Dochdl1onprintreadytmptarget
34265_text section:34265 text section 14/1/11 10:34 Page 1
Caring for People with Dementia
in Acute Care Settings
A Resource Pack for Staff
SECTION 1
Caring for people with Dementia in Acute Hospitals – A 10 Point Guide
SECTION 2
Alzheimers Society ‘This is me' - Patient Profile
SECTION 3
Cognitive Assessment
SECTION 4
Policies and Procedures
SECTION 5
Guidance for Assessment and Care management of Patients who are
at risk of wandering in the acute care setting
SECTION 6
Further information & advice including NICE Guidelines
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 2
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 3
This guide is intended to be used as a referenceto support you to care for people with dementia.
Please add your own local policies/information as needed.
Name of Trust:
Name of Clinical Leads and contact details:
Name of Specialist Dementia Nurse and contact details:
Training and Education department for dementia and contact details:
Signed by:
Chief Executive
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 4
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 5
About 700,000 people in the UK currently have dementia, and this is likely to increase to1.7 million by 2051 (DH, 2009). The term ‘dementia' is used to describe a syndrome whichmay be caused by a number of illnesses in which there is progressive decline in multipleareas of function, including decline in memory, reasoning and communication skills andthe ability to carry out daily activities.
Two thirds of NHS beds are occupied by older people and it is estimated that up to 60 percent have or will develop a mental disorder during their admission and up to 40 per centwill have dementia (Royal College of Psychiatrists, 2005).
Being a patient in hospital can be a very difficult experience for a person with dementia,hospital environments can be disorientating and make the person with dementia appear more confused than normal, but there are things we can do to make the person'sexperience in hospital less stressful.
The aim of this resource folder is to provide practical information for staff caring forpeople with dementia to help understand some of the particular needs of people withdementia and their carers.
Further reading and signposting to further information is included at the back of theresource folder.
Royal College of Psychiatrists (2005) Who Cares Wins Council Report RCP
Department of Health (2009)
Living well with dementia:
A National Dementia Strategy, London, Department of Health
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 6
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 7
SECTION 1
10 Point Guide: Caring for People with Dementia in Acute
Hospitals
Being admitted into hospital and the time spent there as a patient can be a verychallenging experience for a person with dementia. There are times when caring forpeople with dementia on acute hospital wards can be challenging for staff also.
60-70% of beds in acute hospitals are typically occupied by people aged 65 and over, andof these approximately 30% suffer from dementia. With the numbers of people withdementia in hospitals as high as they are it is important staff have some understanding of the particular needs of people with dementia and their carers.
This brief guide aims to help with this understanding by focusing on a few key aspects of care. Further reading is given at the end of the booklet.
1. What is dementia?
Dementia is caused by a disease of the brain, usually chronic (at least six monthsduration) and progressive.
There is a decline in memory and other higher cortical functions such as judgement,thinking, orientation, comprehension and language, and learning capacity
Consciousness is not clouded
A deterioration in emotional control, social behaviour and motivation is alsocommon.
‘There are over 100 causes of dementia, however approximately 95% of cases arecaused by the commonest conditions, these include Alzheimer's disease, Vasculardementia and Dementia with Lewy Bodies.
This is the most common condition causing dementia accounting for around 55% of allcases of dementia. It is a progressive disease in which the neurones (brain cells) andcommunication pathways of the brain are destroyed. Plaques and tangles develop in thestructure of the brain, and the chemical messengers in the brain are affected. Possiblefeatures include:
Memory loss – initially affecting short term memory whilst long term memoryremains intact although this too is affected over time
Loss of sense of time and place
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 8
Loss of everyday skills
Impaired reasoning
Recognition problems – objects and people
disinhibitory behaviour
Movement problems
Incontinence (later stages)
Hallucinations (Be aware that certain misunderstandings can be misleadinglylabelled as "hallucinations" e.g. a person mistaking their reflection in the mirror to be an intruder in their room)
Vascular Dementia (sometimes referred to as "multi-infarct dementia") is the second mostcommon cause, and occurs as a distinct condition in about 20% of people with dementia.
It can be caused by a stroke, or series of strokes where blood supply to areas of the brain isblocked by a blood clot. Deprived of blood supply, brain cells in affected areas can diecausing impairments related to the function of that particular area of the brain.
Symptoms can be similar to Alzheimer's Disease but the following differences are oftenapparent:
Onset is often abrupt
There may be periods where symptoms do not progress followed by an episode ofacute confusion often associated with a new "mini-stroke" – a step-like progression
People can sometimes have a greater degree of self-awareness
There is an increased likelihood of problems with unpredictable behaviour orchangeable moods
Some abilities may remain largely unaffected depending on which areas of the brainare undamaged
As with all types of dementia vascular dementia can co-exist with Alzheimer's and otherforms of dementia.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 9
Dementia with Lewy Bodies / Lewy Body Dementia
DLB accounts for approximately 15% of cases of dementia (some studies put this figurehigher). Lewy bodies are tiny spherical protein deposits found in nerve cells and theirpresence in the brain disrupts its' normal functioning. Lewy bodies are also found in thebrains of people with Parkinson's Disease. Again, the symptoms can be similar toAlzheimer's Disease but the following differences are often apparent:
Symptoms are more likely to fluctuate, episodes of more severe confusion can befollowed by lucid intervals over minutes, hours or days
People are more likely to experience visual or auditory hallucinations
Parkinsonian symptoms – e.g. tremor, muscle stiffness, slowness, changes to voicetone and strength may be present
People are more prone to falls
People may have restless and disturbed nights with nightmares and hallucinations
People with Lewy Body Dementia have a potentially life-threatening sensitivity to
neuroleptic medication which can cause parkinsonism.
The Alzheimer's Society provides the following advice1:
If a person with DLB must be prescribed a neuroleptic it should be done with the utmostcare, under constant supervision, and it should be monitored regularly. The following listincludes the names of many of the major neuroleptics available. New drugs are appearingfrom time to time. The generic name is given first, followed by some of the commonproprietary (drug company) names for that particular compound.
Chlorpromazine (Largactil)Clopenthixol (Clopixol)Haloperidol (Haldol, Serenace)Olanzapine (Zyprexa)PromazineQuetiapine (Seroquel)Risperidone (Risperdal)Sulpiride (Dolmatil, Sulparex, Sulpitil)Trifluoperazine (Stelazine)
1 Alzheimer's Disease Information Sheet 403 August 2003
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 10
2. Be aware of the differences between dementia and other
causes of confusion
Delirium (or acute confusion) is characterised by altered consciousness and cognitive
decline, and often has a rapid onset. WARNING: It is often rather "quiet" and easy to miss
in elderly patients.
Delirium may be brought on by any physical illness (e.g. infections, diabetes, side effect of drugs) and may be the presenting sign in an elderly patient with dementia.
A person may also be confused and disorientated due other reasons such as a reaction tomedications, sensory impairment, depression, pain, bereavement, sudden change tosurroundings/routine.
Delirium is a particularly high risk in patients with the following:
2
Old age, severe illness, dementia, physical frailty, admission with infection ordehydration, visual impairment, polypharmacy, surgery, alcohol excess and renalimpairment
Be aware that changes in behaviour from the norm for the person (e.g. increasedagitation, or increased withdrawal) may indicate an underlying health problem thatmay need urgent attention.
Any acute illness can precipitate delirium.
Dementia can become a "label".
Do not assume that a person's behaviour and
confusion is necessarily a direct consequence of their dementia. Always consider
other causes of confusion.
2 British Geriatrics Society (2005) Guidelines for the prevention, diagnosis and management of delirium in older people in hospital
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 11
3. Focus on communication
People with dementia often experience increasing difficulty with verbal language. Thiscan be a problem of both expressing and interpreting language.
As a consequence, we have to pay greater attention to trying to interpret a person's needsand feelings and when we wish to express something to a person with dementia we needto adapt our usual style of communication to compensate for their difficulties.
Consider the following:
Slow down (do not out-pace) and reduce the length of your sentences.
Concentrate on your non-verbal communication (your words might not make senseto the person but your tone of voice and body language will)
Make use of objects/cues/pictures to back up what you are saying
Concentrate on the feeling/need behind what a person is saying (if a person isasking for their mother, think why this might be and try to clarify: Are they feelinganxious, lost, trapped, are they in pain, do they need the loo?)
Try to provide opportunities for reassuring human contact. Stop and share a fewmoments when you can. Encourage flexible visiting where possible (see below)
Talk through procedures as you do them to try to allay fear. Repeat informationsuch as who you are, what you are doing and why.
4. Aim for the familiar
Put yourself in the shoes of a person with dementia, if you were in a strange anddisturbing place and your short-term memory was so poor you couldn't retain informationwhat or who might help you feel more safe and secure?
