Phm.net.my
Overuse of antibiotic negatively affects to
our intestines & health
ou have been prescribed antibiotics when you caught a cold. At the same time, many of you have
heard about antibiotics giving adverse effects to the stomach and intestines because they kill good
Y bacteria. This issue will include explanations about the relationship between antibiotics and our
◆◇ Microorganisms generate antibiotics in order to kill other bacteria
Antibiotic is an antimicrobial substance that microorganisms generate. Dr. Satoshi Ōmura, a Japanese
biochemist who was awarded the Nobel Prize in 2015, have extracted the anti-parasitical compound avermectin
from the microorganism called actinomycetes. When microorganisms fight over territory, they produce a
substance to kill other microorganisms so they do not come closer to them. This substance is
antibiotic/antiseptic. Antibiotics are also a medicine to kill bacteria. Therefore, it is ineffective as a treatment for
a cold because a cold is caused by viruses.
Tamiflu and Relenza are the trade names of the medicines that are prescribed to patients with influenza. They are
antiviral drugs (Antiviral drugs do not directly kill viruses. They only prevent the multiplication of viruses.). If a
patient is prescribed antibiotics when he/she caught a cold, the purpose is to protect the patient with
compromised immune systems becoming infected with other bacteria. However, recent healthcare providers tend
to reduce use of antibiotics.
◆◇ Be aware of widespread drug-resistant strains which brought by overuse of antibiotics
Antibiotics have greatly contributed to the eradication of infectious diseases throughout human history. Before
1950, over 100,000 patients lost their lives annually due to an infection with bacteria responsible for
tuberculosis. However, almost no patients die by tuberculosis nowadays because of antibiotics. There had been
mortal cases in the past when bacteria entered the body from wounds that occurred during childbirth or injuries.
After the development of antibiotics, these cases rarely occurred. As these examples, antibiotics have been an
absolutely necessary medicine for us to fight against harmful bacteria. On the other hand, the penetration of
antibiotics has created bacteria that are resistant to medicines. These bacteria are called antibiotic-resistant
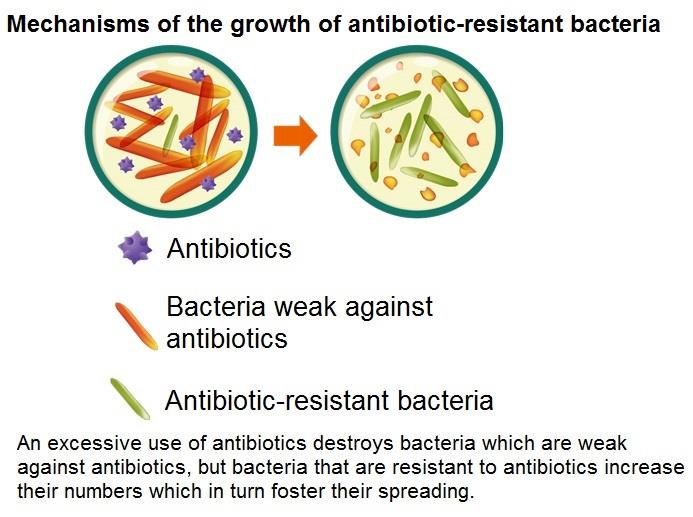
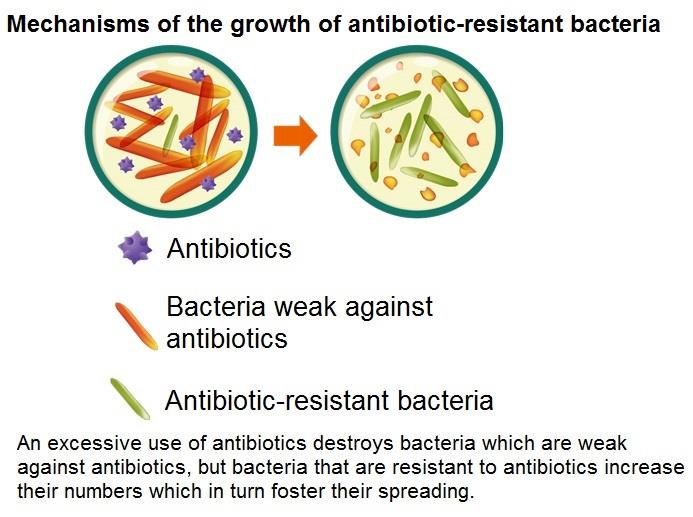
Antibiotic-resistant bacteria do not die even if
they get antibacterial agents. They originally
occur in nature. Unfortunately, only the
bacteria resistant to antibacterial agents
survive and grow their numbers if humans
keep taking antibiotics for a long time.
