion or total joint
force of the entire foot increased at the 1st MTPJ and decreased at
Fig. 3. (a and b) Case with preoperative hallux rigidus stage 2 at two-year-follow-up (same case as ). 47-year-old female; VAS FA 92.4; ROM dorsal extension/
plantar flexion 40/0/308. Hallux rigidus stage was classified 0 at follow-up.
Please cite this article in press as: Richter M, et al. Matrix-associated stem cell transplantation (MAST) in chondral defects of the 1st
metatarsophalangeal joint is safe and effective—2-year-follow-up in 20patients. Foot Ankle Surg (2016),

FAS-937; No. of Pages 6
M. Richter et al. / Foot and Ankle Surgery xxx (2016) xxx–xxx
the cells, and the MAST includes a typical centrifugation (1500 RPM
Radiographic hallux rigidus stage preoperatively and at 2-year-follow-up.
for 10 min) that potentially doubles the concentration of stem cells
in the supernatant to 6% . As in MACI, MAST uses a carrier or
scaffold for the cells . Different scaffold are available, some with
hyaluronic acid, and others with collagen . The introduced
method includes a collagen matrix (Chondro-Guide1, Geistlich,
Baden-Baden, Germany) . This scaffold is manufactured out of
denaturated collagen from the pig, and contains collagen I and III.
The matrix has two layers (bilayer). The superficial layer is water
proof, and the deep layer is porous . The superficial, water proof
the 1st toe (, all p < .01) when comparing preoperative
layer should maintain the cell fluid in the defect, and the deep,
porous layer should contain and maintain the cells, and should
integrate in part with the underlying subchondral bone The
microfracturing is added to add cells and supply from the underlying
bone (marrow), as use in microfracture alone . The fibrin glue is
added to give sufficient initial stability for early functional after
Cheilectomy, synovectomy, arthrolysis and tenolysis are the
treatment Our strategy is to fit the matrix as exact and as stable
standard procedure for joint preserving surgery in hallux rigidus
as possible The main advantage of MAST in comparison with ACI
. These studies have shown good but not optimal results
and MACI is the single procedure methodology and lower cost
Reasons for suboptimal results were remaining pain
. The advantage in comparison with AMIC is the potential higher
and functional restrictions Later conversion to arthrod-
concentration of stem cells . The advantage of the Chondro-
esis were described in up to 16% in the short- to midterm follow-up
Guide1 in comparison with other scaffolds/matrices used (hya-
. As attempt to improve the outcome, we added MAST for the
luronic acid) is the more physiological content and structure . This
chondral defect(s) based on our previous experience with MAST
matrix gives the initial stability to allow the early stimulation of the
and hallux rigidus surgery Despite many studies focused on
transplanted cells by motion which induces the determination of the
treatment of cartilage defects at the ankle, no such methods were
transplanted stem cells into chondrocytes Furthermore, it gives
utilised for the MTPJ so far Furthermore, the use of these
the collagen scaffold which seems to be extremely difficult to
methods in other joints of the foot have not been described so far
determine from stem cells by an in vivo stimulation
Very recently, one study dealing with implantation of synthetic
cartilage in the 1st MTPJ was published showing good results .
4.1. Technical issues
Our results are favourable and no adverse effects have been
registered. The scores improved, ROM increased, and the pedo-
We consider MAST as a combination of stem cell transplantation
graphic parameters were normalised. This is the first study
and AMIC . An almost similar method was introduced for the
including validated functional investigation based on pedography
ankle as completely novel method . The advantage in compari-
as far as we are aware, and improvement of the investigated
son with AMIC which uses peripheral blood is the higher
function (gait stance phase) was shown. The radiographic hallux
concentration of pluripotent cells or stem cells. No one knows the
rigidus stage as proposed by Shereff was decreased at follow-up
exact concentration of stem cells which varies for different age and
when compared with the preoperative stage . This classifica-
location . Rough estimations name 0.1% stem cells as
tion is based on radiographs, and is focused on extent of
concentration in the peripheral blood and 3% in the pelvic bone
osteophytes and joint space. It is not surprising at all that removal
marrow in young adults . This deduces that the cells should
of osteophytes and cheilectomy changes the extend of osteophytes
be harvested from the pelvic bone marrow which is part of MAST
which is part of the classification. However, the width of the joints
Centrifugation is a useful method to double the concentration of
space which is also part of the classification was also changed, i.e.
widened on average at 2-year-follow-up (example ).