Being in hospital can be disorientating and frightening for a person with dementia.
Familiar people and familiar things can provide support, comfort and reassurance.
Encourage rather than discourage the presence of close family/friends.
Encourage the person to have possessions from home (preferably not things of value in-case they go astray!) e.g. photo, bed throw, clock, cuddly toy etc
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 12
5. See behaviour as communicating a need
A person's behaviour may at times be challenging for staff and other patients. A personwith dementia may for example be creating a difficulty on the ward by for example:Repetitive shouting, wandering off the ward, interfering with other people's possessionsor equipment…
What we need to recognise first and foremost is that all behaviour has meaning and weshould "read" the behaviour as communicating a need or a feeling.
Behaviour may indicate many things; here are just a few possibilities:Being in painBeing afraidFeeling LostBeing overwhelmed by too much noise or activity on the wardNot having enough activity to simulateTrying to express a need – hunger, thirst, the need for the toiletEffects of medicationTrying to find someone or something familiar
•
Remember, a sedative used to control behaviour will not meet any of these underlying
6. Make the most of the expertise of family members and
friends
Knowing as much as possible about a person with dementia can assist greatly in their care.
Your most valuable supply for this information will be the person themselves and/or theirrelative/carer.
Relatives may have precious information on what actions/responses are likely to make aperson more distressed, and what can help a person feel more secure.
Relatives might be able to provide insight and explanations of behaviours you findpuzzling (for example it would be imperative to know that if a person with dementia was refusingfluids on the ward, whether they had any particular needs around drinking at home. Itmight be for example, that when at home they only ever drank from a particular mug orcup. Bringing this in might just be an answer).
Make sure such vital information is shared across the care team.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 13
7. Ensure the person eats and drinks well
A person with dementia may look like they should be able to eat and drink withoutassistance, but may in fact need help.
In addition to problems anyone might have when it comes to eating well in hospital suchas physical discomfort, loss of appetite, sensory impairment etc. A person with dementiamay have specific problems such as:
Difficulty initiating an action (picking up a fork or spoon to eat)Difficulty recognising food, drinks, implements for what they are (agnosia)Difficulty with visual-spatial awareness, making seeing the food more difficultDifficulties with memory – remembering to eat and drinkExperiencing anxiety and other emotions that may effect appetite
Appropriate prompting
The presentation of the food
Stress-free environments in which to eat main meals (too much noise and distraction are not conducive to this)
Being able to eat little and often rather than just at the set mealtimes
8. Try to make the environment as stress-free as possible
People with dementia are likely to benefit from continuity and familiarity.
Try to avoid repeated moves within the hospital wherever possible.
Try to make a person's surroundings as calm and familiar as possible.
Make use of signage for toilets and other rooms to improve the chances of a personfinding their way around. Good signage will use a picture (e.g. of a toilet) rather than aword.
9. Encourage the person to be meaningfully occupied
Like everyone else, people with dementia have a need to be occupied, purposeful andactive. All too often in hospitals there is very little to occupy people. For a person withdementia this lack of occupation may lead to them behaving in ways that cause difficultiesfor themselves and others, or conversely, it may lead to a person withdrawing more andmore into themselves and losing all motivation.
Ideas for encouraging meaningful activity:
Encourage families to visit and to bring in anything that may help keep a personoccupied.
Find out from families what interests the person has
Books, photos, bags with items to rummage through may all help.
Provide opportunities for exercise
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 14
10. Providing adequate pain relief
There is evidence to suggest that people with dementia are likely to experience less painrelief in hospital than people who do not have dementia and this becomes a greaterproblem the more severe the cognitive impairment3. Hence, the more confused anddisorientated, a person is the less likely they are to receive effective pain control.
Behaviour such as shouting, aggression, agitation and wandering may be triggered bypain. All too often anti-psychotic medication is prescribed for people with these behavioursrather than pain relief.
Nurses play a vital role in assessing pain and administering pain relief in people withdementia and should consider the following:
Asking patients with dementia regularly if they are in pain
Use of pain assessment scales particularly where verbal communication skills are reduced
Observe for behavioural, physiological and body language changes in individuals to guideassessment of pain
Consider requesting "by the clock" medication for some people rather than "as required"4
3 Scherder E, Osterman J and Swaab B et al (2005) Recent developments in pain in dementia British MedicalJournal. 330, 7489 364-369
4 Cunningham C (2006) Managing pain in patients with dementia in hospital Nursing Standard. 20, 46, 54-58
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 15
Support for family carers
Relatives may be an invaluable support to the person with dementia and to the wardteam. However, caring is very stressful and being in hospital may in itself be theopportunity for a much needed break from caring.
The following organisations may be able to provide support and advice to carers (and topeople with dementia directly)
Alzheimer's Society (National)
National helpline and helpful web resource for information and support for people with
dementia, relatives and professionals:
Telephone: 020 7306 0606 Email:
[email protected]Helpline:
0845 300 0336 (8.30am to 6.30pm Monday to Friday)
www.alzheimers.org.uk
Picks Disease Support Group (PDSG)
For carers of frontotemporal dementia: Pick's Disease, Frontal Lobe Degeneration,
Dementia with Lewy Bodies, Corticobasal Degeneration and Alcohol Related Dementia.
Contact: Carol Jennings, AdviserTel : 0845 458 3208
[email protected]
Archibald, C (2003) People with dementia in acute hospital settings: A practice guide forregistered nurses. The Dementia Services Development Centre. Stirling.
Archibald, C (1999) Food and Nutrition in the Care of People with Dementia. TheDementia Services Development Centre. Stirling.
Cantley, C (2001) A Handbook of Dementia Care. Open University Press
Cheston, R and Bender, M (2003) Understanding Dementia: The Man with the WorriedEyes. Jessica Kingsley.
Kitwood, T (1997) Dementia Reconsidered. Open University Press
Stokes, G (2005) Challenging Behaviour in Dementia: A person centred approach.
Speechmark
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 16
Nursing Standard series on dementia care in acute hospitals:
Archibald, C (2006) Promoting hydration in patients with dementia in healthcare settings. 20, 44, 49-52
Archibald, C (2006) Meeting the nutritional needs of people with dementia in hospitals. Nursing Standard. 20, 45, 41-45
Cunningham, C and Archibald, C (2006) Supporting people with dementia in acute hospitalsettings. Nursing Standard. 20, 43, 51-55
Cunningham, C (2006) Managing pain in patients with dementia in hospital. 20, 46, 54-58
Cunningham, C (2006) Understanding challenging behaviour in patients with dementia .
Nursing Standard. 20, 47, 42-45
The Journal of Dementia Care: Hawker Publications
www.alzheimers.org.uk
The UK's leading care and research charity for people with dementia, their families and
carers
www.brad.ac.uk/health/dementia
Bradford Dementia Group. Provide teaching, education and research in dementia care
and home to Dementia Care Mapping
www.dementia.stir.ac.uk
The DSDC works to spread research and good practice about home and hospital care for
people with any type of dementia including Alzheimers disease, multi-infarct dementia,
Lewy body dementia, vascular dementia and alcohol-related dementia throughout the
world.
Booklet written by:
Trent Dementia Services Development Centre
Part of a network of centres offering advice, training, and service development for all
service providers. Registered Charity no 1109855
Telephone: 0116 257 5017www.trentdsdc.org.uk
[email protected]
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 17
This is me
This leaflet will help you support me
in an unfamiliar place
Please place a photograph of yourself in the space provided.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 18
This is me is about the person at the time the document is completed and will
need to be updated as necessary.
This is me should be completed by the person or persons who know the patient
best and wherever possible with the person themselves.
Please refer to the back page for guidance notes to help you complete
This is me.
My name: full name and the name I prefer to be known by
Carer/the person who knows me best
I would like you to know
My home and family, things that are important to me
My hobbies and interests
Things which may worry or upset me
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 19
I like to relax by
My hearing and eyesight
My eating and drinking
Relationship to patient:
In signing this document, I agree that the information in this leaflet may be shared with health
and care workers.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 20
Guidance notes to help you to complete
This is me
This is me is intended to provide professionals with
My communication: How do I usually communicate,
information about the person with dementia as an
eg verbally, using gestures, pointing or a mixture of
individual. This will enhance the care and support given
both? Can I read and write and does writing things
while the person is in an unfamiliar environment.
down help? How do I indicate pain, discomfort, thirst
It is not a medical document.
or hunger? Include anything that may help staffidentify my needs.
This is me is about the person at the time the
document is completed and will need to be updated
My mobility: Am I fully mobile or do I need help?
as necessary. This form can be completed by the
Do I need a walking aid? Is my mobility affected by
person with dementia or their carer with help from
surfaces? Can I use stairs? Can I stand unaided from
the person with dementia where possible.
sitting position? Do I need handrails? Do I need a special chair or cushion, or do my feet need raising to make me comfortable?