According to a research study that was
published in 2014, the administration of
antibiotics affected gut microbiota and the
number of intestinal bacteria declined while
antibiotic-resistant bacteria that initially reside
in the intestine could survive for a year.
Moreover, farm animals keep taking a certain amount of antibiotics because a low level of antibiotic is mixed
with their feeds. Actually, the weight of animals increases by giving antibiotics. While the use of antibiotics as a
growth stimulant is prohibited in Europe, many other countries including Japan have still been using it. Other
studies have reported that an administration of antibiotic to humans made them obese. Antibiotics are also used
for plants. These wide ranges of use of antibiotics have encouraged an increase of antibiotic-resistant bacteria.
Types of antibiotics
1. Antibiotics which work by bursting bacterial cell walls.
Penicillin antibiotics, Cephem antibiotics
2. Antibiotics which work by inhibiting protein synthesis
Macrolide antibiotics, Tetracycline antibiotics, Aminoglycoside antibiotics
3. Antibiotics which work by inhibiting DNA replication
New Quinolone antibiotics
The target bacteria is different depending on the type of antibiotics. Antibiotics are prescription medicines in Japan but available without prescription in some countries in south-eastern Asia. An improper antibiotic use foments the spread of antibiotic-resistant bacteria.
In-hospital infection has become a big issue with the increase of antibiotic-resistant bacteria. Since the 1970s,
many people have been infected with methicillin-resistant Staphylococcus aureus (MRSA) which is one of the
antibiotic-resistant bacteria and MRSA has been widespread in medical facilities. The antibiotic-resistant
bacteria have spread to the public and caused dermatitis, pneumonia and meningitis. 262 million outpatients in
the US were prescribed antibiotics in 2011. According to the research data reported in 2016, about 30% of those
prescribed antibiotics might be unnecessary.
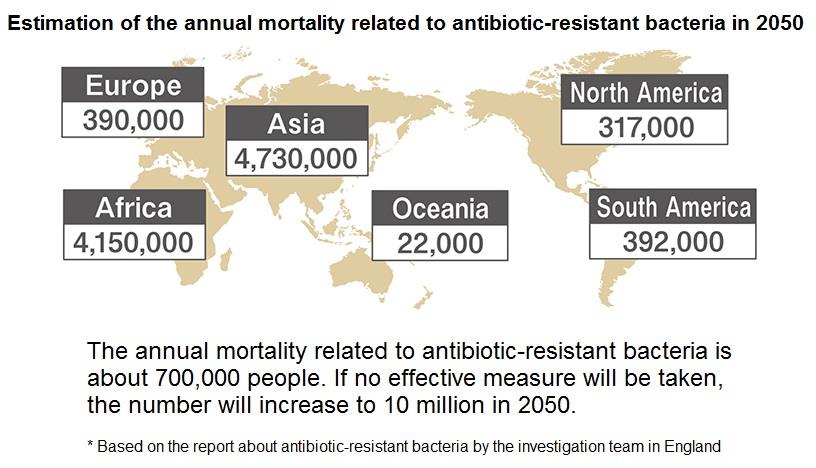
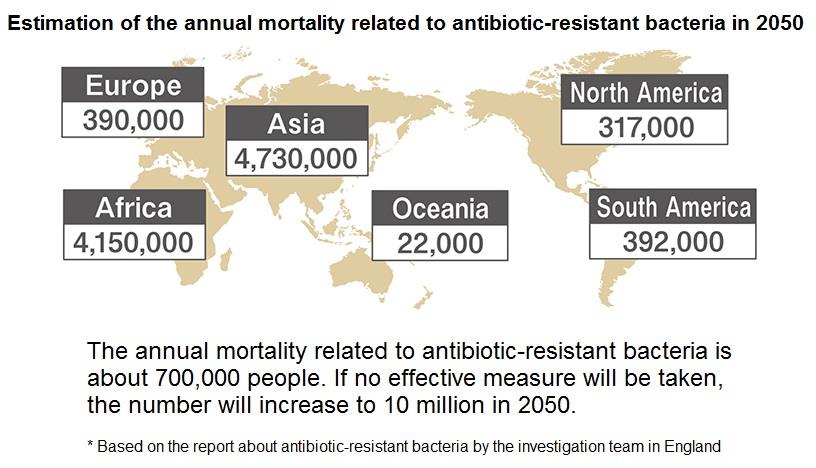
Furthermore, a report in England have made a prediction that the annual fatalities from antibiotic-resistant
bacteria will reach to about ten million people in 2050. Notably, the number of deaths will be very high in Asia
and Africa and serious financial damages are anticipated.