We think that the MAST procedure and not the osteophyte
Pedographic parameters preoperatively and at 2-year-follow-up.
removal/cheilectomy is the reason for the joint space widening.
The widening of joint space after implantation of ‘‘scaffold and
cells'' was not described for the ankle, 1st MTPJ and other joints
MTPJ, percentage maximum
before as far as we know. The used classification does not give any
force of entire foot (%)
direct information about the cartilage as such as sufficient MRI
with thin slice thickness could give. We would be extremely
interested in histological specimens of the transplants. However,
no patient was undertaken surgery again so far in which
histological specimens could have been harvested. Earlier histo-
1st toe, percentage maximum
logical assessment from specimens from the talus gave anecdotal
force of entire foot (%)
but clear evidence that the transplanted cells could develop or
better determine into chondrocytes, and that the implanted
1st toe, maximum pressure (kPa)
collagen matrix stayed in place and acts as a scaffold for the
chondrocytes as in ‘‘real'' cartilage
MTPJ, 1st metatarsophalangeal joint. The individual percentages of the maximum
Only one of the above mentioned studies dealing with cartilage
force of the entire force represent the percentage of the maximum force measured
restoration addressed the 1st MTPJ, and none included a validated
in the in the corresponding area (MTPJ or 1st toe) of the maximum force of the entire
outcome score which makes a comparison with our results difficult
force (100% means that the maximum force of the corresponding area is similar to
from a scientific point of view The single study addressing the
the maximum force of the entire foot). The individual maximum pressure values
mean values of the maximum pressure measured in the three
1st MTPJ compared implantation of ‘‘synthetic cartilage'' with
different trial in the corresponding area (MTPJ or 1st toe).
arthrodesis, and the conclusion of the study was that implantation
Please cite this article in press as: Richter M, et al. Matrix-associated stem cell transplantation (MAST) in chondral defects of the 1st
metatarsophalangeal joint is safe and effective—2-year-follow-up in 20patients. Foot Ankle Surg (2016),

FAS-937; No. of Pages 6
M. Richter et al. / Foot and Ankle Surgery xxx (2016) xxx–xxx
of ‘‘synthetic cartilage'' and arthrodesis were equivalent. When
modifying the MRI at our institution, we immediately noticed the
comparing length and rate of follow-up, our results have the same
difference. The cartilage was clearly pictured. Furthermore, fluid
typical 2-year-follow-up with a 100% follow-up rate The score
content could be measured and displayed. Even lacking a scientific
based results seem to be comparable based on the fact that
investigation, the qualitative interpretation of changed MRI
different scores were used . Regarding functional assessment,
methods with smaller slice thickness implies that the modified
we would again like to point out that this is the first investigation
technique is much better. We conclude that only MRI with slice
including validated pedographic parameters. We registered
thickness of 1 mm or less is able to correctly picture ankle cartilage.
improvement of function, i.e. pressure/force distribution in the
Based on our conclusion, we did not include MRI findings in
gait stance phase which was not shown by the above mentioned
because MRI with sufficient technical specifications (thin slice
study. Our results seem to be better than with cheilectomy alone
thickness) was not available at our institution for the entire follow-
which was the main goal of the introduced method Es-
up period. Therefore, we used our validated score as principal
pecially, improvement of validated score, validated functional
outcome parameter and not MRI findings
assessment and low conversion rate to arthrodesis (0%) is superior
In conclusion, surgical treatment including MAST led to
to previously reported results of cheilectomy alone
improved clinical scores, ROM, pedographic parameters and
decreased radiographic hallux rigidus stage. Even though a control
group is missing, we conclude that MAST is a safe and effective
method for the treatment of chondral defects of the 1st MTPJ.