My name: Full name and the name I prefer to be
known by.
My sleep: Usual sleep patterns and bedtime
routines. Do I like a light left on and do I find it
Where I currently live: The area (not the address)
difficult to find the toilet at night? Position in bed,
where I live. Include details about how long I have
any special mattress, pillow, do I need a regular
lived there, and where I lived before.
change of position?
Carer/the person who knows me best: It may be
My personal care: Normal routines, preferences
a spouse, relative, friend or carer.
and usual level of assistance required in the bath
I would like you to know: Include anything I feel
or, shower or other. Do I prefer a male or female
is important and will help staff to get to know and
carer? What are my preferences for continence
care for me, eg I have dementia, I have never been
aids used, soaps, cosmetics, shaving, teeth cleaning
in hospital before, I prefer female carers, I don't like
the dark, I am left handed, I am allergic to… etc.
My eating and drinking: Do I need assistance to
My home and family, things that are important
eat or drink? Can I use cutlery or do I prefer finger
to me: Include marital status, children, grandchildren,
foods? Do I need adapted aids such as cutlery
friends, pets, any possessions, things of comfort.
or crockery to eat and drink? Does food need to be
Any religious or cultural considerations.
cut into pieces? Do I wear dentures to eat or do I have swallowing difficulties? What texture of food
My life so far: Place of birth, education, work
is required to help, soft or liquidised? Do I require
history, travel, etc.
thickened fluids? List likes, dislikes and any special
My hobbies and interests: Past or present –
dietary requirements including vegetarianism,
eg reading, music, television or radio, crafts, cars.
religious or cultural needs. Include information about my appetite and whether I need help to
Things which may worry or upset me: Anything
choose food off a menu.
that may upset me or cause anxiety such as personalworries, eg money, family concerns, or being apart
My medication: Do I need help to take medication?
from a loved one, or physical needs, eg being in pain,
Do I prefer to take liquid medication?
constipated, thirsty or hungry.
I like to relax by: Things which may help if I become
unhappy or distressed. What usually reassures me,
Dedicated to the memory of Ken Ridley, a much
eg comforting words, music or TV? Do I like company
valued member of the Northumberland Acute Care
and someone sitting and talking with me or prefer
and Dementia Group.
quiet time alone? Who could be contacted to help
The Royal College of Nursing is pleased to support
This is me.
My hearing and eyesight: Can I hear well or do I
need a hearing aid? How is it best to approach me?
To order extra copies call Xcalibre on 01753 535751.
Is the use of touch appropriate? Do I need eye contact
For general dementia queries call our Helpline on
to establish communication? Do I wear glasses or
0845 300 0336.
need any other vision aids?
With Thanks to University Hospitals of Leicester for producing this Resource Pack
Alzheimer's Society operates in England, Wales and Northern Ireland. Registered charity no 296645.
34265_text section:34265 text section 14/1/11 10:34 Page 21
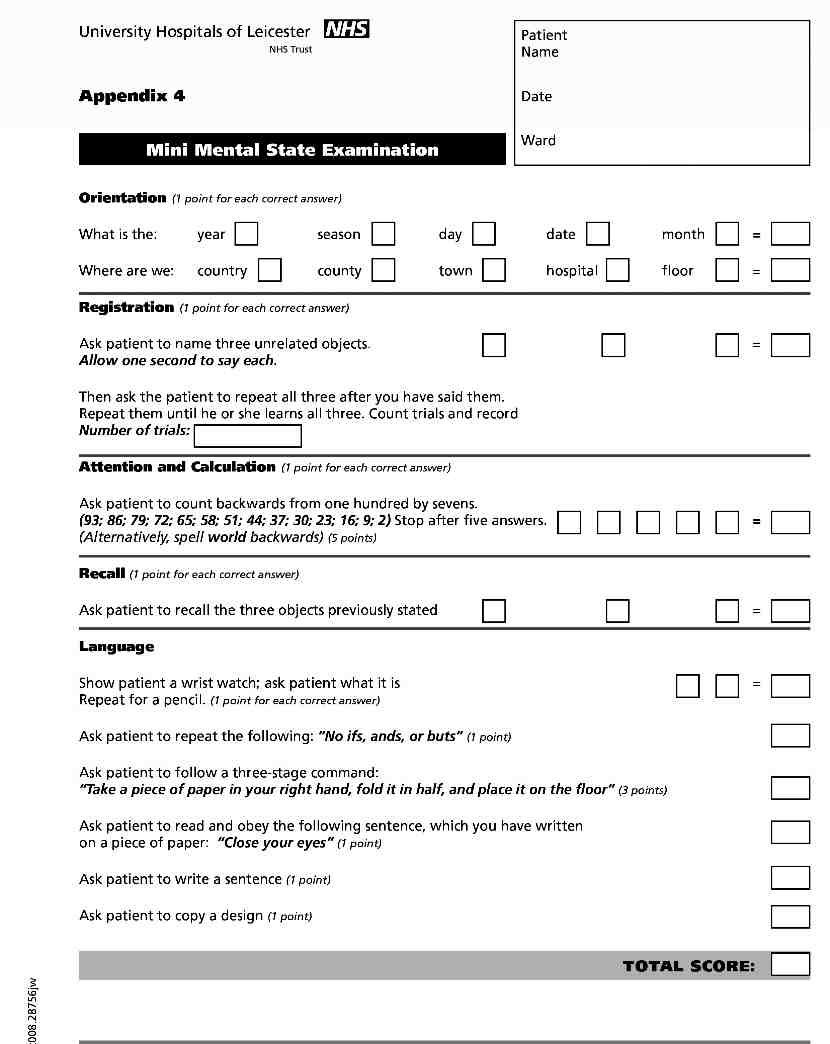
SECTION 3
A cognitive assessment is an examination conducted to determine someone's level ofcognitive function. Cognitive function refers to a person's ability to process thoughts.
Cognition primarily refers to things like memory, the ability to learn new information,speech, and reading comprehension.
There are a number of reasons to perform a cognitive assessment and these assessmentscan be administered by a doctor, nurse or allied health professional. Several standardisedcognitive assessments have been published which are outlined in the Cognitive AssessmentTools guideline within this section including a cognitive screening algorithm.