◆◇ Use of antibiotics shortly after birth rises the risks of developing asthma and obesity
Other research studies have reported that the change of gut microbiota by the administration of antibiotic
provides many different adverse effects to our health. For example, the research study about the relationship
between the use of antibiotic in the infant stage and the development of asthma and obesity has been
progressing. The study with a total of 236 Finnish children with age between 2 to 7 years old were conducted in
2016. It reported that the use of antibiotic during 2 years of life is associated with an increased risk of asthma,
and a high frequency of the use of antibiotics induced more risks of obesity. According to the other study with
laboratory mice which was conducted in 2014, while the number of intestinal bacteria including lactic acid
bacteria was decreasing due to the use of antibiotics, candida, which is one of the fungi, increased its numbers
which in turn made the symptoms of asthma severe.
Side-effects from the use of antibiotics
Aggravation of allergic symptoms including asthma
Increased risks of obesity
Deterioration of memory and learning ability
Increase of Candida
Antibiotics can protect us from infections if we follow the necessary intake amount and frequency. An excessive use of antibiotics may cause above side-effects.
◆◇ The deterioration of gut microbiota from the use of antibiotics provides adverse effects to the brain
Recent studies have revealed that the conditions of intestinal bacteria are associated with the functions in the
brain. The patients with depression or autism have a deteriorated intestinal balance. During an animal study,
laboratory mice that were administrated with antibiotics demonstrated an aggravated gut microbiota, and a drop
of the levels of beneficial substances which were generated by intestinal bacteria. The blood concentration of
corticosterone which is known as a stress hormone increased. Moreover, the deteriorated conditions in the
amygdala and hippocampus in the brain were observed. It drove changes in substances responsible for neural
transmission to the cerebrum resulted in causing negative impacts in their memory and ability to learn.
In light of these circumstances, the World Health Organization made calls in 2015 about the proper use of
antibiotics. What we should not forget is the fact that antibiotics are absolutely necessary to save lives. If we stop
demanding antibiotics without careful consideration, the speed of widespread of antibiotic-resistant bacteria will
slow down. It will make antibiotics more effective when it is truly needed.
Four antibiotic awareness tips addressed by WHO
Never ask for antibiotics if you don't need them
Take the full prescription even if you feel better
Do not hesitate to consult your doctor for advice on
You were prescribed a proper amount of antibiotic, so
the use of antibiotics.
you should finish it even if you feel better.
Never use leftover antibiotics
Never share antibiotics with others
Even if someone who is not a doctor offers
If you are not a doctor, you should not share your
prescribed medicines out of kindness, you should
antibiotics with others based on your judgement.
decline the offer.
We should be aware of what medicine we take in order to speed down the spread of antibiotic-resistant bacteria.
<References>
Cell Host & Microbe. 15, 95-102 (2014)
Brain Behav Immun. doi: 10.1016/j.bbi.2016.02.020 (2016)
Nature Communications. 7, 10410 (2016)
Source: http://phm.net.my/Portal/phm/Newsletter/CNL%20July,%202016.pdf
WOODY PLANT DISEASE CONTROL GUIDE FOR KENTUCKY by John Hartman, Mary Witt, Don Hershman, and Robert McNiel Cultural Practices to Prevent Disease Good care of trees and shrubs prevents many nursery and landscape problems. Because trees and shrubs live for manyyears, their susceptibility to disease is influenced not only bycurrent climatic and environmental conditions but also byconditions and care during previous years. Adverse growingconditions, maltreatment, and lack of care favor manydiseases. Many problems in nurseries and landscapeplantings can be avoided by selecting proper plant materials,creating good planting sites, avoiding unnecessary wound-ing, providing routine care (including fertilization and timelywatering and pruning), and using preventive disease andinsect control measures as needed.
ESTUDIO DE IMPACTO AMBIENTAL PRELIMINAR- RELATORIO PROSALUD FARMA S.A. Importación, Exportación, Distribución y Representación de Especialidades Farmacéuticas Terminadas; Importación, Distribución y Representación de Productos Domisanitarios riesgo I y II; de Dispositivos Médicos (descartables); de Jeringas y Agujas; Importación de Especialidades Farmacéuticas Semiterminados y Fraccionadora y Envasadora de Especialidades Farmacéuticas,