Limitations of the study are: small patient number, unclear
indication for treatment, associated procedures, no control group,
short follow-up, and missing outcome parameter for the created
Conflict of interest
tissue. All patients with corrective osteotomies at the forefoot and
combination with MAST at the 1st MTPJ were excluded from the
None of the authors or the authors´ institution received funding
study because we wanted to exclude any effect of a correction on
in relation to this study.
the result. More patients (n = 57) were excluded from the study
due to corrective osteotomies than patients (n = 20) included
without corrective osteotomies. Furthermore patients with
bilateral treatment (n = 15) were excluded comprising almost as
many patients as included with unilateral treatment (n = 20).
A missing control group is always a methodological shortcom-
ing as in many other studies that we cannot invalidate. The follow-
up time of 2 years for a modified or new technique seems
appropriate. Nevertheless a longer follow-up would be desirable.
When indicating MAST, we did not follow a clear and objective
definition regarding the combination of defect size, location and
age. The indication was finally made intraoperatively and
subjectively by the surgeon. Regarding assessment of the created
tissue, we did not obtain histological specimens which would be
optimal from a scientific point of view. Giannini et al. suggested to
use special MRI protocols (T2) for the ankle for evaluation of the
tissue at follow-up and created a score from that They
suggested that an integration of both T2 mapping and Magnetic
Resonance Observation of Cartilage Repair scoring permitted
adequate evaluation of the repair site in the ankle Based on
our experience regarding MRI based assessment of chondral
lesions at the ankle, we would like to discuss the diagnostic value
of MRI for chondral defects even if we did not investigate the
imaging as such. In our earlier study, we noticed a high
incoherence between MRI findings and intraoperative (arthro-
scopic) findings when focusing on the cartilage and not on the
subchondral bone situation at the ankle . This was also
described earlier and for other joints So it seems clear
that MRI is able to detect subchondral bone abnormalities but it is
much less clear why the investigation of the cartilage is not
optimal After having changed from ‘‘standard'' MRI
imaging with slice thickness of 3 mm to so-called ‘‘Cartilage-
mapping'' with slice thickness of 0.4 mm, we immediately realised
the reason is simply technical. The normal cartilage thickness at
the ankle is around 1 mm, and the same is true for the 1st MTPJ.
Using an investigating method with a larger slice thickness
(‘‘standard'' MRI with 3 mm slice thickness) is technically not able
to correctly picture cartilage. The created pictures show a full
image but the displayed structures between the slices are
calculated means from the neighbouring slices. This might be
sufficient for subchondral bone structure with a diameter of 3 mm
or more but not for cartilage with thickness of less than 2 mm.
When we obtained ‘‘slices'' of 0.4 mm from the ankle after
Please cite this article in press as: Richter M, et al. Matrix-associated stem cell transplantation (MAST) in chondral defects of the 1st
metatarsophalangeal joint is safe and effective—2-year-follow-up in 20patients. Foot Ankle Surg (2016),
FAS-937; No. of Pages 6
M. Richter et al. / Foot and Ankle Surgery xxx (2016) xxx–xxx
Please cite this article in press as: Richter M, et al. Matrix-associated stem cell transplantation (MAST) in chondral defects of the 1st
metatarsophalangeal joint is safe and effective—2-year-follow-up in 20patients. Foot Ankle Surg (2016),
Source: http://jointoperations.co.uk/wp-content/uploads/2016/07/Richter-2016-AMIC-MTP-2-years.pdf
HOLY TRINITY PARISH NEWSLETTER Edition No. 11 October 2011 FROM THE PASTOR'S DESK You might like to say the following prayer as you light yourcandle for your intention; Lord, May this candle be a light for You to enlighten me in mydifficulties and decisions. May it be a fire for You to burn out ofme all pride, selfishness and impurity. May it be a flame for Youto bring warmth into my heart, towards my family, myneighbours, and all those who meet me. Through the prayers ofMary, virgin and mother, I place into Your care those I came toremember especially .(name).
PREEMPTING A PROBLEM: MENSING, TEVA, AND THE PROPER SCOPE OF CONFLICT PREEMPTION State-law product liability claims provide a powerful incentive for companies to create safe products. Federal law, however, provides a defense for manufacturers: preemption of state- law claims when federal and state law conflict such that dual compliance is impossible. The