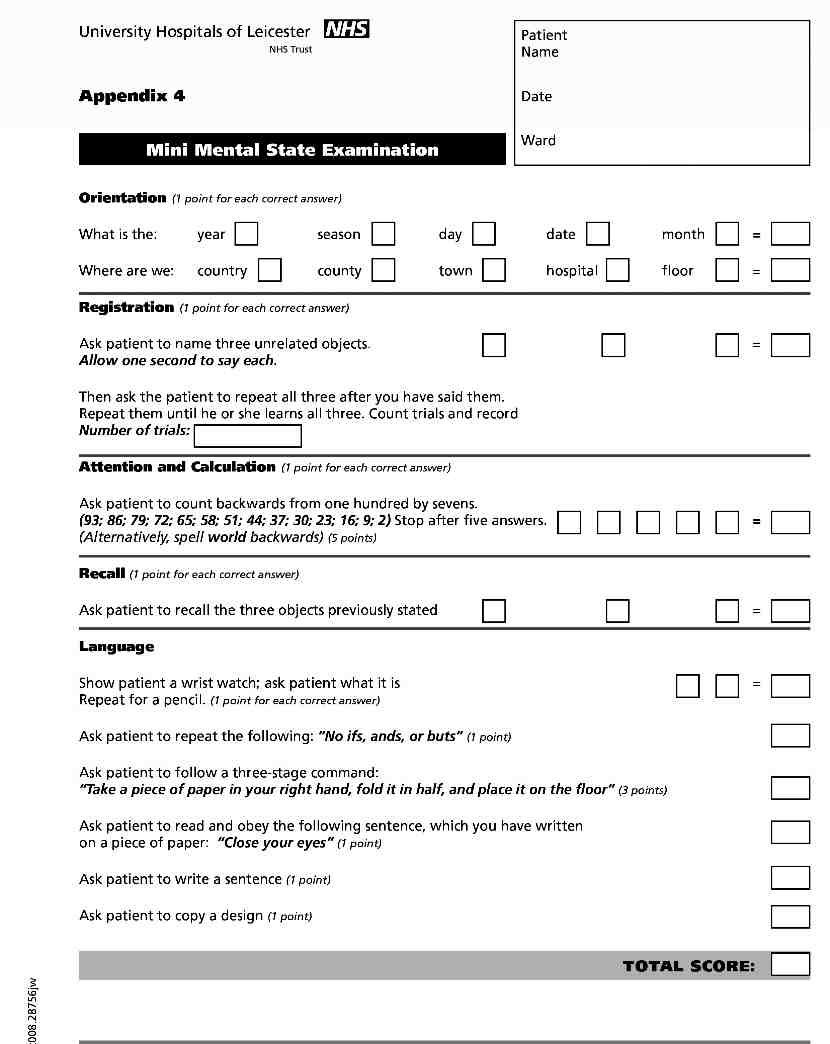
The algorithm recommends the use of four cognitive tests:
1. MMSE – Mini Mental State Examination
2. CLOX1 – An executive clock drawing task
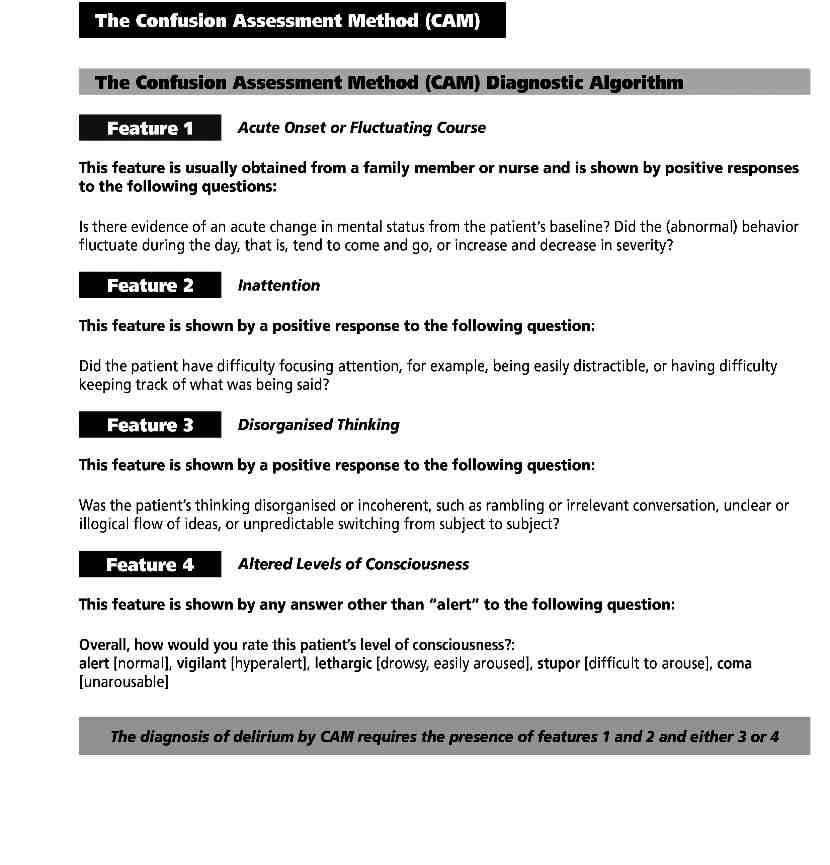
3. CAM (short version) – Confusion Assessment Method
4. IQCODE (short version) – Informant questionnaire on cognitive decline in the elderly
It is important to note that if a person with dementia is physically unwell, any results ofthe cognitive assessment can be considerably affected. Cognitive impairment that presentsas dementia may also be associated with delirium or depression. It is therefore essential tospeak to family and carers to establish a good baseline history.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 22
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 23
A guideline for cognitive assessment
Medicine and A&E Directorate
of the Older person admitted to
hospital
1. Introduction
Dementia is common in older people. It affects 5% of people over age of 65 and 25% of people over age of 80. Yet diagnosis of dementia is frequently missed by health care professionals. It is well recognised that people living with dementia have reduced survival, increased risk of wandering and falls, increased risk of developing dehydration and malnourishment, poor outcome following surgery for hip fracture and significantly increased risk of developing delirium (acute confusional state). Evidence suggests that failure to recognise dementia results in the following:
• unnecessary hospital admission
• increased incidence of delirium
institutionalisation
• increased morbidity and mortality
The aim of this guideline is
• To offer cognitive assessment tools to health care professionals working with older
• To provide overview and limitations of each cognitive assessment tool • To raise the profile of the condition and allow clinicians to confidently diagnose and
manage the condition.
• To encourage cognitive testing on adults over the age of 65 • To develop appropriate care planning and referral of people with established condition
2. Legal Liability Guideline Statement
Guidelines issued and approved by the Trust are considered to represent best practice. Staff may only exceptionally depart from any relevant Trust guidelines providing always that such departure is confined to the specific needs of individual circumstances. In healthcare delivery such departure shall only be undertaken where, in the judgement of the responsible healthcare professional' it is fully appropriate and justifiable - such decision to be fully recorded in the patient's notes
The guideline applies to all healthcare staff working within UHL including Bank and Agency staff and those on honorary contracts.
This document provides detailed evidence based clinical guidance for assessing cognition of patients with dementia. The guidance is primarily aimed at older people (defined as aged 65 and above) although it may be of some relevance to younger patients who have cognitive impairment.
A guideline for cognitive assessment of older person admitted to hospital Page 1 of 12
Author: Nainal Shah
Written: December 2008
Approved by: SEA committee Next Review: December 2011 Insite Document Number:
NB: Paper copies of guideline may not be most recent version. The definitive version is held on the Document Management System
34265_text section:34265 text section 14/1/11 10:34 Page 24
COGNITIVE ASSESSMENT TOOLS
University Hospitals of Leicester NHS Trust
GUIDELINE FOR COGNITIVE ASSESSMENT OF THE
OLDER PERSON ADMITTED TO HOSPITAL
Adopted from British Geriatrics Society & Faculty of Old Age Psychiatry Consensus, Royal College of Physicians and National Institute for Health and Clinical Excellence (NICE) guideline on delirium and dementia 2006
A guideline for cognitive assessment of older person admitted to hospital Page 2 of 12
Author: Nainal Shah
Written: December 2008
Approved by: SEA committee Next Review: December 2011 Insite Document Number:
NB: Paper copies of guideline may not be most recent version. The definitive version is held on the Document Management System
34265_text section:34265 text section 14/1/11 10:34 Page 25
Cognitive Assessment Tools
Why do we need cognition assessment tools?
• These tools are crucial for the diagnosis of dementia and delirium • Delirium and dementia are common
o Delirium – up to 30% of older medical admissions o Dementia – affects 5% of people over age of 65 and 25% of people over age of
80 over 2/3 of patients in hospital are over 65 years and up to 60% have
impaired cognition
• Yet delirium and dementia are frequently missed by health care professionals
Importance of recognising delirium and dementia
• People with delirium have
o High mortality – twice compared to matched control o Increased length of stay o Increased rate of institutional placement o Three times risk of developing dementia
• People living with dementia have
o Reduced survival o Increased risk of wandering and falls (those who are independently mobile) o Three times the likelihood of developing dehydration and malnourishment o Poor outcome following surgery for hip fracture o Significantly increased risk of developing delirium
• Failure to recognise dementia and plan for the needs of both the dementia sufferer and
their carer(s) can result in the following:
o unnecessary hospital admission o increased incidence of delirium o delayed discharge o unnecessary re-admissions o unnecessary institutionalization
o increased morbidity and mortality.
A guideline for cognitive assessment of older person admitted to hospital Page 3 of 12
Author: Nainal Shah
Written: December 2008
Approved by: SEA committee Next Review: December 2011 Insite Document Number:
NB: Paper copies of guideline may not be most recent version. The definitive version is held on the Document Management System
34265_text section:34265 text section 14/1/11 10:34 Page 26
Why improve the assessment of cognition in older people?
• Dementia is prevalent in the acute hospital setting. • It is currently under detected and often remains undiagnosed.
National Service Framework (NSF) - Standard 7 aims
• to promote good mental health in older people • to treat and support older people with dementia and depression
What is dementia?
• A generic term indicating a slowly progressive loss of intellectual functions including
memory, significant deterioration in the ability to carry out day-to-day activities, and
often, change in social behaviour,
lasting more than 6 months
• Diagnosis of a subtype of dementia – Alzheimer's, vascular, dementia with Lewy
bodies, fronto-temporal and other dementia – should be made by health care
professionals with expertise in differential diagnosis using standard criteria.
A guideline for cognitive assessment of older person admitted to hospital Page 4 of 12
Author: Nainal Shah
Written: December 2008
Approved by: SEA committee Next Review: December 2011 Insite Document Number:
NB: Paper copies of guideline may not be most recent version. The definitive version is held on the Document Management System
34265_text section:34265 text section 14/1/11 10:34 Page 27
Tools to assess cognition
¾ Cognitive testing should be carried out on all people over age 65 admitted to hospital
¾ A diagnosis of dementia should be made only after a comprehensive assessment, which
• history taking • cognitive and mental state examination • physical examination and other appropriate investigations (basic dementia
screen includes – FBC, U+E, LFT, Glucose, Calcium, TFT, B12, Folate,
imaging – imaging helps to exclude other cerebral pathology and help establish
subtype, MRI brain preferred)
• a review of medication in order to identify and minimise use of drugs that affect
cognition adversely
• Tests for delirium are different and include screening for sepsis, excluding
metabolic disturbance and reviewing the drug history – more detail is given in
(see delirium guideline)
¾ The consensus statement of British Geriatrics Society (BGS) recommends a
cognitive
screening algorithm (Figure:1, Table:1) that will help to provide a
standard, reliable initial diagnosis of dementia
¾ The algorithm recommends the use of four cognitive tests:
1. MMSE – Mini Mental State Examination
2. CLOX1 – An Executive Clock Drawing Task
3. CAM (short version) – Confusion Assessment Method
4. IQCODE (short version) – Informant Questionnaire on Cognitive
decline in the Elderly.
A guideline for cognitive assessment of older person admitted to hospital Page 5 of 12
Author: Nainal Shah
Written: December 2008
Approved by: SEA committee Next Review: December 2011 Insite Document Number:
NB: Paper copies of guideline may not be most recent version. The definitive version is held on the Document Management System
34265_text section:34265 text section 14/1/11 10:34 Page 28
COGNITIVE ASSESSMENT PATHWAY
In emergency department (ED)
Four point test
Age DOB Place Year
On Admission to AMU/ Ward
Abbreviated
Mental
Test (AMT) score:
2. Time (to the nearest hour)
3. Address for recall at the end of test (42 West St)
5. Name of hospital
6. Recognition of two people (e.g. doctor, nurse)
7. Date of birth
8. Dates of WW2 (1939-1945)
9. Name of present monarch
10.Count backwards from 20-1 (also tests attention)
AMT < 8/10, ED four point test 3/4
Abnormal
Mini
Mental
State
Examination
(MMSE)
An Executive Clock Drawing Task
(CLOX1)
Follow
cognitive screening algorithm
A guideline for cognitive assessment of older person admitted to hospital Page 6 of 12
Author: Nainal Shah
Written: December 2008
Approved by: SEA committee Next Review: December 2011 Insite Document Number:
NB: Paper copies of guideline may not be most recent version. The definitive version is held on the Document Management System
34265_text section:34265 text section 14/1/11 10:34 Page 29
COGNITIVE SCREENING ALGORITHM
S REENING ALGORITHM
ED four point score 4/4, AMT < 8/10
Mini Mental State Examination
(MMSE) and CLOX1: An Executive
MMSE ≥24/30 and
Clock Drawing Task
Determine the duration of cognitive impairment
• Confusion Assessment Method (CAM) • Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE)
Delirium (acute
confusional
> 6months
Delirium and chronic impairment
Team assessment: screen for depression, further background information, appropriate
Investigation and
investigations : See NICE guideline
Possible dementia syndrome requiring further assessment and management Refer to memory clinic or other specia
Recommend GP to refer to specialist
P to refer to specialist
Put test results and di
Put test results and diag
agnoses of deliri
impairment in disc
nt in discharge summar
CMHT assessment in
sment clinic - LGH
Figure:1 C gnitiv
LGH – Leices er
Gen ral Hospital; CMHT – Comm
spital; CMHT – Co
mm nity Mental Health
e for cogn
cognitive a
v assessment o
der perso
person ad
admitted to
d to hospital
pital Page 7
Page 7 of 1
Written: December 200
y SEA committee Next
Insite Document Number:
NB: Paper copies of guideline may not be
s of guideline may not be mo
cent version. The
ent version. The definitive vers
definitive version is held on the Document Mana
io is held on the Document Management S
34265_text section:34265 text section 14/1/11 10:34 Page 30
Further cognitive assessment
Subject of
The patient plus
The patient's carer,
their carer, family
family member or
member and/or staff
Overview
A test that asks
The carer is asked
if there is any acute
draw a clock with change in mental
about the patient's
hands pointing to
state. The patient is
ability to carry out
the time of ‘1:45'. then observed and
a range of everyday
Specific elements
of the drawing are questions to gauge:
1.Inattention 2.Disorganised
3.Level of consciousness
Degree of decline in
assesses
absence of delirium
ability for a range of everyday tasks
Abnormal
Presence of 1+2, and
Test score
Limitations
Relies on people
outcomes in elderly
patient and being
patients for whom
the test may give
their daily activities
false positive results
Table:1 Summary of cognitive screening tools
A guideline for cognitive assessment of older person admitted to hospital Page 8 of 12
Author: Nainal Shah
Written: December 2008
Approved by: SEA committee Next Review: December 2011 Insite Document Number:
NB: Paper copies of guideline may not be most recent version. The definitive version is held on the Document Management System
34265_text section:34265 text section 14/1/11 10:34 Page 31
An Executive Clock Drawing Task
An Executive Clock Drawing Task
(CLOX1)
‘
raw me a
me a clock that sa
that says 1:45. Set the hands and numbers on the face
45. Set th
the hands and numbers on th
so that a child could read them
so that a child could read the .' All positive answers are scored.
m ' All positive a swers are
Organisational elements
nal elements
Point value
Point value
Does figure resemble a clock?
resemble a clock?
Outer circle present?
Diameter >2.5 cm
All numbers inside the circle?
12, 6, 3 and 9 placed fir
Spacing intact? (symmetry on either side of the 12–6 axis)
(symmetry on eithe
eithe side of the 2
If yes, skip next.
If yes, skip next.
spacing e rors are present, are there signs of
he e signs of correction
or erasure?Only Arabic numerals?
Only Arabic numerals?
Only numbers 1–12 among the Arabic numerals?
mbers 1–12 among the Arabic numerals?
Sequence 1–12 intact? No omissions or intrusions.
e 1–12 intact?
Only two hands present
All hands represented as arrows?
Hour hand between 1 and 2 o'clock?
nd between 1 and 2 o'cl c
Minute hand longer than hour?
Minute hand longer than hour?
None of the following:
None of the following:
1) hand pointing to 4 or 5 o'clock?
ting to 4 or 5 'clock?
2) ‘1:45' present?
3) intrusions from ‘hand' or ‘face' present?
3) intrusions from ‘hand' or ‘face' p s
4) any letters, words or
ters, words or ictures?
5) any intrusion from circle below?
5)) any intrusion from circle below? Total Score: / 16
Total Score: / 16
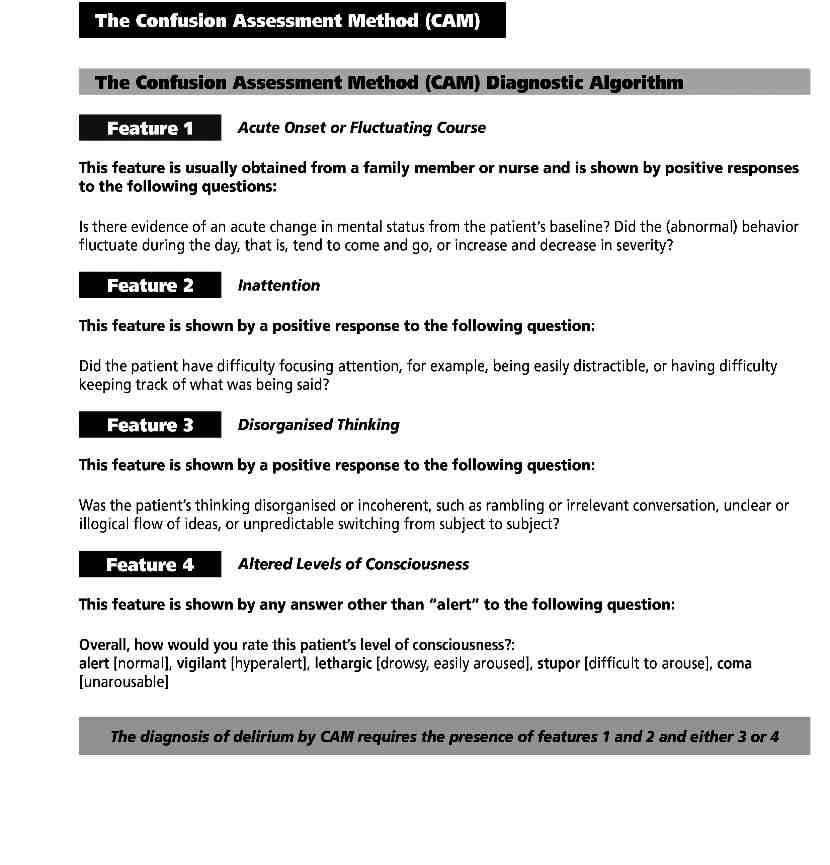
Use the
Confusion
Assessment
Method (CAM) if delirium is suspected:
To have a positive CAM result the patient must display:
1. Presence of acute onset and fluctuating course
2. Inattention (e.g. 20-1 test with reduced ability to maintain attention or shift attention)
and either
3. Disorganized thinking (disorganized or incoherent speech)
4. Altered level of consciousness (usually lethargic or stuporous)
e for cogn
cognitive a
v assessment o
der perso
person ad
admitted to
d to hospital
pital Page 9
Page 9 of 1
Written: December 200
y SEA committee Next
Insite Document Number:
NB: Paper copies of guideline may not be
s of guideline may not be mo
cent version. The
ent version. The definitive vers
definitive version is held on the Document Mana
io is held on the Document Management S
34265_text section:34265 text section 14/1/11 10:34 Page 32
n is held on the Document Mana
definitive versio
knowing how much food to bu
h have been put in a different place from
around the house
of guideline may not be s
visits from family or friend
address and telephone number
A committee Next
dling financial matte
Remembering things about family and friends, eg occupations, birt
Remembering her/hi
Remembering what day and month it is
Remembering where to find things
Knowing how to work familiar machines
Learning to use a ne
Learning new things in general
Handling other everyday arithmetic proble
Informant
Insite Document Number:
34265_text section:34265 text section 14/1/11 10:34 Page 33
The assessment
Now we want you to remember what your friend or relative was like 10 years ago and to compare it with what he/she is like now. On the previous page are situations where this person has to use his/her memory or intelligence and we want you to indicate whether this has improved, stayed the same or got worse than in that situation over the past 10 years. Note the importance of comparing his/her present performance with 10 years ago. So if 10 years ago this person always forgot where he/she had left things and he/she still does this, then this would be considered ‘Not much change'. Please indicate the changes you have observed by circling the appropriate answer.
Scoring the test
1 = Much improved2 = A bit improved 3 = Not much change 4 = A bit worse 5 = Much worse
Score for this question
IQCODE > 3.44
Abnormal
8
9
10
11
12
13
14
15
16
Total score
Sum of the results of all of the questions
The total number of questions
A guideline for cognitive assessment of older person admitted to hospital Page 11 of 12
Author: Nainal Shah
Written: December 2008
Approved by: SEA committee Next Review: December 2011 Insite Document Number:
NB: Paper copies of guideline may not be most recent version. The definitive version is held on the Document Management System
34265_text section:34265 text section 14/1/11 10:34 Page 34
It covers 5 domains:
o Orientation o Registration o Attention & calculation o Recall o Language
Total score is 30
¾ Does not assess executive function.
¾ For any section a patient is unable to complete due to a disability, it should be assumed that full points were obtained.
¾ Questionable validity in assessing cognition in ethnically diverse population
• NICE guideline: http://www.nice.org.uk/CG042• Royal College of Physicians guideline: http://www.rcplondon.ac.uk
A guideline for cognitive assessment of older person admitted to hospital Page 12 of 12
Author: Nainal Shah
Written: December 2008
Approved by: SEA committee Next Review: December 2011 Insite Document Number:
NB: Paper copies of guideline may not be most recent version. The definitive version is held on the Document Management System
34265_text section:34265 text section 14/1/11 10:34 Page 35
SECTION 4
Caring for people with dementia who wander in the acute
care setting
The key to good management of wandering behaviour is to allow the person to walkfreely. Use of technology may contribute to this, but only in conjunction with good designof the environment, meaningful activity and appropriately trained care-givers.
The Dewing Tool for Wandering Screening is a screening tool to help practitioners toidentify patients who are at risk of wandering and likely to leave a safe area.
The wandering assessment and therapeutic plan can also be used in conjunction with thePatient Profile to help identify potential triggers that can cause the patient to wander such as noise, pain, boredom, anxiety etc.
Jan Dewing 2005 Methods for preventing/responding to wandering in acute
care settings
www.wanderingnetwork.co.uk
Jan Dewing 2005 The Dewing Tool for Wandering Screening
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 36
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 37
Guidance for Assessment and Care Management of Patients
who are at risk of Wandering in the Acute Care Setting
Page number
Guideline Intention
Roles & Responsibilities
Use of assistive technology
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 38
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 39
Any person of any age who has a confusional state wether be acute or chronic maybe at risk of wandering. This could be related to a dementia type illness, but notexclusively. (UK Wandering Network, 2005) However the literature that supports thispolicy is limited to patients with dementia who wander, nonetheless the principles of assessment andcare management can be applied to any patient who may wander.
People wander for a variety of reasons, seeking a safe place, exit seeking, wanting totake some exercise and to familiarise themselves with where they are. They may alsowander when they are in a strange or unfamiliar place such as a hospital.
Wandering cannot always be prevented or even reduced. A balance needs to befound between prevention of actual risk and enabling the person to have freedom ofmovement.
There is no agreed definition of wandering; Algase et al (2001) propose thatwandering is a locomotion that is non-direct or more simply it is travelling about without anyclear destination. It can take the form of pacing, lapping or a random pattern.
3. Guideline Intention
This policy sets out the screening, assessment and care planning processes for adultpatients, who after initial assessment have been identified as at risk of wandering.
This policy will also detail good practice standards for promoting ‘safer' wandering as part of the fundamental care needs of the person.
This policy does not cover patients that have absconded, please refer to a MissingPatients Policy
4. Roles & Responsibilities
The senior team including, General Managers, Heads of Nursing, Clinical directors & Heads of Departments are responsible for ensuring that all clinical staff are madeaware of this policy, screening tool and factors to be considered as part of thepatient's treatment and care.
Individual Clinical Directorates are responsible for agreeing the criteria and riskfactors that trigger the use of the Dewing Tool for Wandering.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 40
5. Screening
The Healthcare Professional who identifies concern at initial patient assessment thatwandering may be possible must then complete the Dewing Tool for WanderingScreening ideally in partnership with the patient and their carers and takeappropriate action. (
Dewing, J. 2005 - Appendix 1)
The Dewing tool for wandering screening will help practitioners to identify patientswho are at risk of wandering and particularly those who are likely to try to leave asafe setting, in this instance the Ward or department.
It enables staff to care plan measures for responding to safer or unsafe wandering.
It also prompts practitioners to recognise the need to talk with families and haveproactive discussions about risk, supervision and helpful interventions to respond towandering activity and document helpful information.
6. Assessment
If a patient has been screened and identified as ‘at risk of wandering' then theWandering Assessment and therapeutic plan (Appendix 2) should be completed. Thistool can be used to help identify triggers to wandering and should be used to planinterventions and care accordingly.
The Wandering Assessment & therapeutic plan (Appendix 2) can also be used in conjunction with the dementia patient profile).
7. Care planning
The following factors must be considered as part of a patient's therapeutic care plan;
Wandering should only be prevented where there are high level safety risks and theperson does not respond to diversion or distraction and regularly or constantly seeks to leave the designated clinical area.
Delirium should be ruled out or treated – a delirium can be diagnosed using the ‘Confusional Assessment Method' (CAM) (Appendix 3)
Ensure a baseline cognitive assessment has been recorded, in most instances this willbe the ‘Abbreviated Mental Test Score (AMTS)'. A detailed ‘Mini-Mental StateExamination (MMSE); is recommended – (Appendix 4)
A patient ‘Falls Assessment Tool' should be completed on risk admission, repeated and regularly reviewed to identify the patient's risk of falling.
Patients at risk of wandering should be nursed in a high observation area within theWard area where possible & ensure they are placed away from main thoroughfaresand exits and that ward door security alarms or locks are used where fitted.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 41
If the patient is sensitive to over stimulation from noise and light levels, then consider a quieter area but ensure 7.8 is actioned.
Ensure Ward doors are always closed, such a physical barrier can simply preventwandering out of a clinical area.
Check the person is there on a regular basis, the nurse in charge must assess the level of supervision, the patient must be checked at least every 30 minutes as a minimumlevel of supervision, however following risk assessment there maybe times when thepatient requires continuous supervision. The nurse in charge is responsible fordelegating team member/s to be responsible for this duty during a shift.
Ensure the person is wearing a correct identity band and appropriately dressed toensure dignity.
7.10 Provide appropriate signs and cues (words and/or pictures) for orientation purposes
including personal photos & clocks to identify personal bed space and the toilets.
7.11 Check for causes of physical discomfort such as hunger, thirst, pain and desire to go
to the toilet.
7.12 Negotiate with family or volunteers to provide ‘sitter' companionship services during
busy periods for staff or at the times when the wandering usually occurs.
7.13 Ensure the person has an escort for all tests outside of the main care setting and
where possible re-orientate the person on their return.
7.14 Where possible accompany the person whilst they wander/walk, this will reassure the
person making them feel more at home in our environment and less likely to leave. If you can accompany the person for a longer walk so they can leave the ward ordepartment for a short time this can be beneficial.
7.15 If a patient goes missing from the clinical area please refer to a Missing patient policy
for guidelines and actions (Document number 19918).
8. Use of Assistive technology
If the patient has been identified through the Screening tool to have the potential toundertake a more risky type of wandering and or has made an attempt toleave/wander from the ward, then staff can consider the use of assistive technologysuch as pressure pad alarm sensors or electronic location devices. Assistive technologywhere available for use, should only be used in a therapeutic manner, incircumstances in order to maintain patient safety and promote safer wandering.
Where possible the patient's consent should be sought for the use of these devices. If a person lacks capacity to make this decision the practitioner must take intoaccount the views of anyone named by the person as someone to be consulted and/oranyone engaged in caring for the person interested in their welfare. The practitionershould also consider the use of an Independent Mental Capacity Advocate (IMCA)please refer the MCA Policy
Prior to using any equipment the following check list (Appendix 5) must becompleted and filed in the patients notes and reviewed daily.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 42
9. Audit & Review
This policy has been created to allow a simple audit process to be reviewed through Datix and Clinical Governance Teams. When auditing the following outcomes should be measured;
• Reduction in the number of incidents of patients attempting to leave an area
• Reduction in the number of incidents of patients with dementia, who are
wandering, that abscond from the Ward/Department.
• Reduction in the number of falls related incidents
• Use of assistive technology as a therapeutic intervention
• The number of patients with a baseline cognitive assessment – Abbreviated
Mental Test (AMT) completed
• The number of patients with a delirium diagnosis using the Confusion
Assessment Method (CAM)
It is encouraged that if any audit is undertaken using this policy, the author and orthe Directorate of Services for Older People should be informed to advise andimplement audit results into subsequent policy and practice reviews.
Algase, D et al (2001) Impact of cognitive impairment on wandering behaviour. Western Journal of Nursing Research. 23, 3, 283-295.
Alzheimer's Society (2007) Internet source accessed on 31/01/2008;www.alzheimers.org.uk/site/scripts/press_article.php.
Crum, R, M., Anthony, J, C., Bassett, S, S. & Folstein, M, F. (1993) "Population-Based Normsfor the Mini-Mental State Examination by Age and Education Level." Journal AmericanMedical Association. 269:2386-91.
Dewing, J. (2005) Screening for wandering among older persons with dementia. Nursing Older People; 17, 3: page 20 – 24.
Folstein, M, F., Folstein, S, E. & McHugh, P, R. (1975) "Mini-Mental State: A Practical Methodfor Grading Cognitive State for Patients for the Clinician." Journal Psychiatric Research. 12:196-8,
Inouye, S., van Dyck, C., Alessi, C., Balkin, S., Siegal, A. & Horwitz, R. (1990).
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 43
Clarifying confusion: the confusion assessment method. Annals of Internal Medicine,113(12), 941-948.
Jan Dewing 2005 Methods for preventing/responding to wandering in acute care
settings Internet source accessed 31/1/2008
www.wanderingnetwork.co.uk
Jan Dewing 2005 The Dewing Tool for Wandering Screening – permission to use toolgiven by the author.
Claire AgnewJan Dewing Nicolette MorganLara Wealthall
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 44
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 45
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 46
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 47
With Thanks to University Hospitals of Leicester for producing this Resource Pack


34265_text section:34265 text section 14/1/11 10:34 Page 48
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 49
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 50
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 51
A guideline to help all clinical staff identify, diagnose
and manage delirium in hospitalised older people
Adapted from the Royal College of Physicians and
British Geriatrics Society National Guideline on:
The Prevention, Diagnosis and Management of Delirium in Older People, June 2006.
R. Parikh N. Morgan
34265_text section:34265 text section 14/1/11 10:34 Page 52
An AMT score of less than
Why does delirium matter?
•
8/10 is abnormal.
Common – up to 30% of all older medical patients
• Patients with delirium have:
Serial measurements in at
o Higher mortality – twice that of matched controls
risk patients help detect
o An increased length of stay and chance of institutional
the development of
delirium or its resolution.
o Three times the likelihood of developing dementia
On its own the AMT
The following guidelines aim to improve recognition of this
cannot distinguish
complex and challenging condition
between delirium and
What is delirium?
Delirium is characterised by a disturbance of consciousness and a
Delirium is frequently a
change in cognition that develop over a short period of time. The
complication of dementia.
disorder has a tendency to fluctuate during the course of the day,
Distinguishing between
and there is evidence from the history, examination or
dementia and delirium can
investigations that the delirium is a direct consequence of a
be difficult. Collateral
general medical condition, drug withdrawal or intoxication
history from a relative or
carer is usually the most
What factors increase the likelihood of developing
delirium?
The CAM can quickly and
accurately aid the
• Severe illness
diagnosis of delirium.
• Dementia – increases the risk fivefold • Previous episode of delirium • Infection or dehydration at admission •
Hypoactive delirium has a
Visual impairment
poor prognosis – it is really
• Polypharmacy
easy to miss the "quiet"
• Surgery e.g. fractured neck of femur
• Alcohol excess • Renal impairment
Consider if there is anyone
on your ward who could
Identifying those at risk is the first step in trying to prevent or
curtail episodes of delirium
Where can I get more information on delirium?
Our guidelines are based on the Royal College of Physicians and
British Geriatric Society guidance published in 2006:
"The prevention, diagnosis and management of delirium in older
994b-e56f137a22 With Thanks to University Hospitals of Leicester for pr
34265_text section:34265 text section 14/1/11 10:34 Page 53
Identify older patients (over 65 years) with cognitive impairment using the Abbreviated Mental Test
(AMT) score:
Time (to the nearest hour)
Address for recall at the end of test (42 West St)
Name of hospital
Recognition of two people (e.g. doctor, nurse)
Dates of WW2 (1939-1945)
Name of present monarch
Count backwards from 20-1 (also tests attention)
Obtain collateral history
Step 2: Consider delirium in patients with cognitive impairment
Use the Confusion Assessment Method (CAM):
To have a positive CAM result the patient must display:
Presence of acute onset and fluctuating course
Inattention (e.g. 20-1 test with reduced ability to maintain attention or shift attention)
and either
Disorganized thinking (disorganized or incoherent speech)
Altered level of consciousness (usually lethargic or stuporous)
Delirium can be subdivided into three subtypes:
• Hyperactive – increased motor activity with agitation, hallucinations and inappropriate
• Hypoactive – reduced motor activity and lethargy • Mixed
Be alert when talking to patients – delirium is frequently missed!
34265_text section:34265 text section 14/1/11 10:34 Page 54
Step 3: Clinical assessment and investigation
Identify potential causes of delirium using collateral history and
clinical examination.
In addition to standard questioning, the following information
Drugs (particularly tricyclic
should be sought:
antidepressants, opiates,
analgesics, steroids and
• Onset and course of confusion
anti-Parkinsonian
• Drug history including recent changes
medications) are common
• Bladder and bowel function
contributory causes.
• Dietary intake including fluids
Don't forget alcohol and
• Symptoms suggestive of an underlying cause e.g. infection
• Previous intellectual function and functional status
withdrawal as a potential
• Sensory deficits and use of hearing aids/ glasses
Communicate with staff from other disciplines to avoid unnecessary repetition
A full physical examination should be conducted and particularly
Examination
• Conscious level
• Nutritional status
• Evidence of pyrexia
Urinary retention and
• Signs of infection: lungs, urine, abdomen
faecal impaction are often
• Evidence of alcohol abuse or withdrawal
overlooked as potential
• Neurological examination
• Signs of urinary retention or faecal impaction
The following investigations are almost always indicated to help
identify the cause:
Investigations
• FBC, U&E, LFT, Bone, CRP
• Glucose
When is CT scanning
• CXR • Pulse oximetry
Indications are:
• Urinalysis (+/- culture)
• Focal neurology
• Blood cultures
• Confusion post head
Consider also depending on history and examination findings:
• Confusion after a fall
• Evidence of raised ICP
• Lumbar Puncture • B12, folate and TFTs – if pre-existing dementia suspected
34265_text section:34265 text section 14/1/11 10:34 Page 55
Step 4: Management
Identify and treat the underlying cause:
Treatment of Underlying Cause
• Withdraw incriminated drugs
• Correct biochemical derangements
The most important action
for the management of
• If there is a high likelihood of infection commence
antibiotics promptly. Use the antimicrobial web pages to
help select an appropriate agent.
identification and
treatment of the
• Administer parenteral thiamine when alcohol abuse or
underlying cause!!
under-nutrition is apparent
Management should also focus on symptomatic improvement:
Environmental
• Appropriate lighting for the time of day
• Cues to improve orientation
• Familiar objects from home
• Catheters (where
• Glasses and hearing aids in working order
• Medication review including adequate analgesia
• Constipation
• Encourage mobility
• Inter ward transfers
• Promote nutrition
• Irritating and
• Avoid dehydration and constipation
intrusive noise e.g.
• Involve relatives and carers
Wandering
• Provide close observation within a safe and reasonably
closed environment
• Act in patient's best interests to keep them safe
Remember, there may be
• Ask relatives to help offering meaningful distractions
an easily remedied cause
• Use drug treatment only as the final option
of wandering – pain, thirst
or need for the toilet.
Dealing with false ideas
Try the following: • Tactfully disagree (if the topic is not sensitive)
Confused and rambling
• Change the subject
speech is common in
• Acknowledge the expressed feelings – ignore the content
delirium. It is usually
preferable not to agree
but respond to the feelings
Repeating the AMT will help you
gauge improvement!!
34265_text section:34265 text section 14/1/11 10:34 Page 56
Medication
The main aim of drug treatment is to calm or manage dangerous
or distressing behavioural disturbance e.g. agitation and
Pharmacological options may be necessary in the following
All sedatives may cause
delirium. Use them
• To allow essential investigations or treatment to take
• To prevent the patient endangering themselves or others
Reflect on how you have
• To relieve distress in a highly agitated or hallucinating
used, or seen, sedatives
used in the past.
Which drug should I choose?
Haloperidol is the preferred option:
• Dosage: 0.5mg orally – can be given up to two hourly
o Maximum dose: 5mg in 24 hours
Avoid Haloperidol in
• If the oral route is unavailable and symptoms necessitate:
patients with dementia
o Try: 1-2mg IM (maximum of 5mg in 24 hours)
with Lewy bodies and
those with Parkinson's
Lorazepam is an alternative:
disease. Ask a
• Dosage: 0.5-1mg orally – can be given up to two hourly
psychiatrist, geratician or
o Maximum dose: 3mg in 24 hours
neurologist for advice. In
• If the oral route is unavailable and symptoms necessitate:
an emergency use
o Try: 0.5-1.0mg IV or IM (dilute to 2ml with normal
Lorazepam
saline) up to a maximum of 3mg in 24 hours
Sedation is only a small part of management and should be
kept to a minimum!!
If psychotropic drugs are prescribed, the prescription should be
reviewed regularly and discontinued as soon as possible. Aim to
tail off sedation after 24-48 hours.
For delirium secondary to
One-to-one care of the patient is often required and should be
alcohol withdrawal
provided while the dose of psychotropic medication is titrated
chlordiazepoxide (in a
upward in a controlled and safe manner.
reducing dose) is
34265_text section:34265 text section 14/1/11 10:34 Page 57
How long does delirium last?
Delirium can persist after treatment of the underlying cause:
• The duration of the illness may range from a few days to
Delirium can take up to
• It is important to explain to the patient and carers that
resolution may take time
six months to resolve
Delirium is
• Common
• Associated with an increased morbidity and mortality
• Characterised by acute changes and fluctuation in
How can you personally
translate this guidance
At admission
into practice?
• Use the AMT and CAM to help make the diagnosis • Remember:
o Collateral history is vital o Hypoactive delirium is really easy to miss!!
Clinical Assessment and Investigation
• Try to identify potential causes using collateral history and
clinical examination
• Specifically consider:
o Dehydration, infection, drugs, urinary retention
and faecal impaction
Management
• Treat the underlying cause
• Attend to the ward environment
information on how to
• Closely supervise those who wander within a safe and
manage the problems
reasonably closed environment
experienced by older
• Drugs to calm patients should be kept to a minimum
If you do, why not visit
Want to know more?
the British Geriatric
Our guidelines are based on the Royal College of Physicians
Society website –
and British Geriatric Society guidance published in 2006:
"The prevention, diagnosis and management of delirium in
older people" - www.rcplondon.ac.uk/pubs/contents/
34265_text section:34265 text section 14/1/11 10:34 Page 58
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 59
SECTION 6
Further information and advice
The following organisations may be able to provide support and advice to carers and
people with dementia;
Alzheimer's Society
• Support and advice for people with dementia and their carers, services include;
• Carer Support
• Carer Support Groups
• Information & Advice
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 60
Alzheimer's Society (National)
National helpline and helpful web resource for information and support for people with
dementia, relatives and professionals:
Telephone: 02074233500 Email: [email protected]
Helpline: 0845 300 0336 (8.30am to 6.30pm Monday to Friday)
www.alzheimers.org.uk
Trent Dementia Services Development Centre
Part of a network of centres offering advice, training, and service development for all
service providers. Registered Charity no 1109855
Telephone: 0116 257 5017
[email protected] or www.trentdsdc.org.uk
The UK's leading care and research charity for people with dementia, their families and
Bradford Dementia Group. Provide teaching, education and research in dementia care and
home to Dementia Care Mapping
The DSDC works to spread research and good practice about home and hospital care for
people with any type of dementia including Alzheimer's disease, multi-infarct dementia,
Lewy body dementia, vascular dementia and alcohol-related dementia throughout the
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 61
Kitwood, T (1997) Dementia Reconsidered. Open University Press
Cantley, C (2001) A Handbook of Dementia Care. Open University Press.
Archibald, C (2003) People with dementia in acute hospital settings: A practice guide for
registered nurses. The Dementia Services Development Centre. Stirling.
Cheston, R and Bender, M (2003) Understanding Dementia: The Man with the Worried
Eyes. Jessica Kingsley.
Stokes, G (2005) Challenging Behaviour in Dementia: A person centred approach.
Bryden, C (2005) Dancing with Dementia: My story living positively with dementia
Brooker, D (2007) Person centred dementia care: making services better, Bradford
Dementia Group Good Practice Guidelines.
Stokes, G (2008) And Still the Music Plays: Stories of people with dementia
Department of Health (2009) Living well with dementia: A National Dementia Strategy,
London, Department of Health.
Alzheimer's Society (2009) Counting the cost; caring for people with dementia on hospital
wards, London, Alzheimer's Society.
NHS Confederation (2010) Acute Awareness Improving hospital care for people with
dementia, London, NHS Confederation.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
34265_text section:34265 text section 14/1/11 10:34 Page 62
Dementia quality standard (NICE) Guidelines
People with dementia receive care from staff appropriately trained in dementiacare.
People with suspected dementia are referred to a memory assessment servicespecialising in the diagnosis and initial management of dementia.
People newly diagnosed with dementia and/or their carers receive written andverbal information about their condition, treatment and the support options intheir local area.
People with dementia have an assessment and an ongoing personalised careplan, agreed across health and social care that identifies a named carecoordinator and addresses their individual needs.
People with dementia, while they have capacity, have the opportunity to discussand make decisions, together with their carer/s, about the use of: advancestatements, advance decisions to refuse treatment, Lasting Power of Attorney,Preferred Priorities of Care.
Carers of people with dementia are offered an assessment of emotional,psychological and social needs and, if accepted, receive tailored interventions identified by acare plan to address those needs.
People with dementia who develop non-cognitive symptoms that cause themsignificant distress, or who develop behaviour that challenges, are offered anassessment at an early opportunity to establish generating and aggravatingfactors. Interventions to improve such behaviour or distress should be recorded in their care plan.
People with suspected or known dementia using acute and general hospitalinpatient services or emergency departments have access to a liaison service thatspecialises in the diagnosis and management of dementia and older people´smental health.
People in the later stages of dementia are assessed by primary care teams toidentify and plan their palliative care needs.
Carers of people with dementia have access to a comprehensive range ofrespite/short-break services that meet the needs of both the carer and theperson with dementia.
With Thanks to University Hospitals of Leicester for producing this Resource Pack
Source: http://www.thinklocalactpersonal.org.uk/_assets/Resources/Personalisation/EastMidlands/Dementia/Acute_Hospital_Resource_Pack_text_section.pdf
Redacción y Diseño: María Luisa Preinfalk Sabes que es la violencia contra Las Mujeres Sabes que es la violencia contra Violencia Es cualquier acción basada en su género, que cause muerte, daño o sufrimiento físico, sexual o psicológico a la mujer
THE FAULT IN OUR STARS Scott Neustadter & Michael H. Weber Based on the novel by John Green FOX 2000 PICTURES FINAL SHOOTING SCRIPT 10201 W. Pico Blvd. Los Angeles, CA 90035 Revisions Green – August 27, 2013 Yellow – August 30, 2013 Goldenrod – September 13, 2013 Salmon – September 18, 2013 2nd Blue – September 23, 2013